Affiliation:
1Oral Diagnosis Department, Piracicaba Dental School, University of Campinas, Piracicaba 13414-903, Brazil
Email: c231631@dac.unicamp.br
ORCID: https://orcid.org/0000-0002-7504-7597
Affiliation:
2King’s College London and WHO Collaborating Centre for Oral Cancer, WC2R 2LS London, UK
ORCID: https://orcid.org/0000-0003-2103-0746
Affiliation:
1Oral Diagnosis Department, Piracicaba Dental School, University of Campinas, Piracicaba 13414-903, Brazil
ORCID: https://orcid.org/0000-0003-2040-6617
Explor Digit Health Technol. 2024;2:291–301 DOI: https://doi.org/10.37349/edht.2024.00029
Received: June 13, 2024 Accepted: September 20, 2024 Published: October 22, 2024
Academic Editor: Andy Wai Kan Yeung, The University of Hong Kong, China
The article belongs to the special issue Digital Health Technologies for the Early Detection of Oral Cancer
Teledentistry has emerged as a promising tool in bridging the gap in healthcare accessibility, particularly in regions like Latin America region, where resources for oral healthcare are often limited. Drawing upon a comprehensive review of literature, this overview assessed the applications and clinical outcomes of teledentistry in diagnosing oral potentially malignant disorders (OPMDs) and oral cancer, highlighting the challenges and opportunities specific to the Latin American context. Moreover, it examined the integration of artificial intelligence algorithms and teledentistry for enhancing diagnostic accuracy, thereby optimizing resource allocation and improving patient outcomes. By elucidating the current landscape and future prospects, this overview provided insights for policymakers, healthcare providers, and researchers, fostering advancements in oral healthcare delivery with the aim of reducing the burden of OPMDs and oral cancer in the Latin American region.
Telemedicine, the practice of remotely diagnosing and treating patients using telecommunications technology, has undergone significant evolution influenced by advances in communication technology, healthcare needs, and regulatory changes [1]. Initially centered around telephone consultations between patients and healthcare providers, telemedicine has expanded with the emergence of the internet and video conferencing technology to include virtual consultations and remote monitoring [2]. The concept of telemedicine dates back to the early 20th century when telephones were first utilized for medical consultations, particularly in rural areas with limited access to healthcare [3]. As computers and the internet advanced, telemedicine incorporated video conferencing and digital imaging technologies, enabling more comprehensive and robust remote consultations and diagnostic capabilities. The development of mobile devices, high-speed internet, and wearable sensors further broadened the scope of telemedicine, facilitating real-time monitoring of patients’ vital signs and health data from remote locations [2].
In recent years, telemedicine has become increasingly integrated into mainstream healthcare systems worldwide, with other health sectors adopting this model of consultation, as evidenced by its implementation in dentistry, known as teledentistry. Teledentistry offers a convenient and efficient means of delivering dental care, particularly in underserved areas with limited access to dental professionals, with the aim of improving oral health outcomes by earlier diagnosis and enhancing patient satisfaction, particularly in cases of oral cancer and oral potentially malignant disorders (OPMDs) [4, 5].
OPMDs represent a group of diseases associated with an increased risk of developing oral cancer [6]. OPMDs are heterogeneous and vary in their progression rates to cancer development. Their diagnosis relies on clinicopathologic analysis to exclude other clinical conditions with similar presentations. Early detection of OPMD is paramount in effectively managing oral cancer, significantly improving treatment outcomes and overall prognosis [7]. Oral cancer is a malignant neoplasm that develops in the lip and oral cavity, with 90% of cases comprising the histopathological subtype squamous cell carcinoma (SCC) [8]. In the Latin American region, incidence rates of OPMD and oral cavity cancer vary from low to high between countries, with socioeconomic factors influencing the mortality rate of oral cancer in this region [9]. Dentists and oral healthcare professionals play a crucial role in identifying and monitoring these diseases during routine oral examinations. Teledentistry, in this context, can enhance the diagnosis and management of OPMD through improved patient access, timely detection and monitoring, cost-effectiveness, patient education, and data-driven decision-making [10].
Telemedicine has been used in a number of countries to improve patient access and lessen the burden on healthcare systems. Developing countries, such as Brazil, have included teledentistry in routine practice, and many feasibility studies have been conducted in this field [11]. Nevertheless, the increased use of telemedicine in Latin America raises concerns such as limited broadband access for low-income populations and lack of appropriate legal regulations for transmitting and storing private data, which must be addressed [12]. The results of previous studies suggested that telehealth can be an effective tool for triage and monitoring of OPMD patients [13]. Also, according to preliminary studies, patients are accepting teledentistry as a remote technology for monitoring patients with head and neck cancer and oral cancer [14]. In this context, this review aimed to report on the advances of teledentistry in the diagnosis of OPMD and oral cancer, highlighting clinical outcomes, as well as highlighting challenges and limitations.
The updated 2020 definition of OPMD identifies it as any abnormality of the oral mucosa that contributes to an increased risk of oral cancer [6]. This group of disorders can manifest within the oral cavity and lip, showing various clinical aspects including variations in size, texture, and color. A total of eleven disorders are included in this group, predominantly diagnosed in middle-aged or elderly males [6]. The overall prevalence of OPMD worldwide is 4.47% and the frequency differs between populations [15]. The main OPMDs encountered in clinical practice in Latin America are oral leukoplakia (OL), oral erythroplakia (OE), and actinic cheilitis (AC). The risk factors associated with these principal OPMDs are related to tobacco use (smoking or smokeless forms), heavy alcohol consumption, and ultraviolet radiation [6]. These risk factors place certain populations at higher susceptibility to developing these conditions.
OL is the most common OPMD, characterized by persistent white plaques in the oral cavity that do not resolve over time and cannot be removed by mechanical means, such as rubbing. OL can be further subclassified into homogeneous and non-homogeneous based on clinical aspects (color and surface) [6]. Another frequently observed disorder is OE, defined as a solitary red patch clinically not characterized as any other definable disease. OE may indicate severe dysplasia, with a higher probability of progressing to oral cancer compared to leukoplakia [6]. AC occurs due to the effect of actinic (solar, predominantly ultraviolet) radiation on exposed areas of the face, predominantly affecting the skin and vermilion of the (lower) lip. It may present as localized or diffuse lesions of white flaking plaques or scaly lesions with interspersed red areas [6]. The different clinical aspects found in this group of disorders can be difficult to diagnose for some dental professionals, and the recognition of OPMD is crucial for detecting people at risk and decreasing the possibility of malignant transformation.
Oral SCC (OSCC) is a malignant neoplasm that develops in the oral cavity and lower lip [8]. The main risk factors for oral cavity SCC include tobacco use (smoking and smokeless), chronic alcoholism, human papillomavirus infection (HPV), and ultraviolet radiation, the latter specifically for lip SCC [7]. The presence of these risk factors predisposes patients to develop these conditions, with those dependent on tobacco and alcohol considered at high risk. Oral cancer is regarded as an important global health issue ranking sixteenth in incidence among all cancer cases in the world [16]. The incidence of oral cancer varies greatly depending on geographic location, with higher rates in developing countries and lower rates in developed countries.
Oral cancer can present with various clinical manifestations, ranging from early to advanced stages. In its early stages, especially in incipient SCC, the disease can manifest as OPMD, with white plaques (leukoplakia), reddish spots (erythroplakia), or a combination of both (erythroleukoplakia lesions) [6]. As the disease progresses clinically, it may manifest as an ulcerated lesion with raised edges that are hard on palpation. The majority of patients with OSCC are diagnosed at an advanced stage, often with neck metastases already present at the time of diagnosis, which significantly contributes to the high mortality rates and poor prognosis of this disease [17, 18]. To reduce mortality rates associated with oral cavity cancer, screening and early detection are crucial interventions that must be implemented in the population through program models designed to identify suspicious or innocuous lesions [19].
Understanding the definition, classification, risk factors, and prevalence of OPMDs and oral cancer underscores the importance of early detection in preventing the progression of oral cancer [7]. Additionally, detecting OPMDs at early stages often leads to less invasive treatment options and better prognoses. Early detection initiatives raise awareness about the risk factors and symptoms of OPMDs, empowering individuals to seek timely medical attention. Therefore, efforts aimed at promoting awareness, implementing screening programs, and providing access to timely healthcare services are essential in combating the burden of OPMDs on public health [7].
Teledentistry, a subset of telehealth, utilizes digital communication and information technologies to remotely deliver dental care, consultation, diagnosis, treatment planning, and education [4, 5]. It allows dental professionals to reach patients who are geographically distant or have limited access to traditional dental facilities, thereby extending oral healthcare beyond physical dental offices and enhancing access to care [20]. It also reduces the delay encountered in obtaining the first consultation.
Various modalities of teledentistry include real-time (synchronous), store-and-forward (asynchronous), remote monitoring, and mobile health [21]. Real-time teledentistry involves live interactive dental consultations and examinations typically conducted through video conferencing platforms. Dentists can assess patients’ oral health status, offer immediate advice, and demonstrate techniques for oral hygiene or self-examination [21]. Store-and-forward entails capturing images, videos, or other dental data at one location and securely transmitting them to another location for evaluation by a dentist or specialist at a later time, making it useful for diagnostic purposes, treatment planning, and offering second opinions [21]. Remote monitoring utilizes wearable devices, sensors, or mobile applications to track patients’ oral health metrics over time, enabling dentists to monitor parameters such as tooth movement, bruxism activity, mouth opening, or adherence to oral hygiene practices remotely [20].
For OPMD and oral cancer, the most frequently used teledentistry modalities are store-and-forward and remote monitoring [11]. Previous studies have supported asynchronous teledentistry for OPMD diagnosis [22]. Additionally, mobile phones have been used in previous studies to aid in the remote early detection of oral cancer by primary care dental practitioners in resource-constrained settings [23]. In the Latin American region, Brazil, Chile, Colombia, Cuba, and Peru have reported studies in the teledentistry field, according to previous bibliometric analyses [24]. The teledentistry diagnostic process in Latin America starts with patients submitting images or videos of OPMDs/oral cancer followed by remote assessment by healthcare professionals. These professionals then formulate a diagnostic hypothesis, conduct consultations, and provide feedback, ultimately leading to a final diagnosis and treatment plan (Figure 1A). Brazil remains the first country in this region to describe the use of teledentistry for oral diagnosis through targeted research [11]. Tools used to obtain patient data include clinical photographs, smartphone-based examination photographs, video conferences, emails, questionnaires, histopathological examinations, and telemedicine applications and platforms [11, 25]. A previous systematic review reported that smartphones for image capturing are feasible and convenient for the implementation of teledentistry [25]. Nevertheless, challenges may arise worldwide when integrating teledentistry into oral diagnosis. While teledentistry modality facilitates proactive interventions and personalized care, it also presents regulatory considerations.
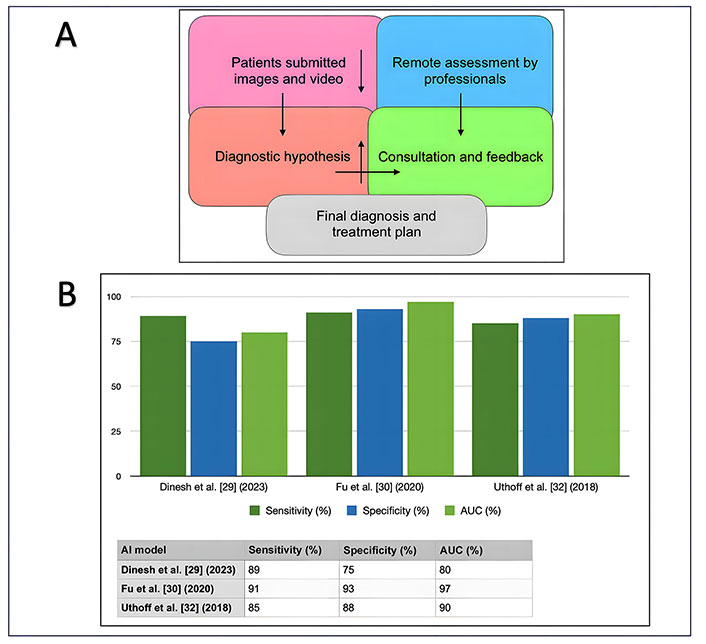
The process diagnosis and results of teledentistry use for oral potentially malignant disorders (OPMDs) and oral cancer in the Latin America. (A) Diagnosing process for (OPMDs) and oral cancer using teledentistry in Latin America; (B) performance metrics of machine learning and deep learning models in the context of the application of teledentistry and diagnosis of OPMD and oral cancer. AI: artificial intelligence; AUC: area under the curve
Regulatory considerations and challenges in teledentistry encompass various aspects [26]. Dentists engaging in telehealth practices must navigate licensing regulations tailored to the jurisdictions where their patients reside, potentially hindering licensure acquisition across multiple states or countries and thereby limiting the scope of teledentistry services. Compliance with health data privacy laws is imperative to safeguard patients’ confidential information during consultations and data transmission, necessitating the establishment of secure communication channels and encrypted storage systems. Furthermore, reimbursement poses a significant challenge for teledentistry, as insurance coverage and government healthcare programs may not fully encompass remote services, underscoring the need for advocacy efforts to promote policies recognizing the value and efficacy of telehealth care [26]. Moreover, the uneven distribution of technological infrastructure and access exacerbates the adoption of teledentistry, particularly in rural or economically disadvantaged areas, emphasizing the importance of investing in infrastructure and digital literacy initiatives to bridge these gaps [26].
Recent years have seen remarkable strides in teledentistry. This paradigm shift has been accelerated by innovations across the integration of artificial intelligence (AI) for image analysis, development of smartphone-based oral screening tools, and teleconsultation platforms tailored for disease diagnosis, especially OPMDs and oral cancer lesions. An annual increase of 42.1% is observed in the number of articles published on AI in telemedicine [27], and in this context, AI can assist patients, clinicians, researchers, and healthcare systems [28].
The integration of AI for image analysis and decision support has revolutionized the way dental professionals interpret radiographs and intraoral images. AI algorithms can swiftly analyse vast amounts of data, aiding in the detection of oral lesions [28]. Machine learning (ML) models are trained on extensive datasets to recognize patterns indicative of oral lesions, enabling quicker and more accurate diagnoses, with a strong performance (Figure 1B). A previous study, reporting specificity and sensitivity rates of 75% and 88% respectively, demonstrated that analysing 300 photographs of intraoral lesions could reveal the potential of ML for early detection of OPMD [29]. Remote screening with intraoral photographs has been useful in identifying OPMD and oral cancer [30]. Moreover, AI-powered decision support systems offer valuable insights to clinicians, facilitating treatment planning and enhancing patient care outcomes. The use of AI in teledentistry could improve patient diagnosis in Latin American countries, but new evidence is necessary to support this statement. Previous studies suggested that AI and telehealth services together could potentially improve patient outcomes for oral cancer patients, make it easier for oral medicine specialists to share clinical data, and improve case monitoring in Brazil’s public healthcare system [31].
The development of smartphone-based oral screening tools has democratized access to dental care, particularly in underserved regions with limited infrastructure [28]. These mobile applications utilize the built-in capabilities of smartphones, such as cameras and sensors, to perform oral examinations remotely. Users can capture images of their oral cavity and upload them to the app, where AI algorithms analyse the images for signs of OPMD or oral cancer. A previous study aimed to analyse the use of probes (autofluorescence and white light imaging) on a smartphone platform to detect OPMD and oral cancer lesions in high-risk populations in remote regions with limited infrastructure. This study incorporated convolutional neural networks (CNN) to classify the images into suspicious and not suspicious, and the results showed sensitivity and specificity ranges from 81% to 94% [32]. In this context, remote consultations will be possible with the installation of these probes in primary care centers serving high-risk populations. These probes can be used even in the event that a healthcare professional is absent. In order to lessen the burden of oral diseases, this would also make predictive population risk stratification possible [28].
Teleconsultation platforms tailored for OPMD diagnosis represent a significant advancement in teledentistry, addressing the critical need for early detection of OPMD. These platforms provide a secure environment for patients or primary healthcare professionals to communicate with oral medicine specialists, enabling remote consultations and evaluations of suspicious lesions. In Brazil, the Ministry of Health, in partnership with the Federal University of Rio Grande do Sul, created an online service to support diagnosis and decision-making for oral lesions. In five years of experience with this service, OPMDs were reported in 19% of cases, and 7.7% were suspected to be malignant lesions [33]. Advanced features, such as high-definition video conferencing and secure image sharing, facilitate comprehensive assessments and collaborative decision-making between clinicians and specialists. By leveraging teleconsultation platforms, patients can receive timely evaluations, avoid unnecessary referrals, and obtain treatment recommendations, ultimately improving outcomes for individuals at risk of oral cancer [33].
Integrating AI into telehealth services within the global healthcare system has the capacity to enhance patient outcomes in OPMD and oral cancer, streamline the sharing of clinical information among specialists in oral medicine, and bolster the monitoring of cases. Engaging healthcare professionals in the ultimate decision-making process, coupled with the imperative for further research and interdisciplinary teamwork, is essential for reducing misdiagnoses and promoting superior clinical results in the treatment of OPMD and oral cancer in the Latin American region.
Clinical outcomes and validation studies offer compelling evidence supporting the effectiveness, reliability, and acceptance of teledentistry, including its role in diagnosing OPMDs. Few investigations have delved into the efficacy of teledentistry in identifying OPMDs and oral cancer in the Latin American region, consistently presenting encouraging results. Typically, these studies involve remote consultations where patients submit images or videos of suspicious oral lesions for assessment by dental professionals.
A study from Brazil examined the feasibility of diagnosing oral diseases based on digital images communicated by email. The results suggested that distant diagnosis can be an effective alternative in diagnosing oral lesions and that using two distant consultants improves diagnostic accuracy [34]. In this context, the use of information technology can increase the accuracy of consultations in oral medicine [35].
Research consistently demonstrated high levels of sensitivity and specificity in diagnosing OPMDs via teledentistry, comparable to traditional in-person evaluations. For instance, a previous study from Brazil examined the diagnostic accuracy between presential assessments of oral lesions and the diagnostic hypotheses proposed at a distance with the use of a sample of photographs obtained with a smartphone, concluding good diagnostic accuracy [36]. Additionally, Fonseca et al. [37] (2022) demonstrated that telediagnosis using smartphone photography is reliable, producing results comparable to in-person diagnoses.
Roxo-Gonçalves et al. [38] (2017) evaluated the diagnostic skills of primary healthcare professionals regarding oral cancer and presented them with an e-learning course. The results suggested that both dentists and non-dentists have a fairly good capacity for discriminating the nature of oral lesions. Early OSCC is the most challenging situation and remains an issue to be addressed [38]. Carrard et al. [39] (2018) summarized the experience of a telediagnosis program catering to primary care dentists and physicians from southern Brazil. The results showed that AC and OSCC were the most common diagnoses, concluding that telediagnosis for oral lesions is feasible and has the potential to improve the quality of primary health care by bridging the gap between primary and specialized health care [39]. A meta-analysis performed by a Brazilian research group reported a high probability of detecting OPMD by remote examination (97.37%) but highlighted that new studies are required to incorporate them into clinical practice [40]. In addition, Brazilian researchers reported an increased awareness of oral cancer and increased availability of expert advice on teledentistry for the diagnosis and treatment of oral lesions. While this approach has promising potential, there are obstacles that need to be addressed [41].
In summary, although few published studies have reported on teledentistry in the context of OPMD and oral cancer diagnosis in the Latin American region, clinical outcomes and validation studies robustly support the efficacy, reliability, and patient acceptance of teledentistry. Comparative analyses with traditional evaluations demonstrate comparable diagnostic accuracy, while patient satisfaction surveys underscore the convenience and accessibility of teledentistry services. These findings emphasize teledentistry’s potential to enhance oral healthcare delivery, particularly in the early detection and management of potentially malignant oral lesions.
A comprehensive review of the current state and potential for the use of teledentistry in detecting OPMD and oral cancer reveals promising applications. However, most of the existing literature focuses on real-time and store-and-forward methods, as well as remote monitoring and mobile health technologies. Given this, it is crucial to approach the outcomes of AI applications with caution, especially when drawing conclusions about their effectiveness. While the studies highlighted the potential of AI, the small number of images used raises questions about the robustness and generalizability of the resulting AI models. The complexity and heterogeneity of OPMD suggest that larger and more diverse datasets are necessary to develop reliable AI-based screening programs. Collaborative efforts across multiple institutions could facilitate the collection of sufficient data, ultimately leading to the creation of AI models that are more accurate, sensitive, and generalizable. These models could then be effectively integrated into teledentistry platforms for the early detection and management of OPMD and OC, complementing existing telemedicine approaches.
In addition, capturing high-quality photographs of intraoral lesions poses significant challenges, even under optimal clinical conditions. These challenges are often due to the limited space, lighting difficulties, and the need for proper angulation. To improve the quality of intraoral images in the region under investigation, several strategies can be employed such as the use of specialized equipment, lighting adjustments, positioning and stabilization, and training and practice. By implementing these techniques, the quality of intraoral images can be significantly improved, making teledentistry applications for OPMD and oral cancer more effective in diagnosis and management.
Teledentistry, while holding promise in revolutionizing oral healthcare delivery, faces several challenges in effectively addressing the management of OPMDs and oral cancer. The foremost obstacle lies in its inability to offer complete consultations, hindering comprehensive assessment and diagnosis. This limitation is compounded by reduced confidence among both patients and health professionals due to the absence of physical interaction and examination [42, 43]. Moreover, the shift towards teledentistry necessitates a modification in the knowledge and skills required of health professionals, along with ergonomic challenges in adapting to virtual platforms [42, 43].
Patients in high-risk groups may have varying levels of motivation to engage with telehealth services. Factors influencing their motivation may include their familiarity with technology, perceived ease of use, and the perceived effectiveness of telemedicine in managing their condition. However, a significant barrier remains in the form of access to necessary tools, such as smartphones and reliable internet connections. While many patients in urban areas may possess these tools, those in rural or underserved regions might face challenges. As a result, the effectiveness of telemedicine in reaching these populations could be limited by technological disparities. Addressing these barriers is crucial to ensuring equitable access to telemedicine services for the early detection and management of OPMD and oral cancer.
Teledentistry faces a myriad of barriers, particularly within the realms of organization, bureaucracy, and regulatory frameworks [44]. Infrastructure planning and development present significant challenges, with disparities in technological access and uneven distribution of resources hindering widespread adoption, especially in Latin American countries [42–44]. Telecommunications regulations further complicate matters, often lacking clarity or adaptability to evolving telemedicine practices [42]. Compounding these issues is the absence of consistent reimbursement policies for telemedicine services, leaving practitioners financially unsupported. Licensure and credentialing pose additional hurdles, as conflicting interests among stakeholders contribute to a lack of uniform standards across states and countries [42–44].
Overcoming these challenges and barriers demands concerted efforts in technological advancements, regulatory frameworks, and educational initiatives to ensure the efficacy and reliability of teledentistry in managing OPMD and oral cancer.
Looking forward, the future of teledentistry concerning OPMD and oral cancer diagnosis is marked by ongoing innovation, collaboration, and commitment to improving patient outcomes and access to oral healthcare services [4]. By embracing emerging technologies, standardizing practices, fostering collaboration, and investing in education and training, the dental community can harness the full potential of teledentistry to address the evolving needs of patients and enhance the delivery of oral healthcare worldwide [4, 10]. Additionally, teledentistry could improve the screening of OPMD and oral cancer, as shown by a previous study [45]. Low-and-middle-income Asian countries have utilized teledentistry for the early detection of oral cancer with promising results [46, 47]. These results could be explored in the Latin American region, as developing countries could address oral cancer screening in conjunction with visual oral examinations to reduce incidence and mortality rates.
Teledentistry presents a transformative opportunity for addressing the challenges of diagnosing and managing OPMDs and oral cancer in the Latin American region. By harnessing the capabilities of cutting-edge technologies like AI, smartphone-based oral screening tools, and teleconsultation platforms, teledentistry offers a multifaceted approach to enhancing early detection, evaluation, and treatment of these conditions. Particularly in underserved communities where access to traditional dental services may be limited, teledentistry emerges as a vital tool for overcoming barriers to oral healthcare. Its ability to facilitate remote consultations, real-time assessments, and secure image sharing empowers both patients and oral healthcare providers to collaborate effectively in identifying and managing OPMDs. Moreover, the integration of AI algorithms for image analysis and decision support enhances diagnostic accuracy and efficiency, enabling timely interventions and ultimately improving patient outcomes. Thus, the potential of teledentistry in the Latin American region is immense, promising to revolutionize oral healthcare delivery and combat the burden of OPMDs and oral cancer.
AC: actinic cheilitis
AI: artificial intelligence
OE: oral erythroplakia
OL: oral leukoplakia
OPMDs: oral potentially malignant disorders
OSCC: oral squamous cell carcinoma
SCC: squamous cell carcinoma
CMP: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. SW and ARSS: Validation, Supervision, Writing—review & editing. All authors read and approved the submitted version.
Saman Warnakulasuriya who is the guest editor of Exploration of Digital Health Technologies had no involvement in the decision-making or the review process of this manuscript. The other authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Xin-Jia Cai
Eduardo D. Piemonte ... Jerónimo P. Lazos
Kehinde Kazeem Kanmodi ... Jacob Njideka Nwafor
Romina Andrian ... Gerardo Gilligan
Márcio Diniz-Freitas ... Pedro Diz-Dios
Gerardo Gilligan ... Eduardo Piemonte
Simon A. Fox, Camile S. Farah
Constanza B. Morales-Gómez ... Víctor Beltrán
Anna Luíza Damaceno Araújo ... Alan Roger Santos-Silva
