5 results in Exploration of Asthma & Allergy
Latest
Sort by :
- Latest
- Most Viewed
- Most Downloaded
- Most Cited
Open Access
Mini Review
Small airway dysfunction and impulse oscillometry in adult patients with asthma: recent findings
Marcello Cottini ... Alvise Berti
Published: October 31, 2023 Explor Asthma Allergy. 2023;1:163–173

Open Access
Review
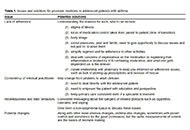
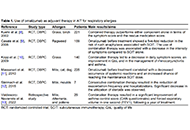
Precision medicine: how to approach the adolescent asthmatic
Alan Kaplan
Published: October 31, 2023 Explor Asthma Allergy. 2023;1:153–162
This article belongs to the special issue Precision Medicine in Allergy and Rhinology
Open Access
Original Article
Safety of 2-day rush induction protocol in sublingual immunotherapy with Pru p 3
Maria Inês T. Silva ... Célia Costa
Published: October 31, 2023 Explor Asthma Allergy. 2023;1:142–152

Open Access
Review
Biologic drugs and allergen immunotherapy: potential allies
Palma Carlucci ... Danilo Di Bona
Published: October 20, 2023 Explor Asthma Allergy. 2023;1:126–141
This article belongs to the special issue The Era of Biologics in Allergy
Open Access
Review
Impact of the GINA asthma guidelines 2019 revolution on local asthma guidelines and challenges: special attention to the GCC countries
Riyad Allehebi, Hamdan AL-Jahdali
Published: October 10, 2023 Explor Asthma Allergy. 2023;1:115–125
This article belongs to the special issue The Global Picture of Asthma after Guideline Changes and the COVID Pandemics

Journal Information
 Previous
Previous