Abstract
Lettuce allergy is uncommon and usually attributed to lipid transfer protein (LTP) sensitization. Most LTP-sensitized patients present with heterogeneous symptoms not only to lettuce, but to a large number of other foods and pollen allergens, including peaches, apples, Platanus, and mugwort, with peach LTP being considered as the primary sensitizer. The case of a medical student with a history of lettuce allergy investigated by skin prick tests (SPTs) and oral food challenge (OFC) is presented in this report. SPTs showed sensitization exclusively to lettuce and not to any other known cross-reacting allergens, which contrasts with previous literature and highlights the uniqueness of this case. During OFC, the patient developed generalized symptoms including abdominal discomfort, bilateral tinnitus, facial flushing, generalized itching, and urticaria. No cardiopulmonary compromise was observed at the time, and the reaction was managed with oral antihistamines. More sophisticated molecular analysis is required to identify the patient’s sensitization profile; however, SPTs and OFCs remain the most practical clinical approach. Lettuce allergy deserves further attention and investigation.
Keywords
Food allergy, lettuce allergy, lipid transfer protein, skin prick tests, oral food challengeIntroduction
Whilst attending a lecture on allergic diseases at Limassol General Hospital, students from the University of Nicosia were given the opportunity to discuss their own experiences with allergies. One of our male peers opened up regarding his history of lettuce allergy. The case seemed outlandish and even provoked laughter among the group as none of us could believe somebody to be allergic to lettuce. However, giving our classmate the benefit of the doubt and after obtaining consent, we decided to further investigate his possible lettuce allergy in the hospital the following day, with skin prick tests (SPTs) and an oral food challenge (OFC).
Herein, this paper reports a case of isolated lettuce allergy in a 22-year-old medical student, from whom informed consent to publish the details was obtained. The case is followed by a short literature review on lettuce allergy.
Case report
A 22-year-old male experienced his first allergic reaction to lettuce at the age of 8. About 30 min after ingesting a salad, containing lettuce and other vegetables, he experienced nausea, abdominal cramps, generalized itching, and urticaria. No cardiopulmonary compromise was observed at the time. His symptoms resolved with the administration of an oral antihistamine, as recommended by his pediatrician over the phone.
Lettuce was not considered as the trigger, however, after a few days, he developed a similar reaction when consuming lettuce, leading to his family correlating the two. The patient avoided eating lettuce for over a year, until he tried to reintroduce it into his diet. This resulted in similar symptoms as the previous episodes, however, it took more time to resolve with antihistamines. At the age of 14, with the hope that he had outgrown the allergy, he once again tried to reintroduce lettuce. Symptoms were similar to previous occasions, but this time involving a more extensive rash, which urged him to consult a dermatologist who advised him to avoid lettuce in his diet. No official allergy testing was conducted. Since then, the patient avoided lettuce in his diet, without any accidental exposures or reactions. He has no other known food allergies and tolerates a variety of fresh fruits, vegetables, and nuts.
The patient is of Greek Cypriot origin, and was normally delivered at term, without any perinatal problems. From his teenage, he developed mild rhinitis symptoms triggered mainly by climate/temperature changes and exposure to dust from storms, for which he does not take any treatment. He has solar sensitivity resulting in itchy erythematous patches on sun-exposed skin, which resolve spontaneously. The remaining history is unremarkable. His height is 175cm and has a body mass index (BMI) of 29.2. He is a non-smoker and drinks socially on weekends.
Lettuce allergy investigation
Initial assessment
SPTs with positive (histamine) and negative (normal saline) controls (extracts and lancets manufactured by Inmunotek, Madrid, Spain), along with a prick-to-prick test using fresh lettuce were initially performed (Figure 1). As the SPT to lettuce was borderline positive [mean wheal diameter (MWD) of 1.5 mm], an OFC was further proceeded with to confirm his allergy or tolerance to lettuce. Increasing doses of fresh Iceberg lettuce (starting with 1/4 of a medium size leaf, followed by 1/2, one, and three leaves of lettuce) were given in 30-min intervals. The patient was closely observed and vital signs were monitored during the challenge. Medication and equipment for the management of anaphylaxis were readily available.
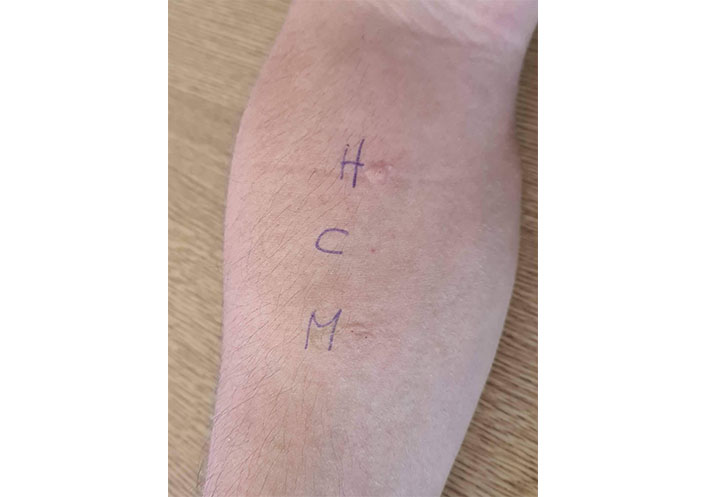
SPT results in MWD. H = histamine, 3 mm; C = negative control, 0 mm; M = fresh Iceberg lettuce, 1.5 mm
The patient did not develop any symptoms with the first three doses of lettuce. However, 12 min after the final dose, he developed erythema of his palms. In the following minutes, the reaction progressed with abdominal discomfort, itching between his fingers, a burning sensation over his face, bilateral tinnitus, and facial flushing. An oral antihistamine (cetirizine syrup 1 mg/mL), 20 mls, was administered immediately. Over the following five minutes, he developed generalized itching and urticaria on his trunk (Figure 2) and lower extremities. Blood pressure remained within normal range, and no respiratory compromise was observed at the time.
His symptoms resolved completely within the following time frame after the administration of cetirizine: generalized itching within 30 min, tinnitus and facial flushing within 45 min, and all other symptoms within 60 min.
Further allergy testing
One month following the initial investigation, and after a review of the literature on lettuce allergy, the team proceeded to further skin testing with additional food and aeroallergens, particularly those known to cross-react with lettuce (Figure 3). The following Inmunotek extracts were used to perform SPTs: Positive control—histamine, Negative control—normal saline, peach, carrot, apple, tomato, potato, silver birch, alder, olive, cypress, poplar, Platanus, mixed grasses, mixed cereals, ragweed, mugwort, Parietaria, house dust mite, cat, dog, Alternaria, and Aspergillus. Prick-to-prick tests were performed using fresh Iceberg lettuce, Batavia lettuce, dandelion greens, and rocket (Arugula).
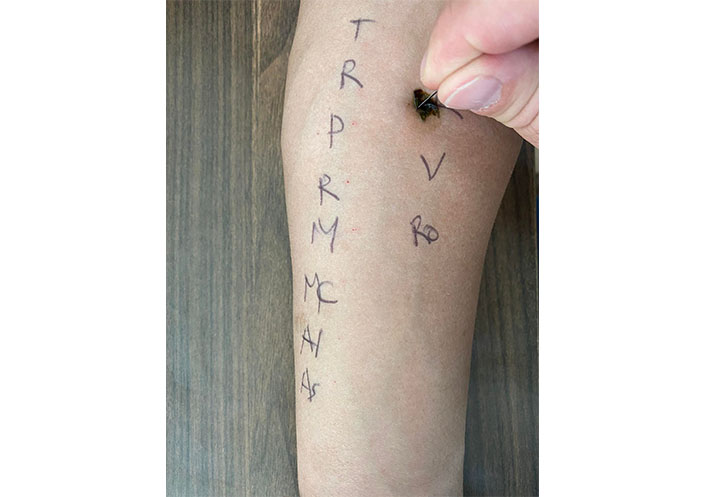
Prick-to-prick skin test with fresh lettuce. T: Timothy grass; R: rye grass; P: Parietaria; R: ragweed; M: mugwort; MC: mixed cereal; Al: Alternaria; As: Aspergillus; Ro: rocket; V: dandelion greens lettuce
Skin tests were positive for histamine, Iceberg lettuce, Batavia lettuce, and dandelion Greens (MWD of 3, 6, 4, and 3 mm respectively), and negative for all other allergens tested (Figure 4).

Positive SPT for all three lettuce types in MWD. I = Iceberg lettuce, 6 mm; R = Batavia lettuce, 4 mm; V = dandelion greens lettuce, 3 mm. Negative SPT for the following, in order. H: histamine; O: negative control; C: cat; D: dog; H1: Dermatophagoides pteronyssinus; H2: Dermatophagoides farinae; B: birch; A: alder; O: olive; P: pine; C: cypress; Po: poplar; Pl: Platanus; MG: mixed grasses; B: Bermuda grass
Literature review on lettuce allergy
Background
Lettuce (Lactuca sativa), a member of the Compositae family, is commonly consumed in the Mediterranean region as a fresh vegetable in salads [1, 2]. This plant family comprises vegetables such as endive, artichoke, chicory, chard, and escarole, as well as plants including ragweed (ambrosia), mugwort (artemisia), and dandelion (taraxacum) [1, 3].
Although lettuce allergy is considered rare, a number of studies have reported hypersensitivity reactions to lettuce [3–7], with most suggesting lipid transfer protein (LTP) as the predominant sensitizing allergen [1, 8–16]. LTPs are widespread pan-allergens identified in both plant- and non-plant-based products, with evidence indicating cross-reactivity [1].
In Cyprus, an island in the transition zone between Europe and the Middle East, with a population of 1.2 million [17], there are no reported cases of lettuce allergy in the literature [8]. However, through personal communication with Dr. Nicolaou, who runs the only pediatric food allergy clinic on the island, there was only one other lettuce allergy case, aside from the one presented in this report, in 12 years.
Clinical presentation of lettuce allergy
Symptoms of lettuce allergy are heterogeneous in nature, affecting any organ system with varying severity. Reactions are mainly immunoglobulin E (IgE)-mediated, however, cases driven by non-IgE mechanisms have been described [8, 10]. They may present locally to the skin (contact urticaria or dermatitis), the oropharynx (oral allergy syndrome), the gastrointestinal tract (abdominal pain, vomiting, diarrhea), or become more generalized with cardio-respiratory compromise (anaphylaxis) [9]. Cofactors, including non-steroidal anti-inflammatory drugs (NSAIDs) and/or exercise, are commonly necessary for the elicitation of lettuce-allergy symptoms [9].
In a study that identified allergens associated with lettuce allergy, the most frequent clinical symptoms reported were found to be cofactor-enhanced anaphylaxis (47.61%), anaphylaxis (21.42%), oral allergy syndrome (16.66%), and urticaria (11.9%) [8]. Although LTP-associated lettuce allergy has a similar presentation to LTP allergy syndrome, its manifestations are usually associated with more generalized symptoms and anaphylaxis [14].
The literature also includes cases of contact dermatitis triggered by lettuce. In a case report presenting a 56-year-old male with a lettuce allergy, skin symptoms were almost exclusively experienced. The patient had gradually worsening generalized urticaria, angioedema, burning erythema of the face, and lettuce ingestion-caused perioral dermatitis. The patient did not experience non-skin/non-mucosal symptoms, which could have been in part due to the patient’s outdoor occupation and hobby of gardening [10]. Krook [18] in 1977 reported two cases of chronic dermatitis of the hands, due to a combined delayed and immediate allergy. The patients presented with vesicular, itching eruptions of the skin within minutes of skin contact with fresh lettuce.
Lettuce and cross-reacting allergens
A number of allergens have been reported to cross-react with lettuce, however, these allergens fit into a small number of protein families [19]. LTP is largely considered the most common food allergen in the Mediterranean area, with LTP-associated peach allergy being the most prevalent [11]. Some patients are exclusively allergic to a single LTP-based food, whereas others develop sensitization and IgE cross-reactivity between LTPs in a broad spectrum of foods and/or pollen. The latter has been termed the LTP syndrome [12], and has mainly been described in patients reacting to peach, lettuce, walnut and hazelnut [8].
Muñoz-García et al. [8] aimed to determine the frequency of LTP syndrome in lettuce-allergic patients, by using immunoblotting and mass spectrometry to determine specific IgE to LTPs. The results from 30 patients indicated that lettuce allergy is mostly due to LTP sensitization [Lactuca sativa 1 (Lac s 1)]. A majority of the patients (87.5%) were also sensitized to peach LTP [Prunus persica 3 (Pru p 3)], and had an allergy to peach prior to their lettuce allergy symptoms. This suggested that peach acted as the primary sensitizer for patients’ developing lettuce allergy. Patients in the study were found to be sensitized to nuts and pollens; walnut [Juglans regia 3 (Jug r 3)] 78%, peanut [Arachis hypogaea 9 (Ara h 9)] 67%, hazelnut [Corylus avellana 8 (Cor a 8)] 44%, Platanus [Platanus acerifolia 3 (Pla a 3)] 87.5%, mugwort [Artemisia vulgaris 3 (Art v 3)] 44% and profilins 8.3% [8].
The above-mentioned report supports a previous study by Hartz et al. [13], who used similar methods to carry out the molecular characterization of both peach and lettuce LTP allergens, Pru p 3 and Lac s 1 respectively. Aside from identifying a strong association between IgE sensitization to Lac s 1 and Pru p 3, the two LTPs showed different IgE binding properties. Their data also provided evidence of the peach LTP’s role in sensitizing patients to lettuce allergy [13].
The Lac s 1 protein was originally identified as the major allergen of lettuce, by San Miguel-Moncín et al. [16], in 2003. The study used immunoblotting and inhibition techniques on fourteen patients with lettuce allergy and concluded LTP to be the main cause of hypersensitivity, with 71% of patients having specific IgE to Lac s 1. Furthermore, the presence of LTP sensitivity was found to be a risk factor for more systemic reactions [16].
Bascones et al. [15] analyzed a case of two female patients who experienced symptoms of anaphylaxis after ingesting lettuce. Similar symptoms were observed in the patients after ingestion of fruits from the Rosaceae family including peach and apple, which was subsequently confirmed by SPTs [14]. IgE determination by electrophoresis identified Lac s 1 and Pru p 3 sensitization, which was in agreement with previous studies [8, 13]. In addition to LTP, a study using electrophoresis and mass spectrometry, identified IgE antibodies against thaumatin-like proteins (TLP) and aspartyl proteases, in 50% of lettuce-allergic patients [14]. This was the first study to characterize these proteins as major lettuce allergens.
By performing patch testing, Paulsen et al. [10] identified that their lettuce-allergic patients were highly sensitive to the Compositae family. Strongly positive reactions were observed with extracts of Roman chamomile, Pyrethrum and Chicory amongst others. Rocket, a member of the Brassicaceae family, was not previously identified as a sensitizer. An oral provocation with Rocket was negative, however, it elicited a positive patch test and histamine release test. The authors hypothesized that the positive histamine release test result was a nonspecific response, due to the lack of any congruent immediate-type hypersensitivity signs. Reasons for the negative oral provocation were discussed, one being that the rocket is not allergic enough to elicit systemic reactions, and the other being that there was potential inconsistency in the allergen content in the rocket given for oral provocation and patch testing [10]. Further studies into the relationship between rocket and lettuce allergy could clarify between co-sensitization and cross-reaction.
Platanus pollen amongst other allergens was identified by Bascones et al. [15], who studied a 42-year-old female following anaphylactic shock after ingestion of “Tudela” lettuce hearts. SPTs for “Tudela” lettuce heart, Iceberg lettuce, endive, Platanus acerifolia, and Artemisia vulgaris pollen were positive. Western blot confirmed IgE reactivity to epitopes of the above allergens; however, it also revealed sensitization to potato, carrot, and leek, which did not induce a positive skin reaction. The findings from the case could indicate poly-sensitization, the expression of common epitopes in different proteins or both [15], suggesting further studies are required to understand the relationship.
Other allergens including grass, wall pellitory, olive and cypress, melon, mustard, cereals, tomato, legumes, tree nuts, and runner beans have also been identified as concomitant sensitizations [8]. A comprehensive table of the reported LTP cross-reacting allergens and the food they can be identified in, can be found in the European Academy of Allergy and Clinical Immunology (EAACI) Molecular Allergology User’s Guide, Part C, Table 2 [19]. Non-LTP sensitizations identified in lettuce-allergic patients are presented in Table 1.
| Botanical family (plant foods) | Allergen source |
|---|---|
| Compositae | Roman chamomilePyrethrumChicory |
| Brassicaceae | Rocket |
| Others | PotatoCarrotLeekMelonCerealsLegumes |
Discussion
Current literature suggests that lettuce allergy is uncommon and usually attributed to LTP sensitization, due to cross-reacting allergens. LTP from peach is considered as the primary sensitizer. Most patients present with symptoms not only to lettuce, but to a number of other food allergens and pollen. The case presented in this report describes a patient showing IgE reactivity solely to lettuce, without any other sensitizations as confirmed by SPTs. From a scientific perspective, the application of novel methods and molecular analysis, including singleplex and/or multiplex immunoassays, would be interesting to identify the specific allergenic profile of the patient. Lettuce allergy deserves further attention and investigation. However, in settings with limited access to molecular testing, prick-to-prick tests and OFC remain a practical and clinical approach to confirm allergy or tolerance to lettuce.
Abbreviations
| IgE: |
immunoglobulin E |
| LTP: |
lipid transfer protein |
| OFC: |
oral food challenge |
| SPTs: |
skin prick tests |
Declarations
Author contributions
KA and NN: Conceptualization. KA: Writing—original draft. KA, EM, AP, and NN: Writing—review & editing. NN: Investigation, Supervision. All authors contributed to the manuscript revision, and read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study was approved by the Cyprus National Bioethics Committee EEBK 21.1.01.03.
Consent to participate
Informed consent to participate in the study was obtained from the patient.
Consent to publication
Informed consent to publication was obtained from the relevant patient.
Availability of data and materials
The anonymized medical notes and test results could be provided upon request from the Asthma and Allergy Center (Nicolaos Nicolaou, nic.nicolaou@googlemail.com).
Funding
Not applicable.
Copyright
© The Author(s) 2023.
