Abstract
This is a case of remarkable alpha-fetoprotein in a female patient with known cryptogenic liver cirrhosis. Both ultrasound and triphasic computed tomography (CT) abdomen cannot diagnose or exclude hepatocellular carcinoma (HCC). It turns out to be a case of portal vein thrombosis and hepatic pseudo-infarction. It is better to postpone the therapeutic intervention, whether surgical or chemotherapeutic, in cases not confirmed to be HCC for at least 3 months to avoid misdiagnosis of hepatic pseudo-infarction.
Keywords
Remarkable alpha-fetoprotein elevation, portal vein thrombosis, liver cirrhosis, liver pseudo-infarction, case reportIntroduction
Alpha-fetoprotein (AFP) is an important biomarker for the diagnosis of hepatocellular carcinoma (HCC). The serum expression levels of AFP in many patients with HCC are increased, and a persistently increased AFP level is a risk factor for HCC progression. Two-thirds of HCC patients secrete AFP, and these patients exhibit increased levels of AFP; hence, AFP is still extensively applied for the diagnostic screening of liver cancer [1]. However, the expression of AFP also increases during liver regeneration in active viral hepatitis and cirrhosis, resulting in false-positive AFP screening results [2, 3]. Still, the addition of the AFP indicator during ultrasound assessment can increase the sensitivity of tumor detection [4].
The patients with AFP > 400 ng/mL had larger tumors and up to 65.9% of the patients had vascular invasion. The 5-year overall and disease-free survival was significantly lower than the patients with < 20 ng/mL AFP. High levels of AFP > 9,000 ng/mL and > 14,000 ng/mL warrant an upstage of the diseases for disease-free and overall survival, respectively [5].
AFP is useful for determining prognosis and monitoring therapy for HCC [6]. The concentration of AFP is a prognostic indicator of survival. Elevated AFP concentrations (> 10 μg/L) and serum bilirubin concentrations greater than 2 mg/dL are associated with a decreased survival time [7].
In nonpregnant women and men, elevated levels are seen in cancers, other than liver cancer as testicular and ovarian carcinoma [8]. Elevated maternal blood AFP levels imply a significant risk of having congenital disabilities; hence, further evaluation may be required to assess the level of risk [9], however, this may be an increased risk of obstetric complications like premature membrane rupture, placenta accreta, and increta [10].
Case report
A female patient, 76 years old, working as a journalist, is known to have liver cirrhosis of unknown etiology, splenomegaly, and portal hypertension. She presented with fever and abdominal pain early in the year 2021. On examination, there are multiple spider nevi along the upper chest with palmer erythema; hepatomegaly with sharp edge and firm consistency, and splenomegaly 5 cm below the costal margin were found. CBC showed mild microcytic hypochromic anemia (10 gm/dL) but with normal white blood cell count and platelet count. Alanine transaminase (ALT) was elevated 194–140–32 U/L (normal value: 0–33 U/L) and aspartate aminotransferase (AST) 120–94–30 U/L (normal value: 0–32 U/L), however, both liver enzymes normalized after a few weeks. Albumin 3.8 g/dL (normal value: 3.5–5.2 g/dL), prothrombin concentration was 49.6% once, then came back to 100% within a month. Both anti-HCV and hepatitis B surface antigen (HBsAg) were negative. Serum copper, ceruloplasmin, and 24-hour urinary copper were normal. Autoimmune markers; antinuclear antibodies (ANA), smooth muscle antibodies (SMA), antimitochondrial antibodies (AMA), and LKM1 are negative. AFP showed remarkable elevation (26,000 ng/mL) which was repeated in more than one laboratory at the same time and yielded the same result. Cytomegalovirus-IgM was negative while IgG was positive at 170 U/mL (normal value: > 1 U/mL). Epstein-Barr virus (EBV)-IgM was negative while IgG was positive at 25.3 signal to cut-off (S/Co) ratio (normal value: > 1.1 S/Co ratio). Uric acid was elevated at 6.8 mg/dL (normal value: 2.4–5.7 mg/dL), lactate dehydrogenase (LDH) was 309 U/L (normal value: 135–214 U/L), and creatinine was elevated once at 1.5 mg/dL (normal value: 0.5–1.1 mg/dL) and then came back to normal value. Thyroid functions, electrolytes, lipid profile, and glycosylated hemoglobin were all in the normal range. The abdominal ultrasonographic examination showed a heterogeneous liver with a thrombosed right hepatic vein propagated to the suprahepatic portion of inferior vena cava (IVC) with partial thrombosis of the main portal vein (PV) extended to the confluence with the right PV and chronic calculus cholecystitis. This was confirmed by the Doppler abdominal study. The triphasic abdominal computed tomography (CT) examination showed liver cirrhosis in addition to right hepatic vein thrombosis with attenuation of the right PV and right hepatic lobe patchy areas, in addition to abnormal parenchymal attenuation and enhancement. Segment VIII/V fairly defined area/lesion of early enhancement with no definite delayed washout. There are multiple small splenic hypodense foci, portal hypertension, and chronic calculous cholecystitis (Figure 1).
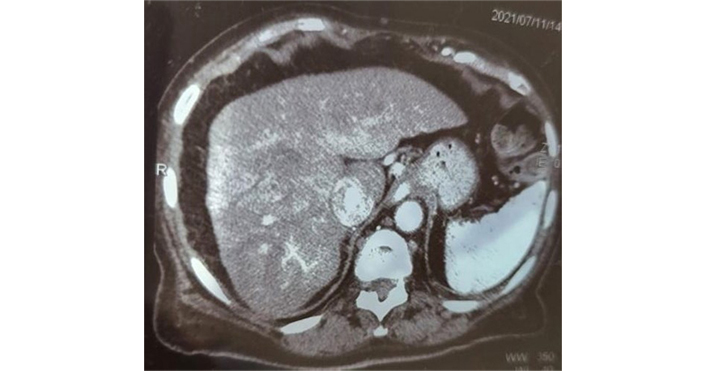
Abdominal CT. Liver cirrhosis with the right hepatic vein thrombosis with attenuation of right PV and right hepatic lobe patchy areas. Segment VIII/V area of early enhancement with no definite delayed washout
The liver biopsy could not be done due to PT prolongation for fear of bleeding and fear of track metastasis. Based on both ultrasonography and CT reports and the marked AFP elevation, a diagnosis of HCC on top of liver cirrhosis could not be ruled out and the patient preferred to take oral targeted therapy; sorafenib (Nexavar), protein-tyrosine kinase inhibitors, as a treatment for her condition in a dose of 400 mg every 12 h. Pretreatment MRI would not add more information or change the line of therapy. We could not confirm the PV thrombus nature whether malignant or hematologic. Adding to this point, there is a prolongation of PT and there is a fear of bleeding if an anticoagulant is added to the targeted therapy. She started the medication and one month later, she developed right calf vein thrombosis (DVT), superficial thrombophlebitis of the left superficial saphenous vein with bilateral marked subcutaneous edema, and sluggish venous flow as proofed by venous duplex ultrasonographic study. She complained of paresthesia in her both lower limbs (LLs) and hair loss as a side effect of the chemotherapy. On examination, she developed moderate ascites and was admitted to the hospital. Nexavar was discontinued and the patient improved on diuretics, albumin, and anticoagulation therapy. Her AFP was still high (20,000 ng/mL). On discharge from the hospital, she received liver support and low-dose diuretics for her ascites and LL edema. On the next follow-up visit 1 month later, both the ascites and LL edema disappeared and the patient’s general conditions improved dramatically. The diuretics discontinued. The liver functions remain within normal range. The patient was instructed to repeat the AFP and the CT before the next follow-up visit. AFP dropped dramatically to 3.6 ng/mL and then to 2.5 ng/mL and 2.6 ng/mL and remains within the normal range over 2 years. We believe that the decrease in AFP is due to the improvement of PV thrombosis (PVT) after starting anticoagulation rather than the effect of sorafenib as this drop was associated with the CT image changes, in addition to the short time of therapy (one month). The triphasic CT abdomen showed liver cirrhosis with right hepatic vein thrombosis and hepatic veins attenuation without any right hepatic lobe patchy areas. To confirm the CT findings, we ordered a dynamic MRI that showed right hepatic vein thrombus and attenuated right PV in addition to right hepatic lobe patchy areas of abnormal signal and enhancement (VIII/V); however, no areas of delayed contrast washout suggestive of HCC (Figure 2).
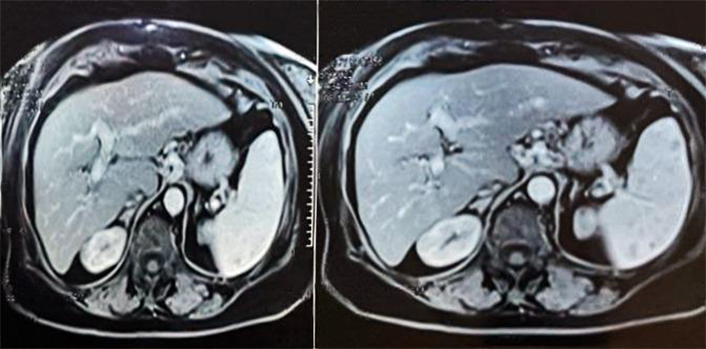
Dynamic MRI. Right hepatic vein thrombus and attenuated right PV in addition to right hepatic lobe patchy areas of abnormal signal and enhancement (VIII/V)
The patient is doing well with excellent general condition on liver support only and diuretics on and off as needed over nearly 3 years now. We are following the patient up with abdominal ultrasonography, duplex study, and AFP.
It is the first time for us to face marked AFP elevation by thousands value with patchy heterogeneous hepatic area caused by portal and hepatic veins thrombosis due to hepatic pseudo-infarction. This can be mistaken for an HCC diagnosis.
Discussion
Hepatic pseudo-infarct (Zahn’s infarct) represents a hepatic area of marked congestion associated with atrophy of the parenchyma but without coagulation necrosis [11]. Hepatic infarction due to PVT was found in patients with liver cancer, cirrhosis, or chronic pancreatitis [12].
Zahn’s infarct has been observed in the setting of various vascular processes, including occlusive phlebitis in PV radicles [13], PVT [14], PV thromboembolism [15], and tumor-induced stenosis of intrahepatic vessels [16]. Macroscopically, the lesions may turn bluish-red, leading to the term “cyanotic atrophy” [11].
We review the literature for marked elevation of AFP with PVT. Only there is a single case report from Japan published in 1996 [17]. This is a case of an old man with liver cirrhosis in whom a PV thrombus was found to be the cause of a marked elevation in serum AFP, 91,000 ng/mL, and liver mass was discovered during the workup. The mass gradually regressed, and the AFP concentration simultaneously decreased to 163 ng/mL. However, because HCC could not be ruled out, a partial hepatectomy was performed where PVT surrounded by the fibrosis associated with liver cirrhosis was found, with no neoplastic lesion on histologic examination. This is the same situation we faced in our case; however, no surgical intervention was done.
It is of utmost importance to follow up with patients with liver cirrhosis and PVT with marked elevation of AFP (> 20,000 ng/dL), especially in cases when the image cannot rule out HCC diagnosis for at least 3 months by duplex ultrasonography, triphasic CT and AFP level before you decide to start treatment, whether chemotherapy or surgery. This is to avoid the misdiagnosis of hepatic pseudo-infarction with HCC and to avoid exposure of cirrhotic patients to unneeded therapeutic interventions.
Abbreviations
| AFP: | alpha-fetoprotein |
| CT: | computed tomography |
| HCC: | hepatocellular carcinoma |
| LLs: | lower limbs |
| PV: | portal vein |
| PVT: | portal vein thrombosis |
Declarations
Author contributions
MTE: Conceptualization, Data curation, Methodology, Supervision, Writing—review & editing. MHH: Conceptualization, Formal analysis, Writing—review & editing. YAA: Software, Validation, Writing—review & editing. GME: Investigation, Supervision, Project administration, Writing—review & editing. AAE: Software, Visualization, Writing—review & editing. MDE: Data curation, Validation, Writing—review & editing. All authors contribute equally like the corresponding author in creating the idea of the article, gathering the information, drafting and writing, reviewing and editing the manuscript in the final shape. All authors agree with the content of the manuscript.
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was waived by the local Ethics Committee of Theodor Bilharz Research Institute in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Consent to participate
Informed consent to participate in the study was obtained from the participant.
Consent to publication
Informed consent to publication was obtained from the participant.
Availability of data and materials
The datasets that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
Not applicable.
Copyright
© The Author(s) 2024.