Abstract
Numerous methods for functional diagnostics of nasal obstruction provide various information on nasal airway resistance and may aim to replace physically based methods by so-called simplifications or solely on subjective score systems. This may lead to nonsatisfying results in nasal surgery and prolonged postoperative care. An interdisciplinary analysis of contemporary methods for measurement was the task of the German-Austrian research program “Rhinodiagnost”. This review is intended to discuss basic and wide-spread errors playing a significant role during daily practice and proposes a step program for functional rhinological diagnostics with some modifications to be applied in case of allergic nasal disease. With regard to the content of “position paper on the standardization of nasal allergen challenges (2018)” of the European Academy of Allergology and Clinical Immunology (EAACI) and the results of the consensus conference of Riga in 2016, the differences between of “classic” and 4-phase-rhinomanometry (4PR) and their differences are clarified. The parameters of logarithmic effective resistance (LReff) allow a classification of the obstruction obtained during 36,500 measurements which are correlated to the subjective sensing of obstruction. The classification can be adapted for age and size and is valid for the Caucasian and Chinese populations.
Keywords
Nasal functional tests, nasal obstruction, allergy, rhinomanometry, nasal challengeIntroduction
Nasal obstruction is a typical symptom of allergic rhinitis amongst other causes such as anatomic variants of the nasal skeleton, acute rhinitis or rhinosinusitis, tumors, etc. Moreover, congested noses are one of the most frequent complaints in the practice of an otorhinolaryngologist. Septoplasties and septorhinoplasty as well as surgery of the paranasal sinuses belong to the most frequently performed surgical procedures of an ear, nose, and throat (ENT)-specialist and are taught to trainees commonly at the beginning of the career.
The estimated number of nasal surgeries in Germany exceeds 100 per day, in the USA the number per year exceeds 1 million. Following non-statistic publications in newspapers or public journals, the percentage of “non-successful” surgeries is indicated between 20% and 40%. Reliable data are missing. Persistent obstruction or further symptoms such as impaired smell or the so-called “empty nose syndrome” implicate revision surgery or long-lasting postoperative care. To diminish the number of unnecessary surgeries and to establish validated methods for preoperative and postoperative diagnostics, the International Standardization Committee on the Objective Assessment of the Nasal Airway (ISCOANA) published a new standard in 2018 [1]. At the same time, the German-Austrian research project Rhinodiagnost (www.rhinodiagnost.eu) has been started where most of the presently applied diagnostic methods for physical diagnosis in rhinology have been analyzed for their methodological and technical correctness.
Wide-spread uncertainties concerning the diagnostics of nasal obstruction
The most wide-spread errors because of missing or not physically based objective diagnostics are the following:
The human eye used for rhinoscopy alone cannot estimate the degree of nasal resistance because the resistance depends exponentially on the diameter. The failure increases remarkably if two subsequent obstacles determine nasal resistance.
The nose is not a rigid anatomic structure but a “Starling resistor” as the entire respiration tract, which means that the resistance increases with the air flux due to the elastic properties of the lateral nasal wall.
The so-called nasal valve is one physiological unit. A differentiation between external and internal valves is not corresponded with real physiology.
Rhinomanometry is the determination of the intranasal flow (flux) and the narino-choanal differential pressure and the calculation of the nasal resistance in a physically correct way. The graphical and numerical results of 4-phase-rhinomanometry (4PR) also show the influence of the elasticity of the lateral nasal wall by graphic “loops” in the inspiratory part. The elastic behavior of the nose must be considered when planning surgical procedures. Changing the anatomy or the mechanical properties of the lateral nasal wall by scars or implants has a huge but mostly underestimated effect on ventilatory function.
Acoustic rhinometry measures anatomic dimensions in the anterior part of the nose only and cannot be considered as a functional investigation. The unilateral or bilateral resistance of the nasal airflow can only be determined by measuring the flow and narino-choanal differential pressure with rhinomanometry, where logarithmic parameters must be used to get a correlation with the sensing of obstruction.
Peak nasal inspiratory flow (PNIF) does not consider the elasticity of the nose and is an erroneous “simplified” method with deceptive appearances!
Subjective scores such as visual analogue scale (VAS), sino-nasal outcome test (SNOT) score, total nasal symptom score (TNSS), or Nasal Obstruction Symptom Evaluation (NOSE) score should not solely determine the indication of surgery or conservative treatments with intended irreversible results. Some patients do not know the feeling of a “normal” nose, others cannot feel the just noticeable difference (JND) of obstruction or the timeline of obstruction in different body positions. The subjective main symptoms are obstruction or reduced smelling. We recommend recording the subjective feeling of obstruction on a simple VAS after rhinomanometric measurement on each side before and after decongestion. This informs also about the part of mucosal and skeletal obstruction with different treatment options and can be used before and after treatment to see its effect.
The subjective sense of obstruction is a combination of the feeling of power, needed for inspiration, of the temperature gradient generated by the air stream, and probably also of wall-shear-stress. All these sensations follow the basic law of Weber-Fechner in psychophysiology from the 19th century. Between sensing and intensity, a logarithmic correlation exists. While the intensity increases in exponential order, the power of sensing increases arithmetically. A related term is the “just noticeable difference”. A widening of the nasal diameter at a critical area from 3 mm2 to 4 mm2 is recognized by the patient as a big improvement, extension of the diameter from 6–8 mm2 does not release the feeling of a “better nose”. This relation was never considered in rhinology up to the classification of obstruction by 4PR [2].
Since it is necessary to deduce the indication and the extent of surgery as well as of conservative treatment from objective findings with a clear relation to breathing physiology, the following order was proposed as a follow-up of the “Rhinodiagnost” program.
A step program of functional rhinological diagnostic
Functional Rhinodiagnostic should include contemporary methods as suggested by the “Rhinodiagnost” research program in its theoretical, technical, and clinical details. In the future, the diagnostic workflow can be extended by additional steps, considering elastic compartments or novel analytic methods testing the nasal mucosa. Photonic methods will allow detailed analysis of the mucosa, including the visualization of the activity of the ciliated epithelium. Such methods are, for instance, optical coherence tomography (OCT) and Raman spectroscopy. The presently applicable methods can be subordered in a practically relevant step program (Figure 1).
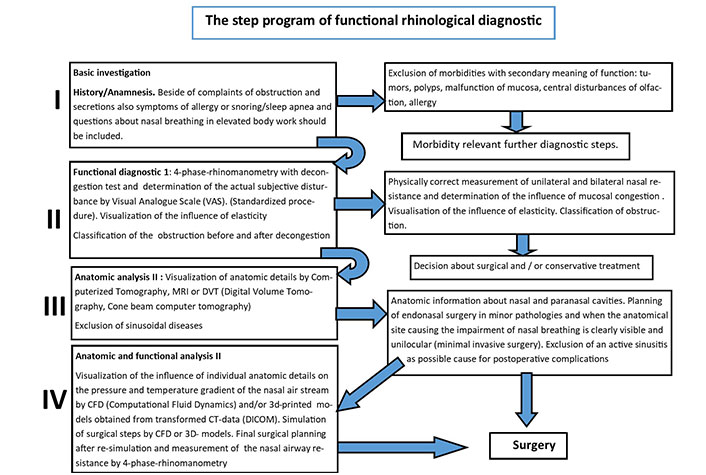
The step program of maximal functional rhinological diagnostic. CT: computerized tomography; DVT: digital volume tomography; MRI: magnetic resonance imaging; CFD: computational fluid dynamics; 3D: three-dimensional; DICOM: digital imaging and communication in medicine
Note. Adapted from “Rhinodiagnost project,” by Vogt K. [cited 2022 Nov 18]. Available from: https://rhinodiagnost.eu/projekt-info/
The steps as depicted in Figure 1 need some explanations for details:
Step I: Basic investigation with history taking and clinical investigation/inspection, which may include specific procedures like taking specimens for histological investigation of suspicious masses.
Step II: 4PR for retrieval of quantitative information on obstruction, including separate information on the mucosal portion. The logarithmic effective resistance (LReff) and logarithmic vertex resistance (LVR) are determined for inspiration and expiration prior to and after decongestion. The total nasal resistance can be calculated with good approximation by the rule of Kirchhoff for parallel electrical resistances. Calculated results differ from the measured results by posterior rhinomanometry but are more reliable because frequently patients cannot keep the tongue immotile during measurements. Side-specific results of 4PR are divided into five obstruction classes, defined through 36,000 preclinical measurements in Caucasian individuals. Moreover, the shape of the resulting curves provides information on the influence of elastic structures (Starling resistor). Finally, a VAS is included for documentation of actual individual subjective complaints.
By changing the body position the influence on nasal breathing during sleep can be determined. Statistical data for the influence of body position on LReff and LVR are available as well as data showing the important relation between nasal resistance and acceptance of continuous positive airway pressure (CPAP) [2]. The role of the nose in snoring and obstructive sleep apnea syndrome (OSAS) is doubtless.
Step III: Anatomic analysis through radiologic procedures—CT, DVT (cone beam tomography), or MRI. Prior to detailed surgical planning, the present morphology of the nasal cavity and the paranasal sinuses need to be anticipated, since the shape of the main nasal channel may contribute to results and may also cause postoperative complications such as infections.
Radiation exposure of modern DVT devices is clearly reduced when compared to CT or classic X-ray. The exposure dose of a CT of the paranasal sinuses is 2 mSv. This corresponds to a natural environmental radiation exposure of eight months.
Step IV: Additionally, to the determination of overall and side-specific aerodynamic properties, two additional procedures may be performed in order to achieve further information on morphologic and functional consequences through present structures.
Using data generated through imaging modalities DICOM data it is possible to simulate and visualize the patient-specific air stream and locations with special influence on the pressure or resistance as well as on the temperature gradient along the air stream. These methods are well known as “computational fluid dynamics” and allow a precise topical diagnosis, which may be used as a basis for surgical planning [3]. CFD is not yet a standardized procedure in rhinology. In cooperation between information technology (IT)-specialists and surgeons, the primary structural analysis may be followed by a simulation of surgical steps and a re-analysis to simulate the intended functional effect of surgery. The cooperation between rhinologists and IT-specialists and a new Society for CFD of the Nose and Airway (SCONA) as well as the introduction of artificial intelligence will contribute to a future routine method (Figure 2).
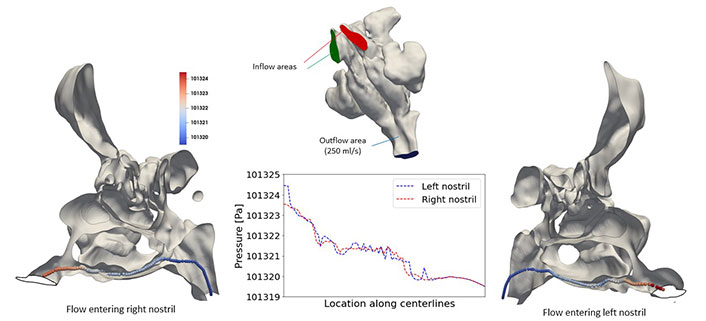
Example for a CFD-simulation of the nasal air stream [Mario Rüttgers, Rheinisch-Westfälische Technische Hochschule (RWTH), Aachen/Germany]
Note. Reprinted from “Contemporary diagnostic of nasal obstruction - basic errors and how to avoid them,” by Vogt K, Roesch S, Bauer SM, Neumaier P. Ann Otolaryngol Rhinol. 2022;9:1297 (https://www.jscimedcentral.com/public/assets/articles/otolaryngology-9-1297.pdf). © 2022 Vogt K, et al.
A second procedure of interest is a method, increasingly used in industry: 3D printing. DICOM data generated by CT or DVT can be transformed into the digital format of “stereolithography (STL)”-files. These files can be adapted by simple standard imaging procedures in order to remove parts of minor interest and to slice the model in a vertical direction in 4–6 layers [4]. These layers provide not only an outstanding insight into the structures of the nose but the composed printed model can also be measured by 4PR. For didactic purposes and to anticipate the effect of surgical steps as planned for the upcoming real surgery, intended steps can be performed in a real model and instantaneously measured by 4PR. The application of 3D printing to date is restricted to specific cases and not during clinical routine. However, resulting uncommon visual insights into the nasal cavity and the sinuses may support surgical planning (Figure 3).
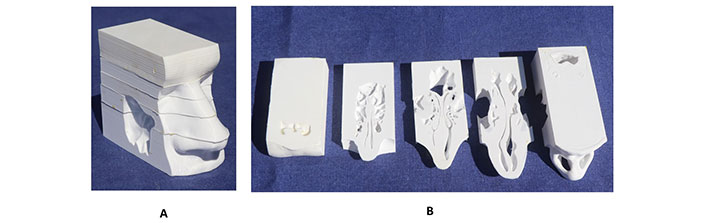
Example of 3D print of a nose with septal deviation. A: Composed slices; B: inferior sides of slices seen from below. Left side entrance of frontal sinus, right side nares with transition to nasopharynx
Note. Reprinted from “Contemporary diagnostic of nasal obstruction - basic errors and how to avoid them,” by Vogt K, Roesch S, Bauer SM, Neumaier P. Ann Otolaryngol Rhinol. 2022;9:1297 (https://www.jscimedcentral.com/public/assets/articles/otolaryngology-9-1297.pdf). © 2022 Vogt K, et al.
Modifications for obstruction diagnosis in allergology
Relevant diagnostic steps in nasal allergy or allergic rhinitis are quite different. Prick-tests, serological investigations, and documentation of itching, sneezing, or nasal discharge may determine an adequate treatment plan in particular in seasonal allergic rhinitis. However, for the identification of allergens in perennial allergic rhinitis, sometimes combined with asthma, a measurement of obstruction is of fundamental interest.
In 2018 the European Academy of Allergology and Clinical Immunology (EAACI) published a “position paper on the standardization of nasal allergen challenges” evaluating the international literature as well as the available techniques to determine quantitatively the influence of allergens on nasal mucosa [5]. Even when following these comprehensive recommendations of experienced scientists, there are missing methodic details or the physical background. Also, the results of recent research and clinical experience should be considered, since the perspectives of ENT-specialists and allergologists may sometimes be diverse.
The EAACI consensus paper nominated PNIF, acoustic rhinometry, active anterior rhinomanometry, and 4PR as methods of choice for objective measurement. Measurement of nasal obstruction means measurement of the nasal airway resistance, which is in the first line determined by the cross-sectional area of the streaming body and only in a minor extent by its length. The law of Hagen-Poiseuille can be applied as a good approximation:
With the resistance R, the length l, and the radius r. Reduction of the radius to the half means a 16-fold increase of the resistance.
In addition, the elasticity of the lateral nasal wall has an influence on airway resistance. The nose is not a rigid streaming body but a so-called Starling resistor, which changes its shape by the volume stream (flux). The nasal valve follows during forced inspiration the “paradoxon” of Bernouilli like an airplane and moves inwards, reducing the cross-sectional area. The intended forced inspiration in PNIF releases constantly this effect and produces erroneous information about the nasal airway resistance with high repeatability of non-usable results.
Acoustic rhinometry determines the anatomic parameters of the anterior cross-sectional area only, but in allergology, detailed information along the total length of the turbinates is needed.
“Classic” active anterior rhinomanometry, as well as 4PR, are reliable methods to determine nasal resistance within the framework of allergology, but the diagnostic information of the 4PR as recommended by the ISCOANA is much higher [6]. The four phases of 4PR are the ascending and descending phases of the air stream in inspiration and expiration. Instead of measuring the flow at 150 Pa as a 1-point method in a part of the breathing wave, which can be different during every breath, 4PR determines the “effective” resistances by root mean squares (RMS) and averages in this way the flow and the narino-choanal pressure difference of three complete breathes with some thousand measurement points (Figure 4). “Effective resistances” are calculated in electric engineering as a standard procedure.
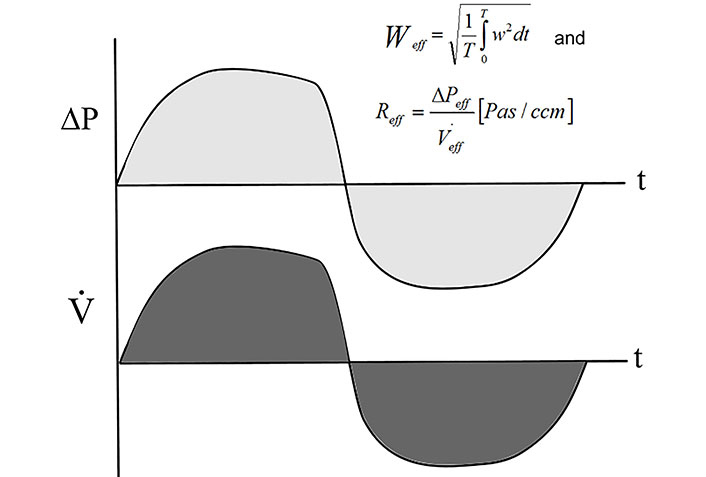
Calculation of effective resistance of an averaged breath
Note. Reprinted from “Four-phase rhinomanometry: a multicentric retrospective analysis of 36,563 clinical measurements,” by Vogt K, Wernecke KD, Behrbohm H, Gubisch W, Argale M. Eur Arch Otorhinolaryngol. 2016;273:1185–98 (https://link.springer.com/article/10.1007/s00405-015-3723-5). CC BY.
These effective resistances can be calculated for inspiration, expiration, or for the entire breath. Applying Kirchhoff’s rule for the calculation of parallel electric resistances the total nasal resistance can be calculated (Figure 2).
For rhinological purposes, the pressure-flow-relation is depicted in a standardized xy-diagram (Figure 5), applied in both, “classic” and 4PR.
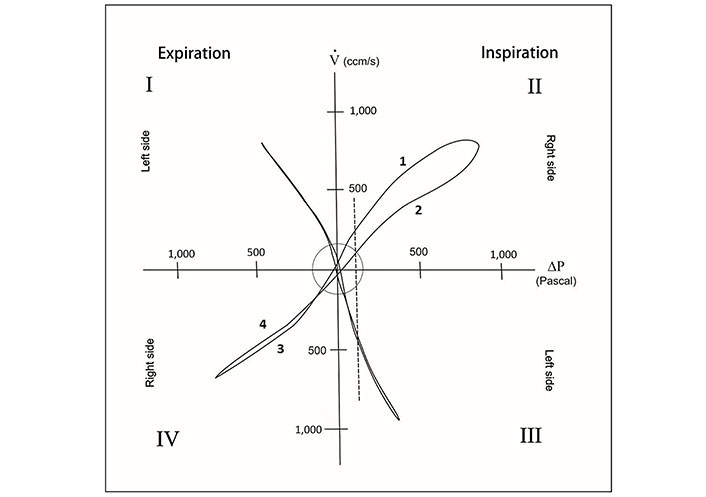
Standard pressure/flow xy-diagram of bilateral 4PR. Phases 1–4 for the right side measurement are indicated.
In the graphic display (Figure 5, quadrant II) a loop is visible during inspiration. During accelerating inspiration (phase 1) the lateral nasal wall is being drawn towards the septum and reduces the cross-sectional area for the airflow. During phase 2 the flow at the same pressure level is lower. Loops do not appear in graphs of “classic” rhinomanometry as in the example of Figure 6.
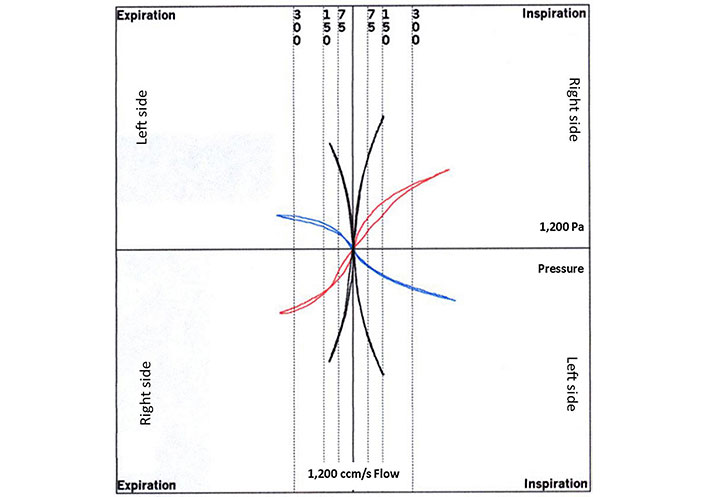
“Classic” rhinomanometry graph of a decongestion test of a patient allergic to house dust mites (red and blue before decongestion, black after decongestion)
The validity of 4PR for the visualization of the elasticity of the lateral wall has been recently confirmed in a clinical study [7]. Moreover, this phenomenon could be confirmed by the application of optical distance sensors and strain gauges. The onset of a motion inwards already starts at the beginning of a breath during low differential pressure and flow rates [8].
In nasal allergy, the behavior of the nasal valve is of minor interest since the obstruction as a symptom of allergy or in nasal challenges is determined mainly by the turbinates and their status of the mucosa concerning swelling. This means that nasal obstruction caused by allergy should be evaluated during expiration instead of inspiration, since the outward direction of the air stream does not force the Bernoulli-effect.
Myriad papers are reporting on missing correlations between objective measurement results and the individual subjective feeling of nasal obstruction. No publication considers the fundamental laws of psychophysics [9]. The sense of obstruction follows the increased power for breathing, the alteration of temperature in the nose, and probably also the wall-shear-stress. The introduction of logarithmic parameters into the rhinological diagnostic follows simply the laws of Weber (1834) and Fechner (1860), later merged as Weber-Fechner’s law: the relationship between stimulus and perception is logarithmic. Every otorhinolaryngologist knows the logarithmic decibel-scale for hearing. For the feeling of power, Weber found that the “just noticeable difference” of weights of a hand-held item is about 5%, which can also be applied to the power necessary for breathing.
During the development of 4PR, the subjective perception of obstruction was evaluated with the help of a VAS. In a first study, including 1,850 measurements, after the logarithmic transformation of the measured effective resistances a high statistical correlation between the LReffs and the sensing of impaired nasal breathing was found [10]. A following multicentric study with 36,500 measurements obtained from six clinical units allowed a classification of the unilateral and bilateral nasal obstruction in five classes [10], as shown in Table 1.
Clinical classification of unilateral and bilateral LReff
| Class | Unilateral LReff | Calculated bilateral LReff (total) | ||
|---|---|---|---|---|
| Untreated | After decongestion | Untreated | After decongestion | |
| 1 (0–19%) | < 0.71 | < 0.63 | < 0.42 | < 0.36 |
| 2 (20–39%) | 0.71–0.89 | 0.63–0.78 | 0.42–0.57 | 0.36–0.47 |
| 3 (40–59%) | 0.89–1.08 | 0.78–0.94 | 0.57–0.70 | 0.48–0.59 |
| 4 (60–79%) | 1.09–1.35 | 0.94–1.18 | 0.70–0.90 | 0.59–0.76 |
| 5 (80–100%) | > 1.35 | > 1.18 | > 0.90 | > 0.76 |
Note. Adapted from “Contemporary diagnostic of nasal obstruction - basic errors and how to avoid them,” by Vogt K, Roesch S, Bauer SM, Neumaier P. Ann Otolaryngol Rhinol. 2022;9:1297 (https://www.jscimedcentral.com/public/assets/articles/otolaryngology-9-1297.pdf). © 2022 Vogt K, et al.
For better convenience of the LReff data in clinical diagnostic programs, the logarithm of the 10-fold effective resistance was introduced. As an example, the LReff in inspiration is noted as:
The important rhinomanometric decongestion test should be performed 10 min after the conventional application of imidazoline or oxymetazoline (1 mg/mL) as a spray.
Following the EAACI position paper, the indication of a nasal challenge is in the first line given by a positive decongestion test [5].
The EAACI position paper as mentioned above evaluates in “classic” rhinomanometry a flow decrease ≥ 40% at 150 Pa as clearly positive and ≥ 20% as moderately positive. For 4PR an increase of ≥ 40% in LReff is seen as clearly positive and ≥ 20% as moderately positive. This is comparable to 1 or 2 classes as noted in Table 1 and comparable with the results of the decongestion tests.
For correct and reproducible rhinomanometric measurements it is important to incorporate physiological variations of the nasal resistance:
Age: Values for resistance in Table 1 are equal in men and women and valid for age > 20 years. They are regarded higher in children and teens. Relationships among nasal resistance, age, and anthropometric parameters of the nose during growth are available [11].
Physical exercise: This represents a reliable method for decongesting the nose: rhinomanometry can therefore result in better than normal results, up to an hour after physical work.
Body position: Rhinomanometric measurements as well as nasal challenge tests should be performed in the upright sitting position. The influence of body position is very important to analyze the role of nasal breathing during sleep. The nasal resistance in the supine position is remarkably higher. Raising the upper body by 30° from the horizontal plane can reduce it [2].
Temperature: The recommended room temperature during rhinomanometry should be 18°–25°C. The influence of temperature varies individually and is not predictable. Studies should be performed in equal room conditions.
Drugs: Drugs may have an influence on nasal breathing. Any nose drops should be avoided for < 24 h before measurement.
The fixation of the tube for measuring the narino-choanal pressure difference is of eminent importance for correct measurements. The method of choice is its fixation with the help of an elastic tape. The usage of preformed plugs deforms the nasal entry of both sides and may distort the numeric results of rhinomanometry.
In another study, only minimal statistical differences in the effective resistance between the Caucasian and Chinese populations have been found. Thus, the classification in Table 1 is also valid for the Chinese population [6].
4PR is also used for the validation of anti-allergic drugs. The “classic” parameters have been used already with 4PR in 2004 by Meltzer et al. [12] for the clinical testing and evaluation of desloratadine in seasonal allergic rhinitis. In that study, the flow in 150 Pa has been evaluated in the “constant” phases 1 and 4 avoiding the influence of elasticity. At this time the “effective values” have been still under development.
Logarithmic scaling is recommended to evaluate surgical procedures through preoperative and postoperative tests. In allergology, the surgical procedure of thermic reduction of the turbinates can bridge the gap between the beginning of immunotherapy and the expected decongestive effect or reduce the blood flow of the turbinates in vasomotor rhinitis [13]. The indication for a thermo-ablation is given if the decongestion test shows a decrease in the logarithmic resistance of ≥ 20%. For the thermic reduction, radiofrequency ablation with monopolar or bipolar electrodes instead of laser or “coblation” is preferable as a practical consequence of comprehensive experimental results, which showed that radiofrequency reduces only the vascularization but preserves the mucosal surface [14].
VAS-test in nasal allergy
The documentation of subjective feeling of obstruction should be documented in a simple VAS together with the rhinomanometric results separately for the right and left side and before and after decongestion. This simple procedure included in the results of 4PR or “classic” rhinomanometry measurements records the subjective problems of the patient separately on both sides during two different states of congestion (Figure 7).
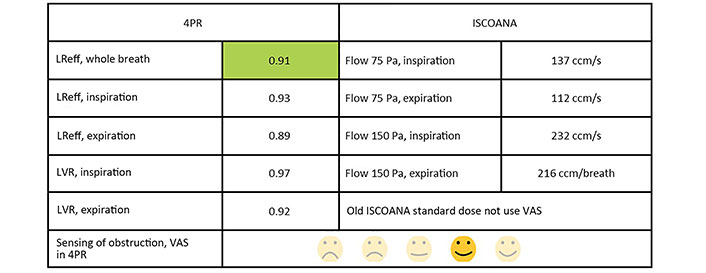
VAS was included in the results of a unilateral measurement of a non-obstructed nasal side by 4PR. The green color is the best classification of 4PR obstruction. The ISCOANA columns show, in addition, the standard results of “classic” rhinomanometry. The “smileys” are numerically recorded for intended statistical evaluation.
Conclusions
Obstruction is a major symptom of allergic rhinitis. Its degree should be determined by reliable methods with a proofed biophysical and statistical background. Following the updated recommendations of the ISCOANA and the evaluation of different methods within the “Rhinodiagnost” research program, 4PR should be used as the preferred method to measure nasal airway resistance. The results can be categorized in a statistically relevant classification. The logarithmically transformed “effective resistances” can be measured in inspiration and expiration side-specifically as well as for the total nose. These parameters match with the subjective sensing of obstruction. For nasal allergen challenges, it is recommended to take into account the guidelines of the position paper of the EAACI.
Abbreviations
| 3D: | three-dimensional |
| 4PR: | 4-phase-rhinomanometry |
| CFD: | computational fluid dynamics |
| CT: | computerized tomography |
| DICOM: | digital imaging and communication in medicine |
| DVT: | digital volume tomography |
| EAACI: | European Academy of Allergology and Clinical Immunology |
| ISCOANA: | International Standardization Committee on the Objective Assessment of the Nasal Airway |
| LReff: | logarithmic effective resistance |
| LVR: | logarithmic vertex resistance |
| PNIF: | peak nasal inspiratory flow |
| VAS: | visual analogue scale |
Declarations
Author contributions
KV and SR equally contributed to: Conceptualization, Writing—original draft, Writing—review & editing, Resources.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2023.