Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0002-0986-1902
Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0002-5619-0750
Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0001-7800-785X
Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0002-8194-0285
Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0001-5959-2109
Affiliation:
1Department of Cardiology, Medical University of Łódź, 91-347 Łódź, Poland
ORCID: https://orcid.org/0000-0002-5850-8187
Affiliation:
2Department of Internal Diseases and Clinical Pharmacology, Medical University of Łódź, 91-347 Łódź, Poland
Email: wierzbowska@ptkardio.pl
ORCID: https://orcid.org/0000-0002-7623-5389
Explor Cardiol. 2023;1:4–14 DOI: https://doi.org/10.37349/ec.2023.00002
Received: December 23, 2022 Accepted: March 09, 2023 Published: July 14, 2023
Academic Editor: David S.H. Bell, University of Alabama, USA
The article belongs to the special issue Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coin
Aim: Left ventricular (LV) hypertrophy (LVH) is a common and relevant complication of arterial hypertension (AH) and 12-lead electrocardiogram (ECG) is widely used for its preliminary assessment. The aim of the study was to compare the correlations of four ECG-derived criteria of LVH and left atrial (LA) anteroposterior diameter with LVH assessed by echocardiography and expressed as left ventricular mass (LVM) index (LVMI) in search of the most accurate preliminary indicator of LVH.
Methods: The study included 61 subjects with AH [age (year) 69 ± 10, 17 females] and 27 without AH, (age 40 ± 9, 10 females) evaluated with 12-lead ECG and transthoracic echocardiography (TTE). As the ECG-based criteria of LVH Sokolow-Lyon index (SLI), Cornell voltage (CV), Cornell product (CP), and Romhilt-Estes point score (RES) system were evaluated. The ECG indices and LA diameter were correlated with LVMI and correlations coefficients were compared.
Results: Among ECG-LVH indicators SLI showed the closest correlation with LVMI [rank correlation coefficients (rho) = 0.38, P < 0.0001], followed by CV and CP with rho = 0.33, P = 0.002 and rho = 0.32, P = 0.002, respectively, whereas RES did not correlate significantly with LVMI. The strongest correlation with LVMI was found for the LA diameter with rho = 0.73 and P < 0.0001, showing an even stronger correlation in women—rho = 0.8 (P < 0.0001) vs. rho = 0.65 (P < 0.0001) in men. In the multivariate analysis, the LA was the only independent predictor of the increased LVMI with R2 = 0.52, P < 0.0001.
Conclusions: LA diameter outperformed significantly the ECG indices as far as the correlation with LVMI was concerned and emerged as the only independent predictor of mild and moderate LVH in hypertensive patients. Among the ECG criteria, the strongest correlation was shown for SLI, followed by CV and CP indices.
Arterial hypertension (AH) is one of the most often diagnoses in internal medicine and cardiology, with a prevalence of 30–45% in the general population in Europe [1, 2]. One of the most common complications of AH is the left ventricular (LV) hypertrophy (LVH), which forms a fundamental stage in the development of diastolic heart failure [3, 4]. Patients with chronically elevated blood pressure, as a result of increased afterload, suffer from compensatory remodeling of the myocardium. This remodeling, mediated by elevated G protein kinase, consists of both cardiomyocytes overgrowth and type I collagen over-synthesis, resulting in increased cardiac walls stiffness [5–8].
The development of LVH is fueled by a wide range of factors beyond AH, including genetic and environmental factors as well as various comorbidities acting by proinflammatory state [9–11]. Significant aftermaths of LVH include diastolic heart failure, coronary perfusion impairment, increased QT dispersion, and a higher risk of cardiac arrhythmias [12, 13]. In view of the documented prognostic significance of LVH resulting in shorter survival time and an increased risk of sudden cardiac death, it is essential to understand better the diagnostic potential, limitations, and hierarchy of widely accessible electrocardiographic and echocardiographic indices to improve the sensitivity of early LVH detection [14, 15].
Over 30 parameters based on the standard 12-lead electrocardiogram (ECG) have been described and used as indicators of LVH [16–20].
The indices commonly used in clinical practice are displayed in Table 1 and Table 2 [21]. Current research has shown relatively low sensitivity of ECG for the diagnosis of LVH, according to Pewnser systematic review of 5,608 patients [22]. On the other hand, ECG-LVH indices correlate with the clinical LVH complications and can serve as predictors of strokes, heart failure, or atrial fibrillation [18, 19]. Cardiac magnetic resonance is nowadays considered as a new gold standard for diagnosis of LVH, since it allows full, real-time visualization of left ventricular walls [21, 23]. However, in practice, the most widely used reference parameter for the LVH assessment is LV mass (LVM) and left ventricular mass index (LVMI) based on echocardiography, see Table 3. [19, 24]. From echocardiographic parameters diastolic function indices and especially left atrium was shown in many studies as simple and repeatable predictor of clinical outcomes [2, 25–27].
Definitions of electrocardiographic indicators of LVH used in the study
| The SLI | CV | CP |
|---|---|---|
| SV1 + RV5/V6 > 3.5 mV [28] | RaVL + SV3 > 2.8 mV (men) RaVL + SV3 > 2.0 mV (women) [29] | (RaVL + SV3) × QRS width ≥ 2,440 mm × ms [30] |
aVL: left arm lead of ECG; QRS: an electrocardiographic complex consisting of the Q, R, and S waves; V1, V3, V5, V6: respective precordial leads of ECG
The RES system [31]
| ECG criteria | Points |
|---|---|
Voltage criteria (any of): 1. R or S in limb leads ≥ 20 mm 2. S in V1 or V2 ≥ 30 mm 3. R in V5 or V6 ≥ 30 mm | 3 |
ST-T abnormalities: 1. ST-T vector opposite to QRS without digitalis 2. ST-T vector opposite to QRS with digitalis | 3 1 |
| Indicates of LA hypertrophy: negative terminal P in V1 exceeding 1 mm in depth and 40 ms in duration | 3 |
| Left axis deviation (QRS of –30 or more) | 2 |
| QRS duration ≥ 90 ms | 1 |
| Delayed or intrinsic deflection in V5 or V6 (> 50 ms) | 1 |
4 points—probable LVH > 5 points—diagnosis of LVH | |
P: P wave of ECG; ST-T: ST segment and T wave
Echocardiographic indicators of LVH according to 2015 recommendations for cardiac chamber quantification by echocardiography in adults: an update from the ASE and the EACVI [32]
| LVM (by the Penn convention) | LVMI in LVH |
|---|---|
Devereux formula for LVM: LVM = 1.04 [(LVEDd + IVSd + PWT)3 – (LVEDd)3] – 13.6 LVMI = LVM/BSA | females > 95 g/m2 males > 115 g/m2 |
| Anteroposterior LA dimension | LA in LVH |
| - | LA > 40 mm |
PWT: posterior wall thickness; -: none
The purpose of the study was to stratify the four most widely used ECG-derived indices of LVH and measured in echocardiography left atrial (LA) anteroposterior dimension according to their correlation with LVMI calculated by two-dimensional (2D) transthoracic echocardiography (TTE) in patients with AH as well as in the control group.
The study was carried out in the group of 88 patients of Cardiology Department of Medical University of Lodz, (61 with and 27 without AH), including 61 males, of average age (year) 60 ± 19. Sinus rhythm was observed in 76 patients and atrial fibrillation (AF) in 12 patients. The average heart rate [HR, bpm (beats per min)] was 71 ± 16, ejection fraction (EF) 49% ± 11%, 16 patients had diabetes type 2. 12-lead ECGs recorded during admission to the department were analyzed, time window between ECG and TTE examinations did not exceed 5 days.
The Sokolow-Lyon index (SLI), Cornell voltage (CV) criteria, Cornell product (CP), and the sum of points according to the Romhilt-Estes point score (RES) were calculated, see Table 1 and Table 2. The results of ECG were correlated with echocardiography data performed in accordance with the American Society of Echocardiography/European Association of Cardiovascular Imaging (ASE/EACVI) guidelines [32]. LV end-diastolic diameter (LVEDd) and LV end-systolic diameters (LVESd), diastolic LV posterior wall thickness at end diastole (LVPWd)/interventricular septal thickness at diastole (IVSd)], and ventricular septal thickness were measured in 2D-TTE. LVM was calculated using the Devereux formula [32, 33]. The LVM index (LVMI) was calculated by indexing the LVM to the body surface area (BSA) as determined by DuBois formula: BSA (m)² = 0.007184 × height (cm)0.725 × body weight (kg)0.425. LVMI values higher than 95 g/m² in women and 115 g/m² in men were used as a criterion for diagnosis of LVH [2]. In the 2D mode, anteroposterior LA dimension was measured in parasternal long-axis (LAX) projection. The criterion of LA > 40 mm was adopted as reference values for LA enlargement [32]. The echocardiographic indices are displayed in Table 3.
Statistical analysis was performed with Statistica™ 10 and MedCalc® 17.4.4 software. The results are presented as average ± standard deviation (SD). The Shapiro-Wilk test was used for distribution checking. Student’s t-test or Wilcoxon test was used to examine the differences between the groups. The strength and direction of correlation between variables were estimated with Pearson’s r or Spearman’s rank correlation coefficients (rho). For groups smaller than 5 Fisher exact test was used. Statistical significance was recognized for P < 0.05.
The research was conducted with the approval of the Bioethics Committee of the Medical University of Lodz number RNN/31/16/KE.
In the studied group, 57 (64%) patients fulfilled the criterion of LVH defined as increased LVMI ≥ 95 g/m2 for women and ≥ 115 g/m2 for men. Mean LVMI was 139.5 g/m2 ± 51.5 g/m2, LA dimension 40.5 mm ± 11.3 mm. Demographic and clinical variables of the studied group are displayed in Table 4. The criteria of LVH according to RES system were fulfilled by 23 patients (26%), according to CP by 12 patients (13.6%), according to SLI by 11 patients (12.5%), and according to CV by 8 patients (9%).
Characteristics of the studied group
| Parameter | AH (n = 61) | Patients without AH (n = 27) | P |
|---|---|---|---|
| Age (year) | 69 ± 10.7 | 40 ± 18.9 | < 0.0001 |
| Males, n (%) | 44 (72%) | 17 (63%) | NS |
| BMI (kg/m2) | 29.4 ± 3.8 | 24.5 ± 4.0 | < 0.0001 |
| DM type 2, n (%) | 16 (26%) | 0 | 0.002 |
| HR (bpm) | 71.1 ± 18.8 | 70 ± 11.8 | NS |
| Sinus rhythm, n (%) | 49 (80%) | 27 (100%) | 0.0301 |
| AF, n (%) | 12 (20%) | 0 (0%) | NS |
| LV EF (%) | 50 ± 11 | 59 ± 15 | 0.0022 |
| LVMI (g/m2) | 158 ± 29.1 | 101 ± 43.3 | < 0.0001 |
| LA (mm) | 45 ± 6.7 | 31 ± 7.1 | < 0.0001 |
BMI: body mass index; DM: diabetes mellitus; NS: none significant, P ≥ 0.05
A comparison of clinical and echocardiography parameters is displayed in Table 5, between the patients without LVH in ECG and the groups with ≥ 1 and ≥ 2 fulfilled criteria of LVH in ECG. There was a statistically significant increase in LVMI values observed between group A: without ECG features of LVH and the group C: with at least 2 ECG criteria fulfilled (P = 0.034), whereas posterior wall and septum thickness differ significantly between group A and respectively group B: with at least 1 ECG criteria fulfilled [IVSd P = 0.0033, posterior wall diastolic thickness (PWd) P = 0.0186] and group C (IVSd P = 0.0147, PWd P = 0.0254).
Comparison of echocardiographic parameters in groups without indicators of LVH in ECG and groups with ≥ 1 and ≥ 2 fulfilled criteria of LVH in ECG
| Parameter | (A) LVH in ECG (–) n = 55 | (B) LVH in ECG (+) ≥ 1 criteria; n = 33 | (C) LVH in ECG (+) ≥ 2 criteria; n = 16 | P A vs. B | P B vs. C | P A vs. C |
|---|---|---|---|---|---|---|
| Females, n (%) | 19 (35%) | 8 (24%) | 3 (19%) | NS | NS | NS |
| Age (year) | 64 ± 18 | 58 ± 20 | 60 ± 22 | NS | NS | NS |
| BMI (kg/m2) | 28.2 ± 4.7 | 27.5 ± 4.1 | 26.6 ± 3.8 | NS | NS | NS |
| EF (%) | 54 ± 11.6 | 51 ± 13.1 | 48 ± 17 | NS | NS | NS |
| LVMI (g/m2) | 131 ± 49 | 153 ± 53 | 160 ± 40 | NS | NS | 0.034 |
| LVEDd (mm) | 48 ± 6 | 50 ± 7 | 51 ± 6 | NS | NS | NS |
| IVSd (mm) | 14.2 ± 3.4 | 16 ± 2.8 | 15.9 ± 2.3 | 0.0033 | NS | 0.0147 |
| PWd (mm) | 12.1 ± 2.1 | 12.9 ± 1.8 | 13.5 ± 2.3 | 0.0186 | NS | 0.0254 |
| LA (mm) | 39.8 ± 11 | 42 ± 11.8 | 43.2 ± 10 | NS | NS | NS |
| E/A (mm) | 1.04 ± 0.5 | 1.05 ± 0.52 | 0.85 ± 0.32 | NS | NS | NS |
| E/E’ (mm) | 8.9 ± 4 | 9.8 ± 5.3 | 9.6 ± 4.4 | NS | NS | NS |
E/A: mitral inflow early wave to atrial wave peak velocity ratio; E/E’: mitral inflow early wave peak velocity to mitral annulus early wave motion peak velocity ratio; (–): LVH according to anyone ECG criteria is absent; (+): LVH is present according to anyone or narrowed below criteria
In Table 6 we compared LA size and ECG criteria separately in women and men with and without LVH. In the majority of comparisons these parameters were higher in the group with LVH independently of sex, but the statistical significance was reached in both sexes for SLI (female P = 0.0016, male P = 0.0368) and for LA (female P < 0.0001, male P < 0.0001) and solely in women for CV (P = 0.0332) and CP (P = 0.0097). Proportion of LVH predicted by left atrium (LA) enlargement reached statistical significance, showing LA diameter exceeding 40 mm in 86% of LVH in both sexes and only in one man without LVH (patient with BSA 1.82 m2), see Table 6.
Comparison of LA dimension and ECG-LVH indices between women and men with and without LVH as defined by sex-specific criteria based on LVMI
| Parameter | LVH (–) by present criteria [13] | LVH (+) by present criteria [13] | P A vs. C | P B vs. D | |||
|---|---|---|---|---|---|---|---|
Women LVMI < 95 g/m2 (A) | Men LVMI < 115 g/m2 (B) | Women LVMI ≥ 95 g/m2 (C) | Men LVMI ≥ 115 g/m2 (D) | ||||
| n | 13 | 12 | 14 | 49 | |||
| Age (year) | 44 ± 11 | 44 ± 16 | 69 ± 14 | 64 ± 18 | < 0.0001 | = 0.0008 | |
| BMI (kg/m2) | 27 ± 6 | 25.2 ± 3.4 | 29.33 ± 4.6 | 28.3 ± 3.8 | NS | = 0.0123 | |
| LA | Median size of LA (mm) | 26 ± 5.7 | 25 ± 9.1 | 44.3 ± 4.8 | 46.6 ± 6.6 | < 0.0001 | < 0.0001 |
| Patients with LA > 40 mm, n (%) | 0 | 1 (8%) | 12 (86%) | 43 (86) | < 0.0001 | < 0.0001 | |
| Average SLI (mV) | 12.5 ± 4.3 | 17.9 ± 6.8 | 21.6 ± 8.3 | 24.9 ± 10.8 | 0.0016 | 0.0368 | |
| LVH by SLI, n (%) | 0 | 0 | 1 (7%) | 10 (20%) | NS | NS | |
| Average CV (mV) | 9.7 ± 5.1 | 14.7 ± 8 | 15 ± 6.9 | 16.8 ± 7.7 | 0.0332 | 0.4 | |
| LVH by CV, n (%) | 0 | 1 (8%) | 3 (21%) | 4 (8%) | NS | NS | |
| Average CP (mm × ms) | 740 ± 403 | 1265 ± 793 | 1486 ± 878 | 1962.7 ± 1114 | 0.0097 | 0.0458 | |
| LVH by CP, n (%) | 0 | 1 (8%) | 3 (21%) | 9 (18%) | NS | NS | |
| Median RES (range) | 1 (0–5) | 3 (0–6) | 3 (1–8) | 4 (1–10) | 0.89 | 0.9 | |
| LVH by RES, n (%) | 2 (15%) | 4 (33%) | 4 (29%) | 13 (27%) | NS | NS | |
Fisher exact test was used when n < 5
The strongest correlation was found between LVMI and LA dimension: r = 0.73, P < 0.0001. In the multivariate analysis, the LA was the only independent predictor of the increased LVMI with the coefficient of determination R2 = 0.52, P < 0.0001 (Figure 1), showing 87% sensitivity and 96% specificity (P = 0.0001) for detection of LVH. When analyzed separately according to sex, higher correlation between LA and LVMI was found in women, with rho = 0.8 (P < 0.0001) vs. rho = 0.65 (P < 0.0001) in men. Moreover, the difference between correlation coefficients was statistically significant (P < 0.0001).
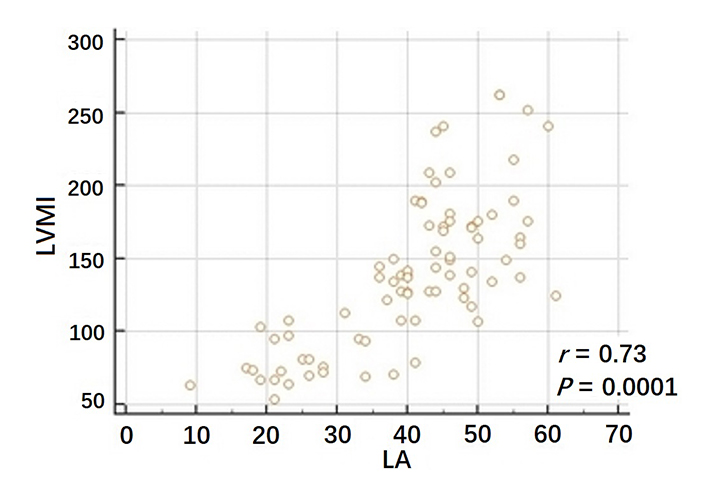
Correlation between LA diameter and LVMI
Note. Adapted from “Poster Session - Poster session 4,” Eur Heart J Cardiovasc Imaging. 2019;20:i864–984 (https://academic.oup.com/ehjcimaging/article/20/Supplement_1/i864/5301370). © 2019 Oxford University Press.
Among electrocardiographic indicators of LVH, the closest positive correlation was found between LVMI and SLI rho = 0.38, P < 0.0001, whereas CV and CP revealed positive correlation of moderate strength with rho = 0.33, P = 0.002 and r = 0.32, P = 0.002, respectively. RES showed no significant correlation with LVMI, rho = 0.004, P = 0.967 (Figure 2, Figure 3). Sensitivity of SLI reached 29% and specificity 100% (P < 0.0001), with even lower sensitivity for CP (19% and 96% respectively, P < 0.0001) and for CV (11% and 96% respectively P < 0.0001).
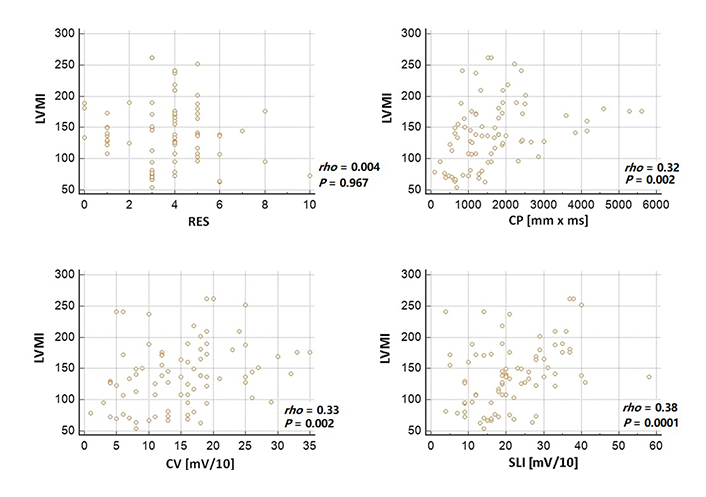
Correlations between electrocardiographic criteria of LVH and LVMI
Note. Adapted from “Poster Session - Poster session 4,” Eur Heart J Cardiovasc Imaging. 2019;20:i864–984 (https://academic.oup.com/ehjcimaging/article/20/Supplement_1/i864/5301370). © 2019 Oxford University Press.
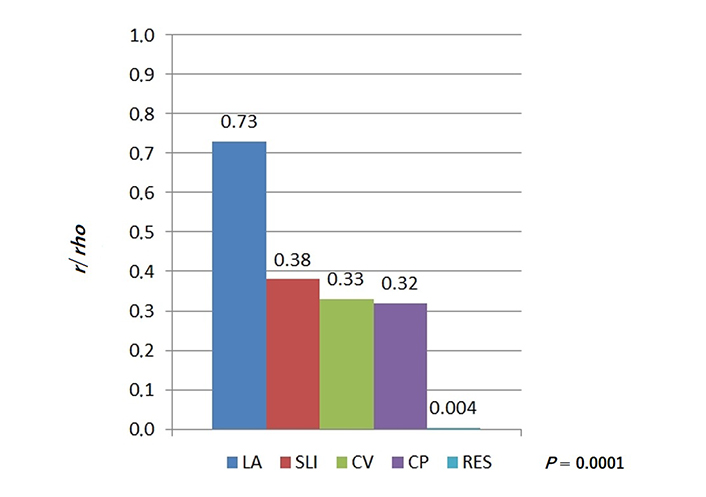
Comparison of correlation coefficients observed for LA and LVM (r = 0.73) and for electrocardiographic criteria and LVM (all r below 0.4)
This study was an attempt towards the assessment of diagnostic utility and gradating of widely used in clinical practice noninvasive echo and ECG-based LVH indices.
We found that simple LA anteroposterior diameter measured routinely with echocardiography is far more closely related with LVM than any of four tested ECG-derived indices. As the proximation of LVM, we used echocardiography-derived LVMI which demonstrated in the literature the excellent correlation (r = 0.96, P < 0.0001) with the gold standard for LVH diagnosis LVMI derived with magnetic resonance imaging [34].
Literature says that independently of patient condition (arrhythmias, valvular heart diseases, etc.) LA enlargement significantly correlates with LVH [35]. Moreover, the prevalence of atrial fibrillation is higher in patients diagnosed with LVH and LA enlargement [36]. It is supposed that early detection of LA enlargement may indicate the presence of paroxysmal atrial fibrillation, which was so far undiagnosed, and the need for anticoagulant treatment [37]. In our study, there is a close correlation between LA and LVMI in the whole group which gets even stronger in women (rho = 0.8 vs. 0.65). Cuspidi and Grassi documented that the presence of LVH offsets the female sex-related protection as far as cardiovascular complications occurring among hypertensive subjects with LVH, and as a result, women and men have comparable cardiovascular risk [38].
Based on our results, from the ECG-LVH criteria, the SLI showed the strongest correlation with the LVMI, better than following CP and CV. According to literature the maximum sensitivity of SLI as the sole diagnostic criterion for LVH detection reached 40%, with the specificity of 90%. The use of ECG criteria for LVH diagnosis is not currently recommended [22, 39, 40]. ECG changes occurring at a later stage of LVH still remain significant predictors of sudden cardiac death, cardiac arrhythmias including atrial fibrillation, heart failure, and risk of stroke [18, 19, 23, 39]. Moreover, the latest research creates new ECG-LVH criteria which were mentioned as more reliable and accurate than SLI, CV, CP, RES as well as significantly correlated with the risk of sudden cardiac death [41, 42].
The undoubted advantages of ECG-LVH indices include the low cost, ease of calculation, complete safety, and wide availability for specialists and general practitioners. Nevertheless, also TTE examination shares the majority of mentioned advantages, simultaneously providing a great amount of additional information. Echocardiography-derived LA diameter had significantly higher sensitivity and similarly high specificity when compared to ECG, being accurate for diagnosis of LVH as it was observed also in our study.
In the multivariate analysis, LA remained the only independent predictor of LVH. The physiological relationship between LV and LA can be characterized as interactive, dynamic, and prognostically relevant as was evidenced in studies characterizing aging, elite athletics, and multiple disease states such as coronary artery disease or hypertension. More recently, functional assessment of the LA has been shown to be, beyond anatomical measurements, a marker of cardiovascular outcomes. Currently, available data suggest that also the combined evaluation of LA size and function has prognostic significance [9, 43]. The search for additional echo-LVH indices beyond the LVMI seems to be especially relevant in the setting of shortened echo examination, without LVMI calculation. This may be particularly useful during examination with portable or pocket-size echocardiography [44].
LA measurement is also faster than the LVMI calculation (directly “on-line” on the monitor vs. entering data into the formula and calculating derived index) and is related with diminished measurement error (one measurement vs. three: both wall thickness and LV chamber diameter). LVMI has also limitations related to using of the thickness of two basal LV segments only, which may be especially important in patients with heterogeneous pattern of muscular hypertrophy. LA volume (and also function) seems to reflect accurately LV filling pressures being cornerstone value with assessment of LV diastolic function and in such a way seems to be adequate "barometer" in the setting of AH [45]. The ability to achieve the right window and LA image (feasibility) is nearly 90% even for an inexperienced doctor or sonographer. In the age of miniaturization and dissemination of ultrasonography, echocardiographic evaluation of LVH can be considered economic and safe [46]. Therefore, it seems reasonable to look for additional parameters supporting the assessment of LVH, such as LA measurement during fast routine TTE examination.
The limitations of our study include the lack of LA volume determination as the more accurate estimation of atrial size. Furthermore, the MRI-based LVM estimation might probably give more accurate data concerning LV dimensions. Moreover, the application of novel echocardiographic techniques could enable LA functional analysis.
Another limitation of our analysis is related to the lack of the preliminary assessment of the required number of patients, although finally included group enabled the detection of statistically and clinically significant relationship between evaluated variables.
To conclude, despite known limitations of ECG LVH criteria they still remain an important screening tool, whereas echocardiography shows advantages in the sensitivity and early pathophysiologic changes detection and this should oblige physicians to conduct echocardiographic examination in a wide spectrum of patients.
AH: arterial hypertension
BMI: body mass index
BSA: body surface area
CP: Cornell product
CV: Cornell voltage
ECG: electrocardiogram
EF: ejection fraction
IVSd: interventricular septal thickness at diastole
LA: left atrium/left atrial
LV: left ventricular
LVEDd: left ventricular end-diastolic diameter
LVH: left ventricular hypertrophy
LVM: left ventricular mass
LVMI: left ventricular mass index
NS: none significant
PWd: posterior wall diastolic thickness
RES: Romhilt-Estes point score
rho: rank correlation coefficients
SLI: Sokolow-Lyon index
TTE: transthoracic echocardiography
BN, KWD, and ET: Methodology. BN, AG, and RN: Investigation. RN, BN, TR, ET, MK, PL, JDK, and KWD: Formal analysis. BN, RN, AG, TR, ET, MK, PL, JDK, and KWD: Writing—original draft.
The authors declare that they have no conflicts of interest.
This manuscript complies with the Declaration of Helsinki. The research was conducted with the approval of the Bioethics Committee of the Medical University of Lodz number RNN/31/16/KE.
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from all participants.
Not applicable.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2792
Download: 31
Times Cited: 0
Piotr Hamala, Karina Wierzbowska-Drabik
Barbara Uznańska-Loch ... Tomasz Rechciński
Maria Możdżan ... Karina Wierzbowska-Drabik
Annamaria Del Franco ... Iacopo Olivotto
Miłosz Broncel, Marlena Broncel
