Abstract
Digital technologies have garnered more attention in this epoch of public health emergencies like coronavirus disease 2019 (COVID-19) and monkeypox (mpox). Digital twin (DT) is the virtual cybernetic equivalent of a physical object (e.g., a device, a human, a community) used to better understand the complexity of the latter and predict, prevent, monitor, and optimize real-world outcomes. The possible use cases of DT systems in public health ranging from mass vaccination planning to understanding disease transmission patterns have been discussed. Despite potential applications in healthcare, several economic, social, and ethical challenges might hinder the universal implementation of DT. Nevertheless, devising appropriate policies, reinforcing good governance, and launching multinational collaborative efforts ascertain early espousal of DT technology.
Keywords
Digital public health, digital twins, public health emergencies, healthcare, digital technologies, epidemiology, remote health, smart health cityDigital public health (DPH) is an emerging field that leverages digital technologies like digital twin (DT) to improve population health in the context of health promotion and disease prevention [1]. Although the first formal definition of DT was first provided by the National Aeronautics and Space Administration (NASA), the term DT was first used by Grieves [2] in his white paper on manufacturing excellence. Even earlier, the term was mentioned in 1994 in a paper describing the design of three-dimensional (3D) phantoms of coronary arteries [3]. A few of the key motivations for why DPH is important are:
(1) Improved disease surveillance and outbreak monitoring: by collecting, analyzing, and sharing real-time data with public health agencies to rapidly detect and respond to outbreaks, monitor patterns of disease spread, and identify high-risk populations [4].
(2) Enhanced health promotion and education: digital technologies provide innovative channels for health promotion and education. DPH leverages digital platforms such as mobile applications and social media to disseminate accurate health information, raise awareness about preventive measures, and promote healthy behaviors [5].
(3) Personalized and remote healthcare: DPH enables personalized healthcare delivery and remote monitoring of patients. Telemedicine and virtual consultations allow healthcare providers to remotely diagnose, treat, and monitor patients, reducing the burden on traditional healthcare systems and improving access to care, particularly in underserved areas [6].
DT is the virtual cybernetic equivalent of a physical object used to better understand the complexity of the latter and predict, prevent, monitor, and optimize the real-world outcome. DT is one of the potential technologies used for diverse industrial applications (e.g., industry 4.0 powered manufacturing, gauging marine fouling, in-orbit wargaming in aerospace, personalized diagnosis, and precision medicine). The DT comprises three basic components as defined by Grieves [2] (Figure 1):
(1) The physical entity can be a product, a process, a human, a feature, or a setting in real space. e.g., a patient, a smartphone, a wearable, a medical device, an external stimulus such as temperature, humidity, altitude, social, economic, political issues influencing patient health, or a multi-specialty hospital.
(2) The virtual entity replicates the physical characteristics in virtual space. e.g., a patient model, a smartphone model, a medical device model, an external stimulus, a digital system model, a community model, etc.
(3) The digital thread is the patient/population health data that facilitates closed-loop optimization of the siloed and unsynchronized systems and enables two-way interaction between real and virtual components. e.g., electronic medical/health record (EMR/EHR), clinical trial registries, survey reports, epidemiological surveillance data, digital diagnostics and genomics sequencing data, population information from government databases, etc.
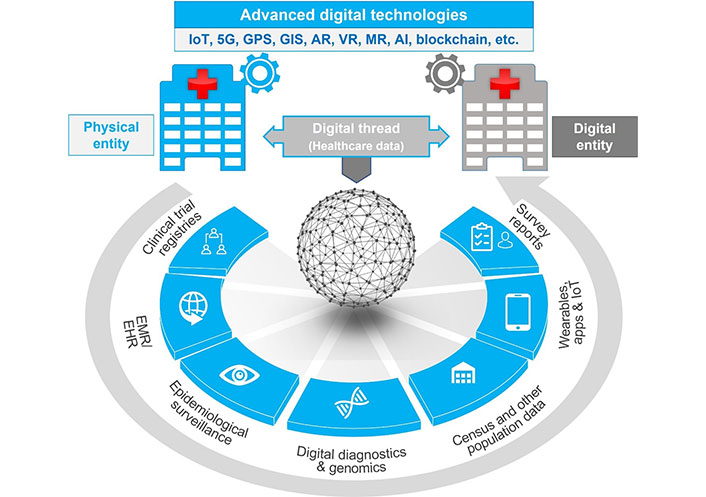
The ecosystem of DT technology. DT consists of a physical entity and its replica (virtual/digital entity). Both components are tied together with the digital thread (the healthcare data). Various advanced technologies like Internet-of-Things (IoT), artificial intelligence (AI), fifth generation (5G), global positioning system (GPS), mixed reality (MR), cloud storage, etc. are used in the data collection and processing, as well as storage, and two-way communication between physical and DTs. GIS: geographic information systems; AR: augmented reality; VR: virtual reality
Advanced technologies such as IoT, cloud computing, GPS, GIS, big data analytic engines, AI, complex simulation systems, 5G communication systems, blockchain, AR, VR, and MR enable the data collection, curation, analysis, and visualization. This curated data (obtained from physical and DTs) could be used for the optimization of patient/population health [7, 8].
DT technology in DPH has the potential to revolutionize healthcare by improving planning and design, enabling real-time monitoring and analysis, facilitating predictive analytics, personalizing healthcare, enhancing training and education, and fostering collaboration. It can drive better health outcomes, optimize resource allocation, and contribute to the overall well-being of individuals and communities in the following ways [9–13]:
(1) Improved and faster mass immunization planning: it could be used to plan resource-optimized mass vaccination campaigns by designing walk-in vaccination clinics with the best configuration in terms of vaccination rate, ideal number of operators, shift duration, mean process time, etc.
(2) Remote and personalized health management: with the help of DT-enabled robotic navigation and IoT connectivity, healthcare professionals can safely monitor infected patients in real time through patient-mounted sensors.
(3) Smart health cities: coupling the DT technology with GIS proffers an array of urban and public health applications including road traffic and air pollution mitigation, sewage disposal, flood monitoring, mobility optimization, etc.
(4) Medical facility and operations design: DT systems could be used to effectively utilize the medical facility through appropriate resource capacity planning and enhance patient’s journey through workflow optimization, bed occupancy prediction, etc.
(5) Clinical research: data obtained through DT simulation models enable near real-world assessment of the effects of interventions such as drugs, supplements, and medical devices on larger groups (healthy population and patient groups).
(6) Drug and vaccine development: from the selection of the best antigens and vectors for vaccines to optimized adjuvants or other formulation ingredients and molecular targets of drugs, DT technology could be potentially used to develop safe and effective biopharmaceuticals.
(7) Health equity planning: Cleveland Clinic (CC) and MetroHealth received a grant of $3.14 million from the National Institutes of Health (NIH) to harness the potential of DT technology to foster a better understanding and tackle the health disparities among disadvantaged communities.
(8) Treatment optimization: Dell Technologies [in association with Integrating Biology and the Bedside (i2b2) tranSMART] has developed an AI-driven DT-based research technology for coronavirus disease 2019 (COVID-19) Long-Hauler Project to understand the causes of long COVID and develop effective treatments.
While DT systems offer the potential to revolutionize public health implementation, it is still in its infancy and hence the full-fledged implementation of the DT systems has several limitations and challenges. Streamlining and standardizing the siloed data from multiple sources is a major challenge. Feasibility with other digital devices/software, complex infrastructure, high implementation and maintenance cost, data quality control, and availability of technical multi-level experts are the additional issues. Some of the key limitations and challenges associated with implementing DT systems in DPH are:
(1) Data privacy and security: implementing DT systems in DPH relies on extensive personal health data, emphasizing the need for privacy and security. However, challenges arise, requiring measures to protect data, comply with regulations, and maintain public trust.
(2) Data interoperability and standardization: as public health data is sourced from diverse platforms like EHRs, wearables, and connected devices, leading to data format and standard disparities, harmonizing and standardizing data across systems is crucial to enhance DT system utility by overcoming integration and interoperability challenges. Hence, appropriate quality control systems must be in place to handle the big data fed into multi-level components of the DT ecosystem. Besides, the scalability of the data from a process or asset level to the enterprise level and the composability of DT data for different applications are additional challenges.
(3) Ethical considerations: implementing DT systems in public health brings ethical concerns, including transparency and informed consent when utilizing personal health data. Careful design and training of DT models are essential to avoid algorithmic bias and discrimination. Ensuring fairness, accountability, and transparency is vital to mitigate unintended negative impacts.
(4) Skill and knowledge gaps: implementing DT systems in DPH requires skilled professionals in data analytics, machine learning, and public health. However, there is often a shortage of such expertise, making training and capacity-building essential for successful implementation.
DT technology is one of the rapidly growing digital technologies in healthcare, especially in the pandemic era. The possible use cases of DT systems in public health ranging from mass vaccination planning to understanding disease transmission patterns have been discussed. Despite umpteen application areas in the healthcare milieu, the cost-associated with DT efforts might further worsen the existing social disparities across the globe. It is worth mentioning that as with any breakthrough technology, DT systems also require time to fix the cost-associated impediments. Since, it is a progressive process wherein research and development of low-cost components and proliferation of more competitors occurs, affordability would definitely improve. Hence, potential long-term benefits to public health should not be overlooked considering the cost burden in the developmental epoch.
Considering the growing aging population, recurrence of pandemics/syndemics (e.g., COVID-19, mpox, etc.), healthcare staff shortage, and increasing patient expectations, future research and development must be focused on personalized healthcare, rapid diagnosis, affordable and enhanced care (especially for a specific population like patients with multiple comorbidities and disability, patients requiring palliative care, etc.), ethical and secure data sharing, etc. Potential strategies including process/asset-wise and comprehensive data privacy validation, establishing good governance, and implementation of coordinated multinational efforts can be followed to improve decision-making, better support public health initiatives, and facilitate more personalized and effective interventions for population health management.
Abbreviations
| 5G: | fifth generation |
| AI: | artificial intelligence |
| COVID-19: | coronavirus disease 2019 |
| DPH: | digital public health |
| DT: | digital twin |
| EHR: | electronic health record |
| GIS: | geographic information systems |
| GPS: | global positioning system |
| IoT: | Internet-of-Things |
| MR: | mixed reality |
Declarations
Author contributions
SK, DKK, and EUS: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. AM: Conceptualization, Validation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2023.