Affiliation:
1Department of Medical Science and Public Health, University of Cagliari, 09042 Monserrato (CA), Italy
Email: andrea.giovanni.ledda@gmail.com
ORCID: https://orcid.org/0009-0003-5456-2359
Affiliation:
2Department of Allergy and Immunology, Çanakkale Mehmet Akif Ersoy State Hospital, 17000 Çanakkale, Turkey
ORCID: https://orcid.org/0000-0002-4528-5404
Affiliation:
1Department of Medical Science and Public Health, University of Cagliari, 09042 Monserrato (CA), Italy
ORCID: https://orcid.org/0000-0002-4517-1749
Explor Asthma Allergy. 2025;3:100974 DOI: https://doi.org/10.37349/eaa.2025.100974
Received: December 23, 2024 Accepted: February 17, 2025 Published: March 09, 2025
Academic Editor: Garry M. Walsh, University of Aberdeen, UK
The article belongs to the special issue The Global Picture of Asthma after Guideline Changes and the COVID Pandemics
Telemedicine (TM) is rapidly gaining recognition as a valuable tool for accessing medical treatments globally. The article aimed to review the latest literature on the role of TM in asthma care. It has been shown that TM offers numerous advantages for patients and clinicians, facilitating an easier access to healthcare resulting in higher patient satisfaction. Telemedicine technology, pushed by the COVID-19 pandemic, has improved asthma management, notably treatment adherence. Smart inhalers, wearable gadgets, and smartphone apps allow doctors to make data-driven decisions and empower patients to manage their diseases. Real-world research shows that TM is effective and patient-friendly. Infrastructure constraints, data security issues, and long-term patient engagement must be addressed. In conclusion, a hybrid strategy combining TM and in-person visits, enabled by AI and secure digital solutions, can provide equal, efficient, and comprehensive asthma management.
Telemedicine (TM), defined as the remote provision of healthcare services and clinical information through telecommunications technology [1], is rapidly gaining recognition as a valuable tool for accessing medical treatments globally [2]. The use of TM in the management of patients with asthma and allergies has surged recently, particularly in response to the coronavirus pandemic (COVID-19) [1]. TM facilitates easier access to healthcare for all patients. Currently, the waiting periods for in-person consultations with allergists or primary care physicians frequently exceed three weeks, particularly in remote regions with significant physician shortages [3]. TM ensures the continuity of care through professional communication among medical consultants, utilizing electronic information and communication technologies to share, archive, and access electronic health data for prevention, diagnosis, treatment, monitoring, education, and administration, both locally and remotely [2]. It offers numerous advantages for patients and clinicians, resulting in heightened patient satisfaction. The convenience of TM consultations, in facts, enhances patients’ desire to utilize the healthcare system for both initial and follow-up care, leading to earlier and more effective preventive actions, including timely follow-up appointments. TM also have the advantage to assess clinical parameters while patients are in their usual everyday settings, offering a more authentic view of their health conditions. Therefore, advancements in TM and associated technologies can paradoxically strengthen the patient physician connection by digitally integrating the physician into the patient’s personal environment. Furthermore, TM reduces the risk of exposure to infectious diseases for both patients and healthcare staff associated with in-person visits to healthcare facilities. It also diminishes the carbon footprint by eliminating the need for travel and mitigates socioeconomic barriers to healthcare access. Specific communities, particularly in rural areas, have numerous barriers to healthcare, including geographical and transportation constraints, as well as a scarcity of local specialty and subspecialty medical professionals, such as allergists and asthma experts. TM consultations can be effectively bridging these gaps through integrated software solutions, including audio and video documentation, which enable patients to revisit consultations for better understanding and adherence to medical advice. The capacity for recording and playback of TM consultations may improve patient education regarding disease management and prevention, alleviate the burden of memorizing healthcare providers’ singular recommendations, and further empower individuals to participate actively in their healthcare [4].
Before the COVID-19 pandemic, in-person consultations constituted a routine component of the examination, evaluation, and management of asthma. The assessment of the patient’s asthma control included office spirometry, pulse oximetry, a physical examination [1] and Asthma Control Test (ACT), a patient self-administered tool useful in assessing asthma control [2]. Nevertheless, even before the pandemic, there was acknowledgement of the advanced state of technological solutions for TM and discussions over the expanding role of such consultations in conjunction with, or even replacing, conventional in-person medical evaluations. Over the past decade, TM has attracted significant attention for its potential to improve asthma outcomes, particularly in managing complex and “difficult-to-manage” asthma cases [3]. Nonetheless, health care professionals, young individuals, and their families expressed concerns regarding access, confidentiality, and safeguarding consequences [3].
The COVID-19 pandemic significantly impacted global healthcare systems, revealing essential vulnerabilities and highlighting opportunities for innovation in healthcare management. Maintaining continuity of medical treatment for patients while minimising infection risk for healthcare staff, patients, children, and families became a major challenge in hospitals and outpatient clinics. One of the most significant trends among these shifts has been the heightened utilisation of TM [4]. During this period, TM facilitated the continuity of care and potentially improved access to services when in-person consultations were unfeasible, either due to a suspected COVID-19 infection or the challenges associated with attending an in-person appointment [5].
The COVID-19 pandemic prompted an exceptional transformation in healthcare services, compelling physicians and healthcare organisations globally to swiftly adopt TM solutions to diminish or substitute in-person consultations. TM has enhanced workforce sustainability, minimised clinician direct patient exposure, decreased overall personal protective equipment utilisation, and may alleviate clinician burnout. It has also enabled the staffing of both large and small facilities that are inundated with pandemic-related patient flows. Furthermore, TM has been employed for surge management or “forward triage,” which involves the assessment of patients prior to their arrival at the emergency department. Direct-to-consumer visits provided rapid patient screening while safeguarding patients, physicians, and the community from exposure. The urgent need for TM consultations has created a necessity to proficiently instruct allergists and immunologists on optimizing utilization [6]. During the pandemic one of the focus of physicians was to improve symptom management for severe asthmatics as non-compliant asthmatics made more efforts to schedule appointments during the pandemic. As a consequence, severe asthma attacks have decreased in primary care and hospitalised patients. Numerous asthmatic patients expressed satisfaction with the utilisation of TM as an efficient intervention for medication prescription and consultation [7].
Remote monitoring technologies have led to significant improvements in patient outcomes by improving asthma patients’ adherence to treatment and improving symptom management. For example, monitoring symptoms via mobile apps, wearable devices, and smart inhalers and facilitating patient-doctor communication have allowed patients to become more involved in their own health, resulting in better outcomes and fewer hospital admissions.
Technological advances in recent years, especially due to the effects of the pandemic, have significantly reshaped asthma care and revealed the importance of TM. eHealth technologies such as smart inhalers, wearable devices and mobile applications have played a critical role in more effective management of asthma [8, 9]. For example, smart inhalers are designed to accurately track medication use and provide feedback to patients, which has helped ensure prescription compliance. This can help patients and healthcare providers recognize medication gaps or missed doses, preventing exacerbations. These technologies include live video sessions, wearable devices, remote patient monitoring tools such as electronic diaries and adherence trackers, mobile health apps (mHealth), and file archiving options [8]. Additionally, technologies that enable remote monitoring and measurement of environmental factors are important due to their contributions to asthma and public health.
In addition, developments in artificial intelligence (AI), which can be integrated into these systems, also contribute greatly to TM. AI has an important potential to be used in areas such as remote monitoring, development of personalized treatment plans, detection of early asthma exacerbations, and providing real-time alerts and predictive analysis. Machine learning models can assist with personalized medication adjustments, and virtual assistants and chatbots can improve symptom management, medication adherence, and patient education. For clinicians, teleconsultations with AI integration may increase decision-making speed by analyzing clinical data such as patient respiratory sounds and patient histories. However, to ensure ethical and effective use of AI, challenges such as data privacy, accessibility, and clinician integration need to be addressed and improved. When implemented responsibly, AI-assisted TM can significantly reduce exacerbations, improve adherence, and optimize long-term asthma outcomes.
Technologies developed based on wearable biosensors for monitoring vital signs in asthma patients include smart clothing, smartwatches, activity trackers, spirometers/peak-flow meters, sensor patches, sensor straps and pulse oximeters [10]. In addition to environmental factors such as temperature and humidity, biomarkers can record findings like wheezing, oxygen saturation, and heart rhythm in asthma, while measurements such as PEF, FEV1, and FeNO, which are essential for patient follow-up, can be performed remotely.
The first identified and implemented role of wearable devices was in fitness, specifically to promote physical activity. While these devices contribute to asthma management, the number of devices specifically designed for asthma remains limited. Additionally, the use of devices to measure sleep quality in asthmatic patients is also being explored. Castner et al. [11] compared the Fitbit Charge™ device with a validated device, the ActiGraph GT3X+, to validate sleep measurements in asthmatic women and found that the Fitbit device tended to overestimate sleep efficiency and underestimate wake counts compared with actigraphy.
Another type of wearable device is the belt-shaped sensors, which allow estimation of the respiratory patterns using acceleration data obtained from body movements, as demonstrated by Liu et al. [12]. Acoustic monitoring, which involves measuring parameters such as respiratory rate and heart rhythm through a microphone placed on the body, is another approach used in asthma [13].
Electronic inhaler sensors enhance symptom control in asthma patients by monitoring the use of short-acting beta-agonists (SABA), while applications have been developed to enable remote monitoring of pulmonary function tests via cloud-based platforms. For example, the Propeller Health app helps asthma patients track and receive feedback on their medication through digital inhaler systems [14, 15]. Devices like Smart Peak Flow allow patients to measure their peak flows at home and share the results with healthcare providers [16, 17]. Furthermore, digital inhaler systems and other remote monitoring tools, such as Propeller and Teva’s Digihaler have significantly improved asthma management by monitoring both medication use and inhalation technique. These tools empower patients to better manage their condition while enabling healthcare providers to adjust treatment as needed [18].
Digital spirometers represent a significant advancement in asthma management. These portable, user-friendly devices enable patients to measure their respiratory function at home, record the results, and share them with healthcare professionals. By detecting even minor changes in lung function, digital spirometers allow timely adjustments to treatment plans. According to the study by Kouri et al. [18], six digital spirometers capable of performing full spirometric measurements are US Food and Drug Administration (FDA) approved and commercially available. The use of digital spirometers provides healthcare professionals with accurate data, thus increasing compliance with treatment and contributing to the prevention of acute exacerbations.
In addition to smart inhalers, mobile health applications offer significant convenience to both patients and healthcare professionals in personalized asthma management. These applications can record patients’ symptoms, report environmental triggers such as pollen levels and weather conditions, track peak flow measurements, and remind medication doses and times. Many mobile applications have been developed for asthma monitoring. Among the most commonly used applications are AsthmaMD and My Asthma App, which offer features ranging from symptom tracking to personalized treatment plans [19]. Applications like MASK-Air allow patients to record daily allergic rhinitis and asthma symptoms, enabling data sharing between patients and clinicians [20]. An interesting systematic mapping review by Sapouna et al. [21] offers a curated selection of the best suitable mHealth applications for children and adolescents with chronic pulmonary diseases, tailored to the specific demands of each demographic target.
In addition to providing the opportunity to examine patient data for remote monitoring purposes, technological developments that remotely monitor environmental conditions can also contribute to asthma management. A study conducted in the El Paso area utilized a personal digital assistant-based network to telemonitor asthma-triggering gases in schools [22]. This system employs Bluetooth technology to monitor five different toxic gases—Ozone, Carbon Monoxide, Nitrogen Oxides, Sulfur Dioxide—and temperature in real time. This portable and low-cost telemonitoring system allowed close monitoring of environmental conditions in schools, where children who are particularly susceptible to asthma, may be exposed to these pollutants. Such telemonitoring systems have the potential to improve the quality of healthcare, especially in low-income and hard-to-access areas, by helping to identify and control asthma triggers effectively (Figure 1).
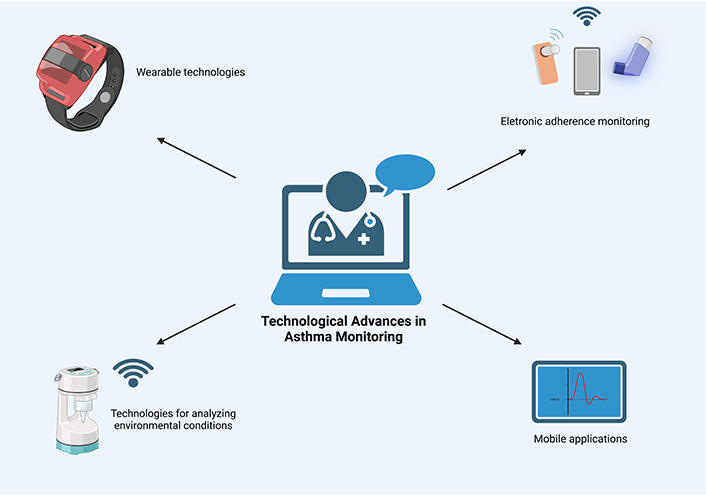
Technological advances in monitoring. Created in BioRender. Ledda, A. (2025) https://BioRender.com/l84m302
Digital inhaler systems, remote patient monitoring, and remote therapeutic monitoring present significant potential as diagnostic instruments and therapeutic interventions to enhance adherence and inhaler technique for patients with difficult-to-control asthma. Various Real-World studies evaluate advantages and disadvantages of TM (Table 1).
Real world evidence studies on TM (telemedicine)
A study utilising digital inhaler systems to gather objective real-time data on medication adherence through electronic medication monitors, which is subsequently relayed to patients via a mobile asthma application and to healthcare professionals through a clinician dashboard for patient counselling, has demonstrated that digital inhaler systems can function as diagnostic instruments and treatment measures to improve adherence and inhaler technique in asthma patients and also assist newly diagnosed patients in achieving proper adherence and inhaler technique and patients with difficult to control asthma in enhancing adherence and technique to prevent the necessity for high-level treatment adverse effects of oral corticosteroids or expensive biologics [23].
A 2016 study compared in-person management with TM. In this instance, TM consultations included the use of digital stethoscopes and a telefacilitator who conducted diagnostic assessments, such as spirometry. The research analysed patient outcomes through asthma questionnaires and assessed patient satisfaction. Both groups had minor statistically insignificant improvements in asthma control, with most TM patients reporting satisfaction with the care received [24].
A six-month study compared TM with in-person asthma outcomes in paediatric patients. Children with asthma in two rural locations had the option of attending in person consultations or TM sessions at a nearby facility. Real-time TM employed a Remote Presence Solution (RPS) equipped with a digital stethoscope, otoscope, and high-resolution camera. Spirometry and asthma education were conducted by a telefacilitator on the RPS. Children from both groups were assessed at the beginning, 30 days, and 6 months. Validated asthma control assessments (ACT, Childhood Asthma Control Test, and Test for Respiratory and Asthma Control in Kids) and patient satisfaction (exclusive to the TM group) served as measures of asthma outcomes. The minimally significant difference of an adjusted ACT that included the three age groups was employed for noninferiority analysis. Out of 169 children, 100 were examined in person, while 69 received TM-based care. All three visits were carried out involving 34 in-person patients and 40 TM patients. Both groups demonstrated minor improvement in asthma control, though not to a statistically significant degree. TM was equivalent to face-to-face consultations. The majority of participants in the TM group expressed satisfaction. The study shows how both in-person and TM asthma treatments can be equally helpful for paediatric patients. Authors concluded that TM can substitute for in-person physician-led asthma treatment and management [6]. Mammen and Java et al. [25], describe clinically integrated smartphone-telemedicine program development for asthmatic patients and proof-of-concept testing findings. They used smartphone symptom monitoring, telemedicine consultations, nurse-led self-management training, and clinical decision-support software that automated asthma severity, control, and stepwise therapy assessment, enrolling seven patients mean age of 29.5 (SD 5.22) that participated in a three-month beta test. Asthma outcomes (control, quality of life, FEV1) and healthcare use were measured at baseline and study end. Each participant averaged four TM consultations with 94% patient satisfaction. All participants had uncontrolled asthma at the start, but 5 out of 7 were well-controlled by the end. Asthma control improved by 1.55 points (CI = 0.59–2.51), quality of life by 1.91 points (CI = 0.50–3.31), and FEV1 percent predicted by 14.86% (CI = −3.09–32.80), with effect sizes of d = 1.16, 1.09, and 0.96. The use of preventive healthcare and controller drug prescriptions increased significantly (1.86 visits/year vs. 0.28/year, CI = 0.67–2.47). TM via smartphones may effectively enhance outcomes and facilitate remote asthma care. Nonetheless, meticulous consideration of system capabilities and stakeholder acceptance is essential for successful integration into clinical practice [25].
A study published in 2020 enrolled twelve patients mean age of 41.1 (SD 9.9) with moderate asthma in a single-center trial and conducted pulmonary function tests at home twice daily with mobile spirometry (mSpirometry) for a duration of 28 days, as well as weekly at the clinic. Daily and average subject compliance data was collected. A simulation was performed to evaluate whether mSpirometry could enhance statistical power compared to traditional clinic methods. The average subject compliance with mSpirometry was 70% for twice-daily usage and 85% for at least once-daily usage. The mSpirometry FEV1 had a strong correlation with clinic measures taken in the same morning (r = 0.993) and afternoon (r = 0.988), with a smaller mean difference observed in the afternoon (0.0019 L) compared to the morning (0.0126 L) readings. The test-retest reliability of mobile spirometry (ICC = 0.932) and clinic spirometry (ICC = 0.942) was comparable. This research demonstrated higher accuracy with dense mSpirometry compared to sparse clinical measurements, higher compliance with repeated at-home mSpirometry, high concordance and equivalent test-retest reliability with clinic counterparts, and enhanced statistical power, indicating its potential utility in asthma clinical research [26].
Another study published in 2023 investigated patient and physician engagement with a new virtual care solution, the KevaTalk app and Keva365 platform, and evaluated the benefit of a remote patient monitoring tool for both groups. The authors also examined physician and patient use of the platform and how devices affect engagement and monitoring. The trial included patients with a history of moderate to severe asthma and tracked remote spirometry, oximetry, app check-ins, alerts, and escalations. Daily data reviews and predetermined criteria for physician evaluation based on patient symptoms and objective data were set. This study, enrolling 25 patients, showed that individuals with asthma could use a novel RPM platform. The software showed excellent patient engagement and satisfaction while providing physicians with real-time subjective data to remotely evaluate patients for clinical decision-making. Escalations prevented patients from exacerbations and reduced the need for emergency department visits, highlighting how continuous chronic disease monitoring could be superior to episodic care. The findings suggest potential for improved quality of life, better clinical outcomes, and significant healthcare cost savings [27].
Especially during and after the pandemic, TM is taking on broader roles in chronic asthma management and improving asthma management, but its role in emergent asthma exacerbations is still evolving. Although TM cannot replace in-person emergency care for severe exacerbations requiring oxygen therapy, bronchodilators, or intubation, it can provide early intervention, triage, and remote guidance for patients experiencing worsening symptoms [28]. Wearable devices and smartphone-based AI tools can monitor lung function, detect respiratory rate changes, cough patterns, and voice changes, and alert patients or healthcare providers early on in asthma exacerbations, enabling early intervention. Virtual triage and real-time consultations may reduce unnecessary emergency department visits by connecting patients with moderate asthma exacerbations to physicians via TM. Through video calls, clinicians can assess symptoms, guide patients on effective inhaler therapy dosage, and determine if emergency room visits are necessary. Additionally, integrating TM into emergency departments could enable emergency room staff to be more prepared by providing pre-arrival data on patient severity. Additionally, in resource-limited settings, paramedics can consult with specialists remotely and receive real-time guidance on managing severe exacerbations before arriving at the hospital. Despite its benefits, there are many limitations and risks to the use of TM in emergency care. Severe attacks still require in-person treatment and TM certainly does not replace IV treatment, oxygen or mechanical ventilation. In addition, since technical problems such as not being able to provide a stable internet connection can lead to life-threatening consequences in emergency situations, therefore, the importance of patients applying to the nearest emergency room in cases where severe exacerbations are suspected must be explained to patients and their caregivers.
While TM offers significant benefits, such as improved access to care, faster specialist input, reduced costs, and enhanced asthma management, its widespread adoption faces multiple challenges [3, 24, 25]. Several obstacles to the implementation of TM in healthcare settings persist. First, many individuals may lack access to the necessary equipment or general infrastructure required to utilise TM programs. Furthermore, given the elevated initial engagement along with decreased continuous involvement, it is imperative to evaluate the long-term efficacy of these programs to develop measures for maintaining users. The plethora of telehealth program alternatives, intricate billing procedures that worsen paperwork requirements, along difficulties in doing full physical examinations have resulted in lower enthusiasm for implementation. These issues are being addressed, and innovative solutions for improving remote evaluations are available. At the same time, it is crucial to note that the goal of most TM programs is not to completely replace in-person doctor visits but to supplement them with virtual appointments where feasible. Furthermore, providers and institutions encounter a lack of integration between specific TM programs and electronic health records, requiring institutions to seek solutions to improve the information sharing among TM programs, specialists, and primary care physicians. Consequently, administrators are hesitant to spend much in these technologies. On the other hand, the advancement of TM raises concerns regarding patient confidentiality and data security. Since patient data is shared remotely, it is crucial to protect it with strong encryption methods and privacy protocols. Security measures such as blockchain technology or multi-factor authentication can increase trust in such systems. Older patients (baby boomer generation and older cohorts) exhibited a lower propensity for utilising video compared to younger patients. The discrepancies in usage may stem from divergent social factors, preferences of patients and providers, technological proficiency, availability of a stable internet connection, and the complexity of patient conditions and types of medical visits (e.g., evaluation, diagnosis, consultation, or intervention) [29]. A hybrid model for asthma care, where patients can choose between virtual and in-person visits, offers flexibility but may also raise concerns about equity and cost. While TM can reduce hospital visits and optimize resource use, it may also result in unequal distribution of resources, favoring patients with better technological access and digital literacy. Future studies should evaluate how voluntary TM selection impacts healthcare disparities, cost-effectiveness, and overall system sustainability. These advantages and challenges underscore the need to carefully evaluate multiple factors before the widespread implementation of TM [3] (Table 2).
PROs and limitations of TM for asthma patients
| PROs | Limitations |
|---|---|
| Improved access to care | Requirement to specific equipment and to TM programs |
| Faster specialist input | |
| Reduced costs | Long-term efficacy unknown |
| Enhanced asthma management | |
| Evaluation of clinical parameters in everyday setting | Lack of integration between specific TM programs and electronic health records |
| Reduced risk of exposure to infectious disease | |
| Reduced carbon footprint | Higher age |
| Enhanced involvement in personal healthcare management | Increased paperwork requirement |
Several considerations are essential for the future widespread adoption of TM. First, strengthening the internet infrastructure, including rural and underdeveloped areas, is crucial to expanding access to these technologies. Second, reducing the costs of TM devices will enhance affordability, enabling broader patient reach. Another element that will increase compliance and trust in TM is increasing the sensitivity of the sensors used and personalizing them with AI integrations. Patients and healthcare professionals must be adequately trained on TM applications to ensure effective use. Providing guides or virtual assistants can facilitate user adoption and simplify the process. To enhance engagement, additional features such as gamification, reward systems, or earning badges for consistent use can be incorporated. These strategies can encourage patients to develop a daily usage routine, ultimately improving adherence and long-term involvement with TM platforms (Figure 2).
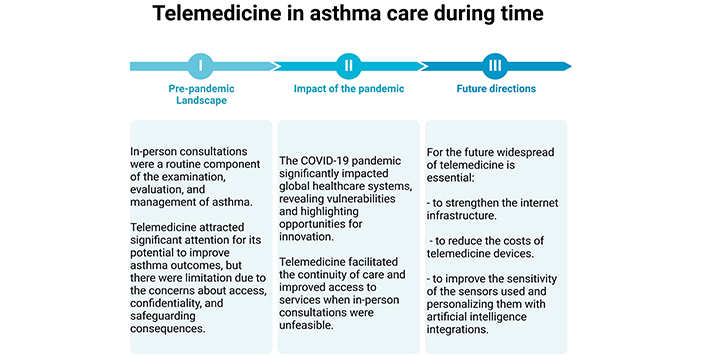
Telemedicine in asthma care during time. Data from [1–5]. Created in BioRender. Ledda, A. (2025) https://BioRender.com/t48p456
The TM technologies accelerated by the COVID-19 pandemic have brought significant changes to asthma management, improving patient outcomes, particularly treatment adherence. Innovations such as smart inhalers, wearable devices, and mobile applications have allowed healthcare providers to make data-driven decisions while encouraging patients to take an active role in managing their conditions. Real-World Evidence emphasizes that TM is an effective and patient-friendly alternative to in-person care. However, challenges such as infrastructure limitations, data security concerns, and ensuring long-term patient engagement need to be addressed. In conclusion, a hybrid model combining TM with in-person visits, supported by advancements in AI and secure digital solutions, holds promise for improving asthma management, but its long-term impact on equity, efficiency, and cost-effectiveness remains to be fully understood. Future studies are needed to assess how patient preferences, healthcare infrastructure, and healthcare costs influence the adoption and sustainability of TM.
ACT: Asthma Control Test
AI: artificial intelligence
RPS: Remote Presence Solution
TM: telemedicine
AGL and OCB: Conceptualization, Investigation, Visualization, Writing—original draft, Writing—review & editing. SDG: Conceptualization, Validation, Visualization, Writing—review & editing, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Riyad Allehebi, Hamdan AL-Jahdali
Yasmeen Othman ... Asmaa Ali
Maria Michelle Papamichael, Charis Katsardis
Yuto Hamada ... Peter Gerard Gibson
Teresa Garriga-Baraut ... Margarita Tomás-Pérez
