Abstract
Aim:
Significant tricuspid regurgitation (TR) may be a confounding factor when assessing right ventricular (RV) function with imaging techniques. Global myocardial work (GMW) has been proposed as a non-invasive surrogate of RV pressure–volume loops, and it might provide a more accurate evaluation of RV performance than standard echocardiographic parameters, accounting for both afterload and myocardial work efficiency. The aim of this study was to assess the relationship between RV GMW and hemodynamic indices of prognostic significance in pulmonary hypertension (PH) and to compare RV GMW in PH patients with or without TR.
Methods:
This was a proof-of-concept study. Thirty consecutive patients with PH undergoing diagnostic right heart catheterization (RHC) in sinus rhythm were enrolled. Echocardiography was performed in all patients within two hours of RHC.
Results:
Global work efficiency (GWE) was directly correlated (r = 0.562, p = 0.006), whereas global wasted work (GWW) was inversely correlated with stroke volume index (r = –0.447, p = 0.037). Poorer correlation was observed with tricuspid annular plane systolic excursion (TAPSE), and no correlation was observed with TAPSE/sPAP (ratio of TAPSE to systolic pulmonary artery pressure). Patients with moderate/severe TR had lower GWE [83% (77–89%) vs. 96% (94–96%), p < 0.001] and higher GWW [137% (90–179%) vs. 25% (18–89%), p = 0.002]. Similar results were obtained when the analysis was applied to subgroups of patients stratified according to either preserved or poor TAPSE/sPAP.
Conclusions:
RV myocardial work is more strongly associated with hemodynamic indicators of prognosis in PH than standard echocardiographic parameters. Patients with moderate/severe TR have significantly lower values of work efficiency and higher values of wasted work as compared to those without significant TR.
Keywords
Right ventricle, pulmonary hypertension, myocardial work, global longitudinal strain, right heart catheterization, right ventricular functionIntroduction
Evaluating right ventricular (RV) performance is critical in the context of various cardiovascular and pulmonary disorders. It is well documented that diminished RV function correlates with higher mortality and morbidity in conditions like heart failure and pulmonary arterial hypertension [1–5]. Nevertheless, accurately assessing RV function using imaging methods can be challenging when significant tricuspid regurgitation (TR) is present. In such cases, the RV ejects blood into both the pulmonary artery and the right atrium, effectively reducing its afterload and compromising the reliability of standard motion-based assessments.
Importantly, evidence shows that in pulmonary arterial hypertension, patients with a normal tricuspid annular plane systolic excursion (TAPSE) but moderate to severe TR tend to have a significantly poorer prognosis compared to those with well-preserved RV function and minimal TR [6, 7]. Additionally, substantial TR can interfere with evaluating RV–pulmonary artery coupling [8]. Recently, global myocardial work (GMW) has been introduced as a noninvasive measure that integrates myocardial deformation with loading conditions to assess systolic function of the left ventricle [9–11] and of the right ventricle [12, 13]. We hypothesized that the application of RV GMW might be especially valuable for assessing RV performance in patients with pulmonary hypertension (PH) who also have TR.
This study aimed to explore the relationship between RV GMW and prognostically significant hemodynamic indices in PH and to compare RV GMW values in patients with and without notable TR.
Materials and methods
Study design and population
This was a monocentric, single-cohort, observational study. Consecutive patients scheduled for right heart catheterization (RHC) at IRCCS Policlinico San Matteo (Pavia, Italy) from March 2022 to September 2022 were enrolled if in sinus rhythm, with PH of different etiologies, including PH due to advanced left heart failure, and if they had a transthoracic echocardiography performed within two hours of RHC. Exclusion criteria: patients with primary valvular disease or with congenital heart disease. At the end of the observation period, a total of 30 patients were included in the study for analysis. The study complies with the Declaration of Helsinki. Ethical approval for this study is not required as this is a retrospective study. Consent to participate in this study is not required as this is a retrospective study.
RHC
Right-sided heart catheterization was performed using a balloon-tipped catheter via jugular approach. The following hemodynamic parameters were measured or calculated: pulmonary artery wedge pressure (PAWP); systolic, diastolic, and mean pulmonary artery pressure (sPAP, dPAP, mPAP); cardiac output (CO, by thermodilution); cardiac index (CI); stroke volume index (SVi, calculated as CI/heart rate); right atrial pressure (RAP); pulmonary vascular resistance (PVR) calculated as: (mPAP – PAWP)/CO. All hemodynamic parameters were obtained in triplicate, and measurements that exceeded a 10% variability were not accepted.
Echocardiographic and Doppler study
A comprehensive transthoracic echocardiogram was performed with either a Vivid 7 or Vivid E9 digital ultrasound system (GE Medical Systems, Horten, Norway), employing a 1.7/3.4 MHz tissue harmonic transducer. All patients were positioned in the left lateral decubitus orientation. Image acquisition was carried out at a frame rate of 60 to 80 frames per second and digitally stored in cine-loop format for offline evaluation using EchoPAC PC SW-only, version 202, revision 61.0.
TAPSE was measured from M-mode recordings of the lateral tricuspid annulus in an RV-focused apical view. sPAP was estimated from the peak velocity of the tricuspid regurgitant jet, applying the modified Bernoulli equation and adding the mean right atrial (RA) pressure. Mean RA pressure was determined based on the inferior vena cava diameter and its respiratory variation. The TAPSE/sPAP ratio served as a marker of RV–pulmonary artery coupling [14]. Peak systolic myocardial velocity of the RV lateral annulus (RV S′) was obtained via tissue Doppler imaging. RV end-systolic and end-diastolic areas were measured in an RV-focused apical view, and fractional area change (FAC) was computed as [(RV end-diastolic area − RV end-systolic area)/RV end-diastolic area] × 100%. A dedicated RV-focused apical four-chamber view was used to assess the global longitudinal strain (GLS) of the RV, encompassing both the free wall and interventricular septum. dPAP was estimated by measuring the TR jet gradient at the point of pulmonic valve opening. This was determined by aligning the time of pulmonary valve opening on pulsed Doppler pulmonary flow with the TR velocity profile, using the onset of the QRS complex as a temporal reference [15]. The severity of TR was determined at diagnosis using a combination of qualitative and semiquantitative Doppler parameters (color flow jet area, intensity and morphology of the continuous wave Doppler, and vena contracta in the apical four-chamber view), evaluated by a single experienced echocardiographer during post-processing, and categorized on an ordinal scale (absent, mild, moderate, or severe). An inter-observer variability analysis was conducted using the Bland-Altman method on the RV-GLS absolute values measured from the same stored clip. This approach was chosen because these values represent the primary determinant of variability in strain-derived myocardial work parameters, assuming that all observers identified the same valve opening and closing times and that input systemic pressure values were the same. All measurements were performed according to the guidelines of the American Society of Echocardiography [16].
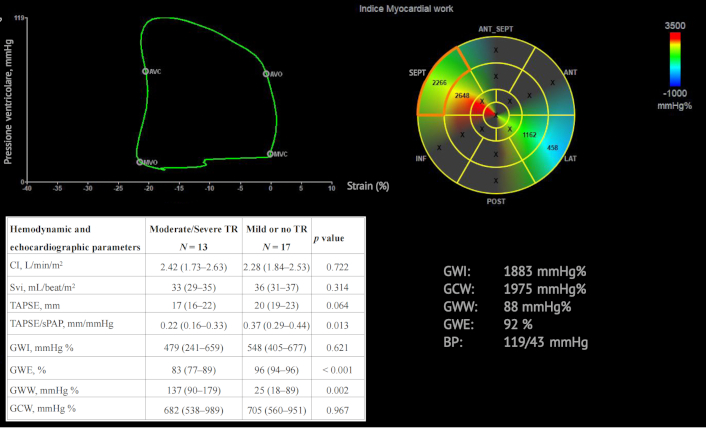
Myocardial work
The proprietary software originally developed for the assessment of LV myocardial work by two-dimensional speckle tracking echocardiography was used (EchoPAC Version 204). RV GLS was calculated according to a 6-segment model (basal, mid, and apical segments of RV free wall and septum). To adapt this procedure initially developed for the left ventricle to the right ventricle, we traced the right ventricle-focused view for all chamber views requested by the software (i.e., the same RV view of the same cycle was traced three times), thus allowing software calculation of GMW of the right ventricle [16]. Subsequently, measurements of RV strain, sPAP and dPAP were synchronized by cardiac cycle timings (determined by pulmonic and tricuspid valve events) to produce pressure–strain loops for the right ventricle. The following parameters were then derived: (1) RV global work index (GWI, mmHg%): the area within the global RV pressure–strain loop, calculated from tricuspid valve closure to opening. (2) RV global constructive work (GCW, mmHg%): defined as the work contributing to the shortening of the cardiac myocytes during systole and the lengthening during isovolumic relaxation. (3) RV global wasted work (GWW, mmHg%): defined as the work contributing to the lengthening of the cardiac myocytes during systole and the shortening during isovolumic relaxation. (4) RV global work efficiency (GWE, %): defined as GCW divided by the sum of GCW and GWW (Graphical abstract).
Statistical analysis
Descriptive statistics are reported as mean ± standard deviation for continuous variables, unless skewed, when median and interquartile range are computed, and as count and percentages for categorical variables. Normality was checked by the Shapiro-Wilk test. Comparisons between subgroups were done with the two-sample t-test, Wilcoxon rank-sum (Mann–Whitney) test, and Fisher exact test, when appropriate. Spearman correlation with 95% confidence interval was used to investigate the relationship between invasively derived CI and SVi and the different components of RV GMW.
Results
Patients population characteristics
The study population included 12 male patients and 18 females, mean age was 55 ± 13 years. Etiology was pulmonary arterial hypertension in 19 patients, group 2 PH in 7 patients, group 3 PH in 1 patient, and group 4 PH in 3 patients. The standard RV echocardiographic data and myocardial work parameters are described in Table S1; overall, the patients showed a moderate dilatation of the right ventricle (RV-EDA was 28 cm2) with a preserved systolic function (TAPSE was 20 mm). In 3 out of 30 patients, TR was absent and sPAP and dPAP estimates were not feasible. RHC data are shown in Table S2; overall, patients had a moderate degree of PH (mPAP = 42 mmHg) and a moderately reduced CI (2.3 L/min/m2). Inter-observer variability analysis (Figure S1) showed a mean bias of –0.96% (95% LoA: –2.8%; 4.7%) for RV-GLS with an intra-class correlation coefficient of 0.927 (95% confidence intervals: 0.854–0.965).
Correlations between GMW components and prognostically relevant hemodynamic parameters
As shown in Table 1, GWI, GWE, and GCW were directly correlated with invasively measured SVi and CI, whereas GWW was inversely correlated with SVi and CI. All correlations were of moderate degree, the strongest correlation was between GWI and CI (r = 0.679; p = 0.001). Poorer correlations were observed between TAPSE or TAPSE/sPAP and SVi and CI.
Correlations between echo-derived estimates of myocardial work with cardiac index and stroke volume index
| Echo-derived parameters | Cardiac index | Stroke volume index | ||
|---|---|---|---|---|
| Spearman’sRho (95% confidence intervals) | p value | Spearman’sRho (95% confidence intervals) | p value | |
| GWI, mmHg% | 0.679 (0.317–0.868) | 0.001 | 0.512 (0.087–0.779) | 0.015 |
| GWE, % | 0.560 (0.148–0.806) | 0.007 | 0.562 (0.151–0.807) | 0.006 |
| GCW, mmHg% | 0.606 (0.210–0.831) | 0.003 | 0.409 (–0.034; 0.718) | 0.059 |
| GWW, mmHg% | –0.244 (–0.608; 0.204) | 0.275 | –0.447 (–0.741; –0.009) | 0.037 |
| TAPSE, mm | 0.518 (0.194–0.740) | 0.003 | 0.479 (0.144–0.716) | 0.007 |
| TAPSE/PASP, mm/mmHg | 0.148 (–0.224; 0.483) | 0.434 | 0.193 (–0.180; 0.517) | 0.517 |
GWI: global work index; GWE: global work efficiency; GCW: global constructive work; GWW: global wasted work; TAPSE: tricuspid annular plane systolic excursion; PASP: pulmonary artery systolic pressure
Myocardial work according to the degree of TR and to the severity of RV dysfunction
Echocardiographic and hemodynamic characteristics according to the degree of TR are shown in Table 2; patients with moderate/severe TR had slightly, but not significantly, lower CI and SVi values but they had significantly lower TAPSE/sPAP and significantly lower GWE and higher GWW.
Hemodynamic and right ventricular echocardiographic data according to the degree of TR
| Hemodynamic and echocardiographic parameters | Moderate/Severe TRN = 13 | Mild or no TRN = 17 | p value |
|---|---|---|---|
| CI, L/min/m2 | 2.42 (1.73–2.63) | 2.28 (1.84–2.53) | 0.722 |
| SVi, mL/beat/m2 | 33 (29–35) | 36 (31–37) | 0.314 |
| TAPSE, mm | 17 (16–22) | 20 (19–23) | 0.064 |
| TAPSE/sPAP, mm/mmHg | 0.22 (0.16–0.33) | 0.37 (0.29–0.44) | 0.013 |
| GWI, mmHg% | 479 (241–659) | 548 (405–677) | 0.621 |
| GWE, % | 83 (77–89) | 96 (94–96) | < 0.001 |
| GWW, mmHg% | 137 (90–179) | 25 (18–89) | 0.002 |
| GCW, mmHg% | 682 (538–989) | 705 (560–951) | 0.967 |
TR: tricuspid regurgitation; CI: cardiac index; SVi: stroke volume index; TAPSE: tricuspid annular plane systolic excursion; sPAP: systolic pulmonary artery pressure; GWI: global work index; GWE: global work efficiency; GWW: global wasted work; GCW: global constructive work
Table 3 shows the hemodynamic and echocardiographic values of patients stratified into low-risk vs. intermediate/high-risk categories of RV to PA coupling (TAPSE/sPAP > 0.32 mm/mmHg vs. TAPSE/sPAP ≤ 0.32 mm/mmHg). In both subgroups, those with moderate to severe TR did not differ in terms of CI and SVi but showed significantly lower values of GWE and higher values of GWW (statistical significance was not reached for GWW in the subgroup with preserved RV to PA coupling because of the very small number of patients).
Hemodynamic and right ventricular echocardiographic data according to TAPSE/sPAP and to the degree of TR
| Hemodynamic and echo parameters | TAPSE/sPAP ≤ 0.32 | TAPSE/sPAP > 0.32 | ||||
|---|---|---|---|---|---|---|
| Moderate/Severe TRN = 5 | Mild or no TRN = 9 | p value | Moderate/Severe TRN = 4 | Mild or no TRN = 12 | p value | |
| CI, L/min/m2 | 2.37 (1.73–2.54) | 2.28 (1.69–2.28) | 0.593 | 2.63 (2.38–2.76) | 2.30 (1.89–2.59) | 0.599 |
| SVi, mL/beat/m2 | 30 (27–34) | 30 (24–35) | 0.894 | 34 (33–36) | 36 (34–48) | 0.541 |
| GWI, mmHg% | 450 (241–482) | 677 (444–772) | 0.240 | 710 (522–809) | 535 (265–634) | 0.316 |
| GWE, % | 78 (76–83) | 87 (86–94) | 0.033 | 92 (91–92) | 96 (96–97) | 0.013 |
| GWW, mmHg% | 174 (137–209) | 103 (89–123) | 0.029 | 81 (64–85) | 23 (16–27) | 0.101 |
| GCW, mmHg% | 680 (538–719) | 1,009 (681–1,020) | 0.350 | 873 (612–989) | 649 (411–809) | 0.363 |
TR: tricuspid regurgitation; TAPSE: tricuspid annular plane systolic excursion; sPAP: systolic pulmonary artery pressure; CI: cardiac index; SVi: stroke volume index; GWI: global work index; GWE: global work efficiency; GWW: global wasted work; GCW: global constructive work
Discussion
The present study demonstrates that the assessment of RV function using myocardial work indices is feasible and potentially useful in the evaluation of PH patients with or without TR. In particular, our findings suggest that severe TR alters the pressure–volume (PV) relationship of the right ventricle by increasing myocardial wasted work, thereby reducing overall work efficiency. This represents the novelty of our study, as it provides insight into the underlying mechanism by which TR impacts RV performance.
Myocardial work is a new echocardiographic tool developed in the last decade that allows one to derive a non-invasive approximation of the PV relationship by combining the LV pressure (estimated by the patient’s blood pressure) with global LV longitudinal strain. PV loops are the “gold standard” for assessing ventricular function since the area of the loop reflects myocardial oxygen consumption, and end-systolic elastance (Ees) reflects load-independent cardiac contractility [17].
However, PV analysis is a highly invasive and time-consuming method, limiting its integration into routine clinical practice. Although originally developed for left ventricular disease, recent proof-of-concept studies have demonstrated that myocardial work techniques can also be applied to estimate RV stroke volume and SVi [13]. We applied this technique to patients with PH of different etiologies to assess how GMW indices correlate with hemodynamic parameters in the presence or in the absence of significant TR, which is an under-appreciated confounding factor when assessing RV function with imaging techniques.
Our results indicate that in the presence of severe TR, conventional parameters such as TAPSE may overestimate RV systolic function. In contrast, the RVMW analysis reveals that PH patients with moderate/severe TR exhibit significantly lower GWE and higher GWW, even if CI and SVi are similar. Furthermore, we observed that standard RV functional indices (e.g., TAPSE and TAPSE/sPAP) showed weak correlations to RVMW parameters. This finding suggests that RVMW may provide incremental information for risk stratification in patients with PH.
Significant TR can lead to an overestimation of RV systolic function in motion-based indices because part of the RV stroke volume is redirected into the right atrium rather than being ejected into the pulmonary circulation. In contrast, GMW is less confounded by TR than traditional parameters because its calculation incorporates afterload (i.e., pulmonary artery pressures), thus offering a more nuanced assessment of RV performance. Indeed, our findings show that patients with moderate/severe TR exhibit higher GWW and lower GWE, which reflects the physiological burden imposed by TR while maintaining a closer link to actual RV systolic workload than standard measures.
Clinical implications
The non-invasive estimation of RV myocardial work via pressure–deformation loops offers a pathophysiologically robust and more comprehensive assessment of RV function compared to conventional echocardiographic indices. RVMW parameters integrate both contractility and pulmonary pressures and are less affected by the presence of TR, which often leads to an overestimation of RV systolic performance with standard measures. Compared to traditional indices, RVMW may thus offer enhanced sensitivity and specificity for detecting subtle alterations in RV function—an important factor for risk stratification and guiding therapeutic decisions in conditions such as advanced heart failure and pulmonary arterial hypertension. In advanced heart failure, for example, grading the severity of RV dysfunction is of outmost importance in patients planned for a left ventricular assist device, to predict whether or not the RV will tolerate the increased flow following implantation; unfortunately, no single echocardiographic parameter can be used to foresee early post-implant RV failure [18]. In patients with pulmonary arterial hypertension, the notion that survival is closely related to RV adaptation to the increased pressure overload has been a consistent finding across studies since more than three decades [19–21]. However, in clinical practice, echocardiographic parameters are not an integral part of any of the risk stratification approaches validated in recent years [22].
Limitations
This study enrolled only patients in sinus rhythm; therefore, the feasibility and accuracy of RVMW assessment in atrial fibrillation remain unknown. Moreover, while our analysis compared PH patients with significant TR versus those without significant TR, data in patients with isolated significant TR are lacking, and the findings strictly apply to the studied population. It must also be acknowledged that the GMW software was originally designed for left ventricular assessment and required several simplifications to adapt it to the right ventricle. The procedure, however, has been validated against the gold standard [13].
Additionally, the current myocardial work methodology does not account for wall stress, wall thickness, ventricular mass, or wall curvature—factors that are particularly relevant given the complex and irregular geometry of the RV. As a consequence, the calculated myocardial work values for the right ventricle may be less precise than those for the left ventricle. Recent publications investigating the use of 3D speckle tracking echocardiography for RVMW evaluation have shown promising results by potentially overcoming some of the geometric limitations inherent in 2D analyses. However, these 3D approaches remain in the early stages of validation and require further study before they can be routinely applied in clinical practice.
Finally, it is important to note that while the area of the PV loop correlates with myocardial oxygen consumption within the same heart, it does not necessarily permit direct comparisons of oxygen consumption across different hearts. Consequently, our reference to the PV loop area pertains to its utility in estimating myocardial work within each patient rather than drawing direct comparisons between individuals.
Conclusions
RV myocardial work indices can be used in the routine clinical assessment of patients with PH or advanced heart failure. Further studies are required to establish whether this technique may be of clinical value, improving the non-invasive understanding of pathophysiology, prognosis, and response to therapies in all such patients.
Abbreviations
| CO: | cardiac output |
| dPAP: | diastolic pulmonary artery pressure |
| GCW: | global constructive work |
| GLS: | global longitudinal strain |
| GMW: | global myocardial work |
| GWE: | global work efficiency |
| GWI: | global work index |
| GWW: | global wasted work |
| mPAP: | mean pulmonary artery pressure |
| PAWP: | pulmonary artery wedge pressure |
| PH: | pulmonary hypertension |
| PV: | pressure–volume |
| RHC: | right heart catheterization |
| RV: | right ventricular |
| sPAP: | systolic pulmonary artery pressure |
| SVi: | stroke volume index |
| TAPSE: | tricuspid annular plane systolic excursion |
| TR: | tricuspid regurgitation |
Supplementary materials
The supplementary materials for this article are available at: https://www.explorationpub.com/uploads/Article/file/101252_sup_1.pdf.
Declarations
Author contributions
MA: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. CDL, LS, SS, AG, AT, GT, CS, BP: Data curation, Investigation, Writing—review & editing. CK: Formal analysis. SG: Conceptualization, Validation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study complies with the Declaration of Helsinki. Ethical approval for this study is not required as this is a retrospective study.
Consent to participate
Consent to participate in this study is not required as this is a retrospective study.
Consent to publication
Not applicable.
Availability of data and materials
The data of this manuscript could be available from the corresponding authors upon reasonable request.
Funding
Not applicable.
Copyright
© The Author(s) 2025.
Publisher’s note
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.