Abstract
Pneumopericardium, the presence of air within the pericardial sac, is a rare but critical condition that can lead to severe complications such as tension pneumopericardium and cardiac tamponade, causing hemodynamic instability and necessitating immediate intervention. Various etiologies include congenital defects, post-surgical complications, infections, and trauma. Malignancies, such as advanced esophageal cancer or lung carcinoma, can also cause pneumopericardium via fistula formation. Multimodal imaging, including chest X-ray, echocardiography, and computed tomography (CT), is essential for diagnosis. This case report discusses a 65-year-old male with advanced pancreatic adenocarcinoma who developed pneumopericardium following the removal of a left lobe liver drainage catheter. Initial CT imaging revealed liver lesions suspicious for metastatic disease or abscess, leading to drainage procedures. Following the removal of the drainage tube, the patient experienced respiratory distress and hypotension, and computed tomography pulmonary angiogram (CTPA) revealed pneumopericardium, likely due to a fistula formed between the abscess and pericardium. Despite no echocardiographic signs of tamponade, the patient’s persistent hypotension warranted CT-guided pericardiocentesis, resulting in gradual blood pressure improvement. This case highlights the intricate interplay between malignancy, infection, and procedural complications in developing pneumopericardium. It emphasizes the need for a multidisciplinary approach and the importance of considering both the quantity and rate of air accumulation when assessing the risk of hemodynamic compromise. The patient’s hemodynamic instability and subsequent improvement following pericardiocentesis underscore the critical role of timely intervention in managing this condition.
Keywords
Pneumopericardium, CT-guided pericardiocentesis, tamponadeIntroduction
Pneumopericardium, the accumulation of air or gas within the pericardial sac, is a rare but serious condition that can lead to complications such as tension pneumopericardium and cardiac tamponade. These complications can cause hemodynamic instability, requiring immediate intervention [1].
Pneumopericardium can result from congenital defects, post-pericardiocentesis, post-thoracic surgery complications, infections, or positive pressure ventilation. It often occurs after blunt trauma or the formation of a fistula between the myocardium and gas-containing cavities like the pleural space or gastrointestinal tract. Malignancy is also a potential cause, with cases reported in individuals with advanced esophageal cancer or lung carcinoma with ruptured alveoli. Gastro-pericardial fistula, though rare, has a high mortality rate [2]. Diagnosis and management rely on multimodal imaging, including chest X-ray (CXR), echocardiography (ECHO), and computed tomography (CT) [3].
This case report highlights a unique presentation of pneumopericardium following the removal of a left lobe liver drainage catheter, underscoring the rarity and complexity of this clinical scenario.
Case report
A 65-year-old man with a medical history of diabetes mellitus, hypertension, dyslipidemia, and smoking presented with advanced pancreatic adenocarcinoma with metastases to the lungs and liver.
Initial CT imaging revealed liver lesions, raising suspicion for metastatic disease versus abscess in the left lobe. A biopsy indicated an inflammatory process and abscess formation, leading to US-guided drainage for the abscess and concurrent ascites drainage.
A follow-up CT scan showed fluid re-collection, edema, and necrosis, prompting a second CT-guided drainage. After removing the drainage tube, the patient developed respiratory distress and hypotension, leading to a CT pulmonary angiogram (CTPA). The CTPA revealed a spontaneous pneumopericardium, likely caused by the proximity of the abscess to the pericardium, creating a fistula between the skin and pericardium (Figures 1 and 2, Movie S1 and Movie S2).
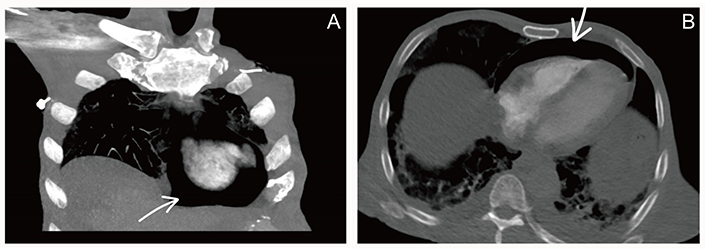
Computed tomography pulmonary angiography. (A) Computed tomography pulmonary angiography (coronal cut) shows air in pericardium surrounding heart (arrow); (B) computed tomography pulmonary angiography (axil cut) shows air in pericardium anterior to heart compressing right ventricle (arrow)
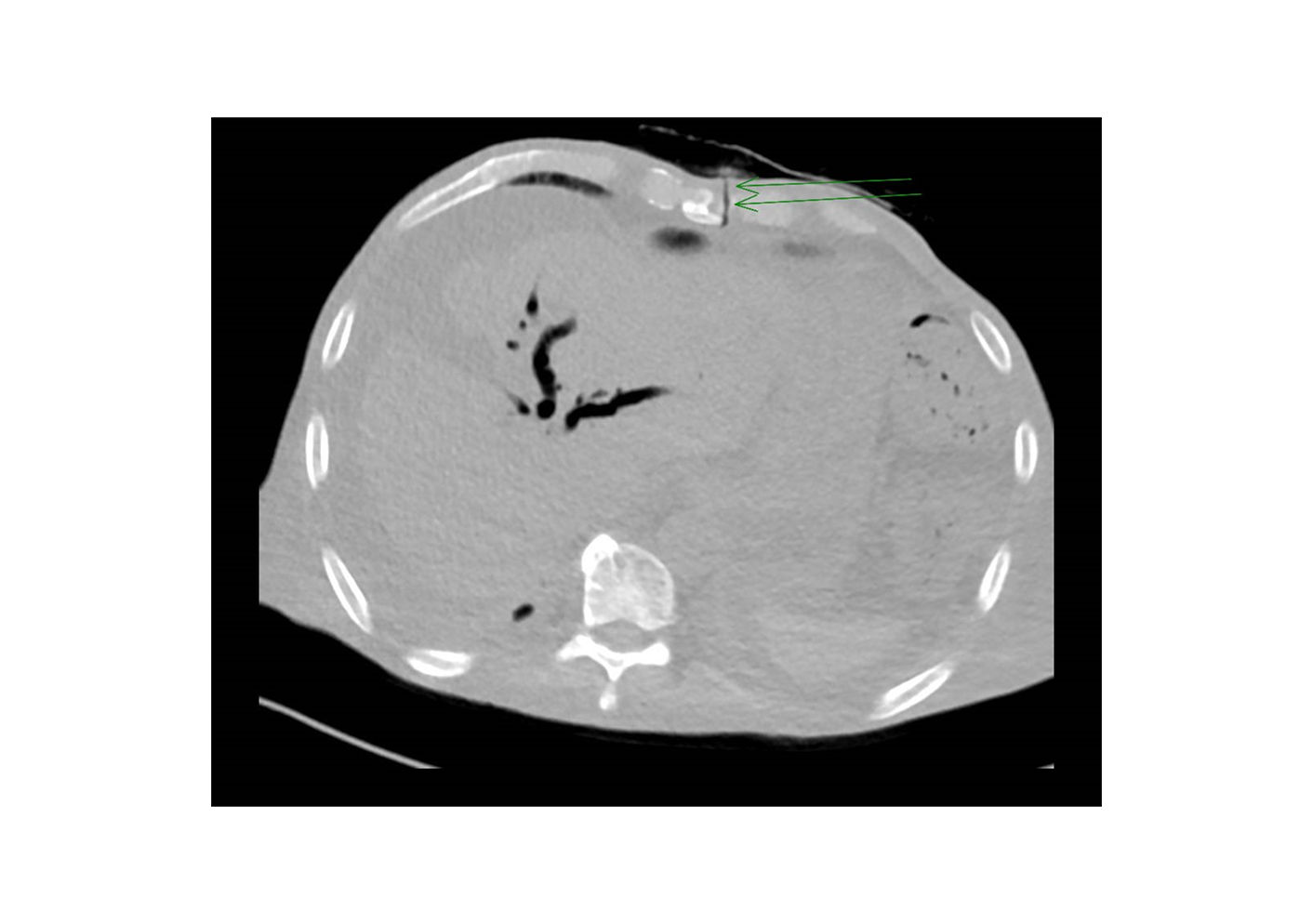
Computed tomography pulmonary angiography. Computed tomography pulmonary angiography (axil cut) shows fistula between pericardium and skin (double arrow)
The patient exhibited hemodynamic instability, including hypotension, tachycardia, and elevated jugular vein pressure (JVP). An ECHO confirmed pneumopericardium but showed no signs of tamponade (Movie S3). Despite the absence of tamponade on ECHO, persistent hypotension necessitated CT-guided pericardiocentesis, which gradually improved the patient’s blood pressure (Movie S4).
Discussion
This case of pneumopericardium following the removal of a left lobe liver drainage catheter in a patient with advanced pancreatic adenocarcinoma illustrates a complex interplay of malignancy, infection, and procedural challenges. Pneumopericardium has diverse causes, including congenital defects, post-pericardiocentesis, post-thoracic surgery complications, infections, positive pressure ventilation, and traumatic fistulas. In this case, the patient’s advanced pancreatic adenocarcinoma with metastases and prior drainage procedures, particularly for a left lobe abscess, likely led to pneumopericardium. The removal of the drainage tube may have resulted in a fistula formation, contributing to this rare complication [2].
Fistula formation can be attributed to the proximity of the abscess to the pericardium, creating a vulnerable area where inflammation and infection can erode tissue planes. This erosion can eventually form an abnormal connection (fistula) between the liver abscess cavity and the pericardial sac. The mechanical act of placing and removing the drainage catheter can further disrupt these fragile tissues, creating a direct pathway for air to enter the pericardial sac from the external environment or adjacent air-containing structures [4].
The amount of air required to induce tamponade varies. Adcock et al. [5] found that hemodynamic disturbances occurred when intrapericardial pressure exceeded 145 mm H2O, equivalent to the rapid introduction of 60 mL of air into the pericardial sac. Celikoglu et al. [6] demonstrated that the speed of air entry is crucial; gradual air entry allows the pericardium to contain up to 500 mL without hemodynamic changes. Other studies report that the pericardium can hold up to 1000 mL of blood without tamponade signs [7].
This information highlights the importance of considering both the quantity and rate of air accumulation when assessing the risk of hemodynamic compromise. In this case, CT-guided pericardiocentesis was performed based on the patient’s clinical presentation and understanding that pneumopericardium can have significant hemodynamic effects even without classical tamponade signs [8].
Managing pneumopericardium in patients with advanced malignancy poses unique challenges. The underlying pancreatic adenocarcinoma, coupled with polymicrobial liver abscess and Streptococcus constellatus infection, complicates the clinical picture. The patient’s hemodynamic instability, characterized by hypotension, tachycardia, and elevated JVP, indicates the severity of the pneumopericardium. Despite no tamponade signs on ECHO, persistent hypotension led to CT-guided pericardiocentesis, improving blood pressure. Case reports suggest that untreated pneumopericardium may lead to complications such as constrictive pericarditis. In cancer patients or those with fistulas, it can progress to constrictive pericarditis, potentially requiring pericardiotomy. However, in this case, the patient improved after CT-guided pericardiocentesis, highlighting the importance of pericardiocentesis even without hemodynamic instability [3, 9].
In conclusions, the presented case underscores the complex interplay of malignancy, infection, and procedural complications in the development of pneumopericardium. The case highlights the diverse etiologies of pneumopericardium, including malignancy-related complications and post procedural interventions. The removal of a left lobe liver drainage catheter, particularly after drainage procedures for a left lobe abscess, played a crucial role in triggering this uncommon complication, possibly through the formation of a fistula. An important consideration in managing pneumopericardium is the variable amount of air required to induce tamponade, as indicated by previous case reports. The speed at which air is introduced plays a crucial role, emphasizing the importance of carefully assessing the quantity and rate of air accumulation in determining the risk of hemodynamic compromise.
Abbreviations
| CT: | computed tomography |
| ECHO: | echocardiography |
Supplementary materials
The supplementary movies for this article are available at: https://www.explorationpub.com/uploads/Article/file/101231_sup_1.pdf.
Declarations
Author contributions
AB: Conceptualization, Data curation, Project administration, Methodology, Writing—original draft, Writing—review & editing. SK: Data curation, Investigation, Project administration. YAM: Data curation, Investigation, Project administration. MM: Investigation, Methodology, Data curation, Project administration, Writing—original draft, Writing—review & editing.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
In accordance with the regulations of the Ethics Committee “Institutional Review Board and Ethics Committee of Sultan Qaboos Comprehensive Cancer Care and Research Center”, ethical approval is not required for case report publications.
Consent to participate
Under the regulations of the Ethics Committee “Institutional Review Board and Ethics Committee of Sultan Qaboos Comprehensive Cancer Care and Research Center”, informed consent to participate is waived for the case report.
Consent to publication
Not applicable.
Availability of data and materials
All data can be shared by the authors, at reasonable request.
Funding
Not applicable.
Copyright
© The Author(s) 2024.