Affiliation:
1Hospital Regional de Comodoro Rivadavia, Comodoro Rivadavia, Chubut 9000, Argentina
ORCID: https://orcid.org/0009-0001-3022-0667
Affiliation:
1Hospital Regional de Comodoro Rivadavia, Comodoro Rivadavia, Chubut 9000, Argentina
ORCID: https://orcid.org/0009-0005-8462-683X
Affiliation:
2Oral Medicine Service, Hospital Señor del Milagro, Salta 4400, Argentina
ORCID: https://orcid.org/0000-0002-8041-5657
Affiliation:
2Oral Medicine Service, Hospital Señor del Milagro, Salta 4400, Argentina
ORCID: https://orcid.org/0000-0002-5269-3254
Affiliation:
3Oral Medicine Department, Facultad de Odontología, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
Email: ggilligan@unc.edu.ar
ORCID: https://orcid.org/0000-0002-5201-1444
Explor Digit Health Technol. 2024;2:279–290 DOI: https://doi.org/10.37349/edht.2024.00028
Received: June 03, 2024 Accepted: August 30, 2024 Published: October 10, 2024
Academic Editor: Andy Wai Kan Yeung, The University of Hong Kong, China
The article belongs to the special issue Digital Health Technologies for the Early Detection of Oral Cancer
Geographic areas like Argentine Patagonia face significant barriers in the fight against oral cancer due to great distances, extreme weather conditions, and a shortage of specialists. These factors contribute to delayed diagnosis and treatment, adversely affecting patient outcomes. The aim of this study was to describe a pilot project to establish the telemedicine network of Chubut (Argentine Patagonia) for the early diagnosis of oral cancer. This perspective study also aimed to describe the advantages and disadvantages of using this tool in remote areas with limited access to healthcare services. Healthcare professionals, including nurses, dentists, doctors, and healthcare workers, were trained in the early diagnosis of oral cancer and high-risk oral lesions by five specialists in Oral Medicine, who traveled throughout Argentine Patagonia. Additionally, training was provided on the use of smartphones to obtain clinical images and data for remote consultations via telemedicine with a specialized center. Over 2,000 km were traveled, and more than 100 healthcare professionals were trained in six towns and localities in Patagonia, Argentina, encountering various limitations for the use of telemedicine in remote areas, such as connectivity issues. The first telemedicine network of Patagonia for the diagnosis of oral cancer was created and is now operational, receiving teleconsultations and referrals from the professionals trained during the journey. This study highlighted that telemedicine is an important tool to overcome geographical barriers and improve access to medical care, especially in remote areas. It promotes agility and speed in referrals and optimizes the available resources of the health system. Future studies should analyze the impact of telemedicine in decreasing the delay of oral cancer diagnosis in Southern Argentina.
Telemedicine has emerged in recent decades as a highly useful tool in the provision of healthcare services particularly in remote areas and under challenging climatic conditions. In regions such as South America and the Caribbean, limited access to healthcare professionals and conventional medical facilities often delays the diagnosis of diseases, including oral cancer [1]. Furthermore, extreme weather conditions can hinder patients’ ability to travel to specialized centers. Telemedicine for residents of forested and mountainous areas facilitates rapid access to healthcare and enhances patient satisfaction [2].
In the context of oral cancer, virtual consultations enable patients to show oral lesions to healthcare professionals, thus facilitating early diagnosis without the need for physical travel or optimizing resources for rapid referral to specialized centers staffed by oral medicine and pathology specialists [3, 4]. However, the successful implementation of telemedicine networks in the context of oral cancer requires training for healthcare professionals in the recording of useful data that can aid in referral or decision-making to achieve early diagnoses. Moreover, awareness campaigns can promote the adoption of this technology by highlighting its benefits and overcoming barriers of distrust [5].
Previous experiences in teledentistry for oral medicine have shown promising results in Brazil. The “Telessaude Brasil Redes” telehealth platform in the state of Parana was well-received by users who rated the service positively. However, there were some limitations regarding the quality of clinical information provided during teleconsultations and the need to standardize teleconsultation criteria, identifying the most common barriers to its use. Telemedicine in oral medicine appears to be a valuable tool for improving oral health care delivery, with significant growth potential due to its relevance in public services and its ability to reduce inequities [6]. Another study from Brazil addressing telediagnosis for oral lesions in remote areas also encourages the development of telemedicine networks, as telediagnosis for oral lesions has the potential to enhance the quality of primary health care by bridging the gap between primary and specialized healthcare [7]. In other regions of the world, where oral cancer is a prevalent concern, telemedicine for oral cancer diagnosis has been developed to achieve early diagnosis of oral squamous cell carcinoma (OSCC). Mobile health approaches have enabled specialists to connect with rural populations. Trained healthcare providers were able to reach out to the population, and electronic data capture facilitated efficient follow-up. Furthermore, the program proved to be very cost-effective [8].
Argentine Patagonia is one of the southernmost regions in the world, encompassing nearly all of Southern Argentina. Covering an area of approximately 673,000 km2, it constitutes a vast expanse of steppe and desert extending from latitude 37° to 51° S. It is roughly bounded by the Andes to the west, the Colorado River to the north, the Atlantic Ocean to the east, and the Strait of Magellan to the south. Despite being one of the largest regions in Argentina, it has the lowest population density in the country. The official 2010 census recorded a population-to-territory ratio of 2.5 inhabitants per km2, marking the lowest rate in the country. Argentine Patagonia comprises four states: from north to south, Neuquén, Chubut, Santa Cruz, and Tierra del Fuego. Chubut, along with Santa Cruz, is one of the most extensive states in Argentine Patagonia. According to the latest population census conducted in 2022, Chubut has 592,621 inhabitants within 224,302 km2, resulting in a population density of 2.6 inhabitants per km2. While oral cancer data throughout Latin America are underreported [9], recent (yet unpublished) information suggests an increase in oral cancer cases in Argentine Patagonia, with advanced diagnostic stages and very low survival rates.
The aim of this study is to describe a proposal and outline the experience of a pilot study aimed at organizing the telemedicine network of Patagonia for the early diagnosis of oral cancer in this remote region of Argentina. In addition to detailing the organizational framework for its creation, this study aims to describe the advantages and disadvantages of using this tool in inhospitable locations from geographical and climatic perspectives.
The present project received approval and academic endorsement from the National University of Patagonia San Juan Bosco, Faculty of Health Sciences (No. 1290/23), and the Ministry of Health of the Province of Chubut, Argentina (No. 4850/2023).
Facilitate access to specialized medical care: Apply telemedicine to connect patients in remote areas of Argentine Patagonia with specialists in oral cancer diagnosis.
Promote early diagnosis: Provide remote diagnostic tools to identify possible cases of oral cancer in their early stages.
Offer education and specific training in the use of telemedicine tools: Train local healthcare personnel in the proper use of telemedicine for the diagnosis and monitoring of oral cancer cases.
Create a care network trained for the early recognition of oral lesions involving general dentists, physicians, nurses, and health collaborators.
Provide information on primary preventive measures for OSCC through community talks (primarily targeting adolescents and young adults who are starting habits such as tobacco and alcohol consumption).
Selection of appropriate technology: Reliable and secure telemedicine platforms were identified to establish communication among healthcare professionals. The free image-sharing application (WhatsApp), which has been used in similar experiences worldwide, was chosen for the initial referral from the remote consultation site to the specialized center. Subsequently, if the oral medicine specialists working at the specialized center had any doubts or considered the teleconsulted case challenging in diagnosis, asynchronous teleconsultations were conducted via a telehealth system with specialists located in different parts of the country, including hospitals and university diagnostic centers. All teleconsulted cases are recorded on the Telehealth platform (the official telehealth and remote communication system from the Ministry of Health, República Argentina).
Establishment of collaboration networks: Partnerships were formed with local stakeholders and specialists in OSCC diagnosis, who also received telemedicine training to provide remote assistance.
Training and capacity building: Training sessions were organized for local healthcare staff on the use of telemedicine and remote OSCC diagnostic methods. The experience was approached through the following activities to be carried out in each visited location or place.
Oral medicine care and diagnostic procedures.
Recording of high-risk OSCC patients.
Preparation of clinical material for training, this included a portfolio of clinical photographs on various presentations of oral potentially malignant disorders (OPMDs) and OSCCs.
Training provided to dentists interested in joining the telemedicine network, including basic instruction in collecting essential data through protocols for urgent patient referrals to specialized oral cancer diagnosis centers.
Meetings and training with non-dentist healthcare personnel: Addressing guidelines for managing consultations related to oral lesions and addressing high-risk OSCC patients. An individual was classified as a high-risk OSCC patient if they met three or more of the following criteria: a) heavy drinking, b) heavy smoking, c) HPV infection, d) clinical conditions indicative of OPMD or chronic wounds not healing within 2 weeks, e) low fruit and vegetable consumption, f) family history of upper aerodigestive tract cancer, g) poor oral hygiene, h) chronic trauma (e.g., sharp teeth, ill-fitting dentures), i) intense sunlight exposure, or j) comorbidities associated with immunological diseases. This classification is based on risk factors for oral cancer identified in previous studies in Argentina by Piemonte et al. [10].
All these issues and criteria related to the increased risk of oral cancer from a multifactorial perspective were reinforced in each training session for professionals, dentists, and healthcare providers, as well as in community talks provided to the population.
Informational talks were organized for the population on OSCC prevention emphasizing primary and secondary oral cancer preventive strategies.
Self-examination as a preventive measure.
A systematic registry of those cases of OPMD and OSCC that were diagnosed via telemedicine was conducted and is currently ongoing, assessing the effectiveness of this tool in early diagnosis.
Although this telemedicine network is primarily established to improve access to the healthcare system for the Patagonian community (mainly affected by OPMD or OSCC), professionals or healthcare providers who consult on cases of oral lesions can also consult on cases of non-cancer suspicious oral lesions, benign lesions, and refer them to the specialized center at the Comodoro Rivadavia Hospital for diagnosis and treatment.
The recruitment of the community that attended the community lectures provided by the oral medicine specialists was handled by the healthcare staff of each hospital or health outpost visited during the journey through the state of Chubut. Each health institution invited community members interested in training on oral cancer awareness. Additionally, the population was recruited through posters, messages on social media, and especially through messaging to rural residents via radio: AM frequency, Radio Nacional, at 9:30 AM and 5:00 PM.
The free image-sharing application (WhatsApp), which has been used in similar experiences worldwide, was chosen for the initial referral from the remote consultation site to the specialized center. Subsequently, if the oral medicine specialists working at the specialized center had any doubts or considered the teleconsulted case challenging in diagnosis, synchronous teleconsultations were conducted via a telehealth system with specialists located in different parts of the country, including hospitals and university diagnostic centers. All teleconsulted cases are recorded on the Telehealth platform (Telehealth and remote communication, Ministry of Health of Argentina—https://www.argentina.gob.ar/salud/telesalud). The Telehealth Coordination of the Ministry of Health has the mission to develop and implement a national and federal public telehealth policy through the use of information and communication technologies, under standards of interoperability, security, and privacy of information, as a measure of equity in access to health for the inhabitants, reducing the burden on the healthcare system. It is noteworthy that the Patagonia oral cancer telemedicine network was the first experience where this network was used in the field of dentistry.
Improvement in access to medical care: Increase in the number of patients receiving timely evaluations and diagnoses.
Reduction of morbidity and mortality: Decrease in the late diagnosis of OSCC due to early diagnosis.
Empowerment of the local medical community: Professionals and healthcare providers. Training of healthcare staff in the use of innovative medical technologies.
Identification of obstacles and solutions: Identification of challenges in the implementation of telemedicine and proposals to overcome them.
Access to technology and connectivity
Insufficient technological infrastructure: In remote areas, especially in geographic areas at the foot of the Andes Mountains, lack of access to high-speed internet or inadequate technological equipment could hinder the effective implementation of telemedicine.
Device availability: Lack of access to electronic devices such as computers, tablets, or smartphones by patients or healthcare centers may limit the adoption of telemedicine.
Climatic factors (e.g., intense snowstorms during winter) cause mobile data system collapses resulting in transient loss of connectivity.
Training and acceptance
Healthcare staff training: Training healthcare staff in the proper use of technology and the interpretation of remotely obtained data may require time and resources.
Community acceptance: There may be resistance or lack of confidence from the community towards remote diagnostic methods, which could affect participation and adherence to the program.
Privacy and regulations
Data security and privacy: Ensuring the protection of confidential medical information during remote consultations is crucial and can be a technical challenge.
Health regulations and policies: Complying with local, state, or national regulations regarding remote medical practice and telemedicine may require adaptations and specific monitoring.
Diagnostic limitations
Limitations in physical examination: Lack of physical presence may limit the ability to perform detailed examinations, which could affect diagnostic accuracy.
Need for complementary examinations: Some cases may require additional diagnostic tests that are not available remotely, which could reduce compliance and delay diagnosis or treatment.
Sustainability and financing
Long-term sustainability: Dependence on continuous funding to maintain telemedicine infrastructure and services.
Associated costs: The costs of implementing and maintaining technology and training could be high and require adequate financial support.
Cultural and linguistic aspects
Cultural and linguistic diversity: The cultural and linguistic diversity of the region may require specific adaptations in communication and the provision of telemedicine services (native and indigenous peoples).
These limitations are important to consider when planning and implementing a telemedicine project for the early diagnosis of OSCC, as they could affect the feasibility, effectiveness, and scope of the program. It is crucial to address these limitations with specific strategies to mitigate their impacts and ensure the success and sustainability of the project.
The experience took place from November 12th to 22nd, 2023, with active participation from all five authors of this manuscript. The main contributors were dentists, and graduates from different universities in Argentina: two with residency in Salta (a Northern Argentine state), one in Córdoba, and two local coordinators residing in Comodoro Rivadavia, Chubut. All participants are specialists or trainees in oral medicine.
Departing from Comodoro Rivadavia, a total distance of 2,921 km was traveled to reach the nine established localities across the state of Chubut for the initial project, equipped with the necessary tools for each scheduled activity (Figures 1 and 2).
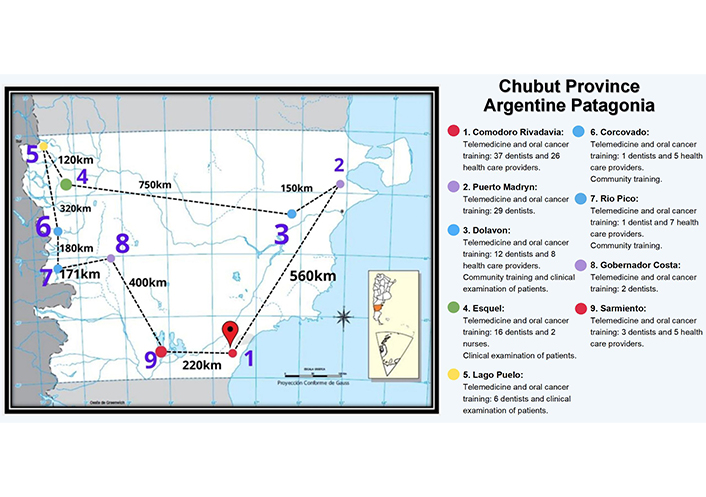
Map of Chubut (state of Argentine Patagonia)—reproduced itinerary of the different locations visited. Left: Chubut state (Patagonia Argentina). Location of the different places where scheduled activities were carried out, route taken, and distance between each of them; right: details of activities and attending professionals
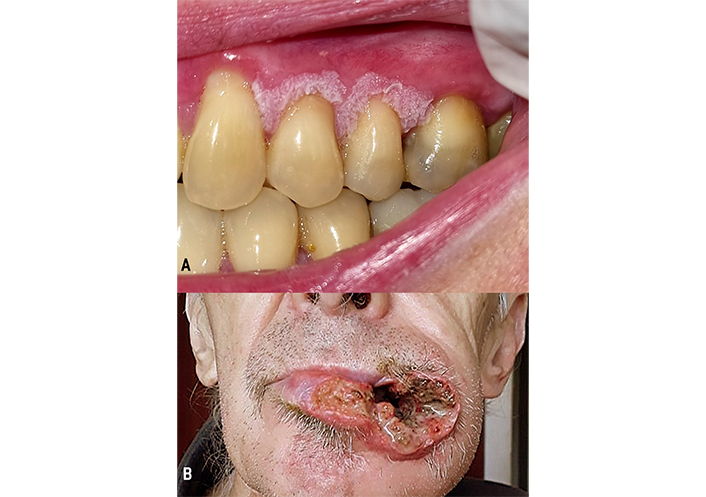
Cases recorded during clinical activity. (A) Verrucous Leukoplakia was diagnosed in a rural worker from the town of Esquel in the context of a clinical examination of the general population; (B) photograph sent to the telemedicine network 25 days after its creation: The patient who lived 450 km from Comodoro Rivadavia’s Hospital where the telemedicine network was coordinated. The quick referral to the oral medicine service allowed the histopathological diagnosis of a lip squamous cell carcinoma. The patient revealed that the lesion persisted for two years
During the activity, a total of 148 professionals were trained in the topics covered in the “Training” section, focusing on telemedicine and its role in optimizing the referral process. Among them, 54 non-dentist healthcare professionals received training, including radiologists, dermatologists, oncologists, physicians, nurses, kinesiologists, nutritionists, dental technicians, medical students, and surgeons.
The topics covered in the community lectures were: general information on oral cancer, early signs of oral cancer, risk factors for oral cancer, and the importance of early diagnosis and early consultation with dentists trained in oral medicine or active participants in the novel telemedicine network. Furthermore, the existence of the telemedicine network was emphasized to the community each attendee belonged to.
Figure 1 illustrates the map of Chubut state and the visited localities. Stomatological care was provided in three localities, where 32 patients were reviewed, identifying a single case with lesions compatible with proliferative verrucous leukoplakia (Figure 2A). Figure 3 shows cases of several landscapes encountered during the journey, spanning remote locations across Patagonia, from coastal areas and wind turbines to the Andean foothills in challenging climates. It also depicts training sessions for healthcare assistants, patient care activities, and visits for telemedicine training in rural hospitals.

Images of the Chubut state, activities carried out, active team and Health Community Workers of rurality. (A) Patient care in the town of Esquel; (B) auditorium of attending professionals in Comodoro Rivadavia city; (C) cliff of the Patagonian Plateau at the foot of the Chubut River, Los Altares Route, Province Route 25; (D) oral medicine specialists, rural dentists, and health community workers from the mountain town of Río Pico; (E) windmills, YPF wind farm, located southeast of the Chubut state, National Route 3; (F) “El Doradillo” beach, a town of Puerto Madryn, Western Chubut (next to the Atlantic Ocean); (G) Corcovado River Valley, Province Rout 17, Patagonian Mountain Range, Eastern Chubut (next to the Andes Mountain)
This study describes a pioneering initiative in developing a telemedicine network for early OSCC diagnosis in a remote region of Argentine Patagonia. Overcoming geographical, cultural, linguistic, and access barriers to dental care through telemedicine technologies was crucial in achieving the primary goal of enhancing early OSCC detection and reducing associated morbidity and mortality [8, 11–13].
As described earlier, the impacts and outcomes of the activities conducted in this initiative, along with the functioning of the telemedicine network, require prompt evaluation. This assessment will systematically analyze the activities to ascertain whether the telemedicine network successfully enhanced early oral cancer diagnosis in Argentine Patagonia. Additionally, it aims to identify any weaknesses in the system to optimize resources and ensure timely referrals. This discussion section will explore some concepts relevant to the analysis.
The use of telemedicine technology in remote areas facilitates access to health care. At present, the gold standard in screening oral suspicious lesions is the conventional oral examination, while the gold standard in the diagnosis is the scalpel biopsy. Several adjunctive diagnostic technologies have been developed in recent decades to aid in detecting OSCC at early stages [14]. Professional delays could be avoided with the proper use of scientific knowledge and diagnostic tools such as telemedicine. Telemedicine enhances healthcare accessibility, identifies high-risk patients, manages referrals, and provides preventive and remote therapeutic support at a reasonable cost. This is particularly beneficial for new graduates working in rural areas [3]. This could be beneficial for developing countries in Latin America [1]. Telemedicine has been a widely accepted method to ensure the safety of both patients and healthcare providers amid the COVID-19 pandemic and to assist patients in receiving consultations, urgent treatments, or follow-ups [15, 16]. A systematic review addressing this issue explored the challenges, opportunities, and equipment required to use telemedicine in remote areas. These results revealed some challenges including harsh weather conditions, Internet connectivity problems, difficult equipment transportation, and ethical issues. On the other hand, telemedicine also has many benefits, such as cost and time savings for patients, improving patients’ quality of life, and improving patient satisfaction [2]. These limitations and benefits were evident during this practice. In mountainous areas near the Andes Mountains, difficulties with Wi-Fi networks and connectivity were prominent, however, connectivity improved within hospital institutions where patients usually arrive. The limited availability of electronic devices and challenges related to community acceptance of telemedicine were also noted. State support and financing for such projects must first ensure the connectivity of users (patients, referring practitioners, and specialists) and the availability of technological resources for all involved parties. Roine et al. [17] demonstrated convincing evidence of the effectiveness of telemedicine in certain medical areas. Their study also highlighted the benefits of electronic referrals, which enable interactions between primary and secondary healthcare providers [17]. These studies, combined with our experience, underscore that despite some limitations, the use of telemedicine could bridge the gap between primary healthcare and specialists, particularly in the field of oral medicine.
Another of the most notable achievements of this project was the successful training of a large group of local professionals in the effective use of telemedicine tools for the early detection of OSCC and OPMD, and the subsequent referral of suspicious oral lesions to specialized centers [11, 18]. This training was essential to empower the different health professionals who practice primary care, improving their ability to properly identify and refer cases of OSCC in the early stages. A key aspect of this project was the emphasis on continuing education and establishing a strong network of collaboration between primary care professionals, including dentists, general practitioners, nurses, and community health workers (non-dentist healthcare personnel). The latter are of vital importance in daily practice [11, 19]. This transdisciplinary collaboration allowed a comprehensive evaluation of patients and better coordination in the referral and treatment procedures [19, 20]. In a recent work from India, a well-structured training module to impart knowledge and upskill the community health workers for early detection of OSCC, creating awareness on disease prevention was highlighted [19]. Our experience highlighted the interest of non-dentist healthcare personnel in training for the early detection of oral cancer and initiating rapid consultations with local dentists to begin referrals to specialized centers. Given the widespread knowledge limitations regarding oral cancer, future studies should evaluate whether the training of non-dentist healthcare personnel has a tangible impact on the cases referred through telemedicine and the interdisciplinary collaboration among all participants in the telemedicine network.
Since this experience is recent, we do not have objective data to robustly assess the benefits or the success achieved, like the empowerment of trained professionals or healthcare providers. However, it is important to highlight that the aforementioned empowerment is based on several essential features. Firstly, continuous education and specialized training enable professionals to stay updated with medical and technological advancements, thereby improving the quality of care provided. Secondly, autonomy in clinical decision-making fosters an environment where professionals can apply their judgment and experience effectively, leading to better patient outcomes. Additionally, access to adequate resources and tools, such as telemedicine platforms and professional support networks, strengthens their ability to handle complex cases and collaborate with colleagues from various specialties. Lastly, the recognition and appreciation of the work of healthcare professionals, along with a positive and supportive work environment, are crucial for maintaining their motivation and well-being. These foundations not only enhance job satisfaction but also positively impact the health of the community served. These impact indicators could be useful in the future when evaluating and measuring the empowerment of healthcare providers during our experience.
In terms of social impact, the telemedicine network for the early diagnosis of oral cancer in Argentine Patagonia has the potential to significantly transform medical care in remote regions, improving clinical outcomes and quality of life for patients. Furthermore, this project could serve as a replicable model for other geographically challenging areas in Argentina and Latin America [1]. Our experience in Argentine Patagonia highlights the importance of transdisciplinary practice, continuous training, and cultural adaptation for the success of similar initiatives in the future.
The clinical applications of telemedicine could be used in the early detection of OSCC. However, the evidence of the effectiveness of such potential benefits is not yet conclusive. The lack of standards and the resistance to change may represent major challenges in catching up with other telemedicine applications in different specialties [16]. The analysis of the limitations and benefits of this project, completed in 2023, serves as a starting point. Currently, the telemedicine network is actively operating with weekly referrals from various geographic areas where professional training was conducted last year. Further studies will evaluate the referral network, considering aspects such as the limitations of telemedicine use, the legal framework, referral times, barriers to referral (including climate, distance, transportation, and delayed diagnosis by professionals or patients), and a satisfaction survey of patients and professionals to improve the resources involved in the Network’s operation. Additionally, the re-training of involved professionals is essential. Table 1 analyzes the main limitations of this project.
Evidenced limitations of the use of telemedicine in the project
| Limitation raised | The situation revealed during the experience |
|---|---|
| Insufficient technological infrastructure: In remote areas, lack of high-speed internet access or lack of adequate technological equipment could hinder the effective implementation of telemedicine. | In areas close to the Andres Mountain Range, we found geographical regions without any signal and/or with weak signals in medical care places such as dispensaries or hospitals. |
| Device availability: Lack of access to electronic devices such as computers, tablets, or smartphones by patients or healthcare facilities may limit the adoption of telemedicine. | All the care centers surveyed had access to electronic devices: computers and tablets or smartphones by the community. |
| Training of health personnel: Training health personnel in the proper use of technology and the interpretation of data obtained remotely may require time and resources. | Fortunately, the health professionals interviewed showed so much desolation and lack of support in the diagnosis of oral lesions, that they showed a lot of interest and motivation in the formation of the network and training in the discipline and the referral protocols for the use of telemedicine. |
| Community acceptance: There may be resistance or lack of trust on the part of the community towards remote diagnostic methods, which could affect participation and adherence to the program. | There was no evidence of resistance, quite the opposite. Patients agreed that telemedicine can be an effective tool that facilitates referral to specialists and optimizes specialized care resources. |
| Data security and privacy: Ensuring the protection of confidential medical information during remote consultations is crucial and can be a technical challenge. | Trained healthcare professionals recognized the relevance of data security and privacy and the use of medical materials for professional and scientific purposes only. However, we believe that it is a challenge and that more free smartphone applications should be generated that ensure the confidentiality of shared data. |
| Health regulations and policies: Complying with local, state, or national regulations regarding remote medical practice and telemedicine may require accommodations and specific monitoring. | Little development of legislation in the field of telemedicine. |
| Limitations on physical examination: Lack of physical presence may limit the ability to perform detailed examinations, which could affect the accuracy of the diagnosis. | This is a fact addressed during oral medicine training and telemedicine training for health professionals, which is the ability of the acting professional to not only take a good quality photograph but also to provide key data requested by the specialist consulted remotely about clinical and semiological data of the patient that are necessary to guide towards a diagnosis and treatment. |
| Need for complementary tests: Some cases may require additional diagnostic tests that are not available remotely, which could delay diagnosis or treatment. | Little training of professionals in performing oral biopsies. |
| Long-term sustainability and associated costs. | It was evidenced that as long as the program is formally or informally supported by the healthcare system, sustainability over time would not be an obstacle. This long-term sustainability must be accompanied by the political decisions of the governments, who continue to support the operation of the telemedicine network as a priority among health policies. The constant reevaluation will also allow us to visualize long-term sustainability, being able to optimize its operation. |
| Cultural and linguistic aspects: The cultural and linguistic diversity of the region may require specific adaptations in the communication and delivery of telemedicine services. | Total acceptance of the members of the native communities who attended the community talks (with the presence of native peoples and chiefs of the “Mapuche” tribe). Although they are familiar with the virtual talks/training that come from their social-ethnic activity, they were receptive to innovative tools in the field of health for the attendees (and the other Mapuche communities). |
Finally, the exchange of clinical data and the modality of teleconsultation for subsequent referral to a specialized center were conducted using free messaging smartphone applications not specifically developed for telemedicine purposes. Although the telemedicine network has proven useful so far, several applications are designed ad hoc to review clinical images of oral lesions, with a special emphasis on the early detection of OPMD and OSCC. Haron et al. [21] evaluated a specific digital tool, highlighting that referral decisions are highly comparable to in-person clinical examinations, demonstrating that telemedicine tools facilitate the early management of high-risk lesions. Future studies should also validate the effectiveness and evolution of the telemedicine network in Patagonia, including an analysis of its specificity for early identification of suspicious lesions and a comparison with in-person examinations. Additionally, further exploration is needed to assess the impact of this telemedicine network on reducing delays in oral cancer diagnosis in Southern Argentina.
Telemedicine could represent a key tool for overcoming geographical barriers and improving access to specialized medical care, particularly in isolated regions like Patagonia. The implementation of this telemedicine network has the potential to enhance health outcomes, helping faster referrals for cases of OPMD and OSCC. Additionally, the results and records from this network will be valuable for future research specifically evaluating the outcomes and impact of this activity on early diagnosis in the context of oral cancer.
OPMD: oral potentially malignant disorders
OSCC: oral squamous cell carcinoma
RA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing—original draft. AM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing—review & editing. JMPS and IMÁ: Conceptualization, Investigation, Methodology, Project administration, Writing—review & editing. GG: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing—original draft.
The authors declare that they have no conflicts of interest.
The present project received approval and academic endorsement from the National University of Patagonia San Juan Bosco, Faculty of Health Sciences No. 1290/23, and from the Ministry of Health of the Province of Chubut, Argentina, No. 4850/2023.
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
The datasets that support the findings of this study are available from the corresponding author upon reasonable request.
Not applicable.
© The Author(s) 2024.
Open Exploration maintains a neutral stance regarding jurisdictional claims in published maps and institutional affiliations.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Xin-Jia Cai
Eduardo D. Piemonte ... Jerónimo P. Lazos
Kehinde Kazeem Kanmodi ... Jacob Njideka Nwafor
Caique Mariano Pedroso ... Alan Roger Santos-Silva
Márcio Diniz-Freitas ... Pedro Diz-Dios
Gerardo Gilligan ... Eduardo Piemonte
Simon A. Fox, Camile S. Farah
Constanza B. Morales-Gómez ... Víctor Beltrán
Anna Luíza Damaceno Araújo ... Alan Roger Santos-Silva
