Abstract
A 74-year-old male patient with beta thalassemia minor presented in 2022 for a follow-up of osteoporosis diagnosed prior to 2004. At the time of presentation, his medical history included: radiation exposure to his head and neck, goiter, prostate cancer status post resection in 2019 without a history of anti-androgen therapy, and atrial fibrillation, for which he had been prescribed apixaban since 2021. Treatment with risedronate occurred from approximately 2004 to about 2011, with improvement in bone density to osteopenia. He had also taken vitamin D and calcium supplementation and engaged in regular weight-bearing exercise. The patient had no other known risk factors for decreased bone mineral density preceding the onset of his osteoporosis, and a previous workup for secondary causes of his osteoporosis etiology proved negative. We propose that beta thalassemia minor is potentially a risk factor for osteopenia and osteoporosis, and that bisphosphonates can be considered for management when therapeutic intervention is indicated. Even in the absence of other known risk factors, clinicians should consider periodically screening beta thalassemia minor patients with DXA for evaluation of bone health.
Keywords
Osteoporosis, osteopenia, beta thalassemia, bone mineral densityIntroduction
Osteoporosis is a known complication of beta thalassemia major and beta thalassemia intermedia, though its etiology in the context of these conditions is not well understood [1, 2]. The pathogenesis of osteoporosis is thought to be distinct in thalassemia major and intermedia [3], and multifactorial. Potential etiologies include bone marrow expansion, ineffective erythropoiesis, abnormal osteoclast activity, GH/IGF-1 axis dysfunction, hypogonadism, vitamin D deficiency, parathyroid dysfunction, receptor gene polymorphisms, and iron overload secondary to treatment [4–7]. To date, however, there is no known association between osteoporosis and beta thalassemia minor [8]. We present a case of a patient with known beta thalassemia minor who presented for osteoporosis follow-up, with no other known risk factors for osteoporosis at the time of diagnosis or at the time of presentation [9]. We postulate that beta thalassemia minor, a form of non-transfusion-dependent thalassemia, may be an independent risk factor for osteoporosis [9], adding to one existing case report in the literature suggesting a potential link between the two conditions [3].
Case report
A 74-year-old Caucasian male patient with beta thalassemia minor presented for osteoporosis follow-up in 2022. The patient reported that his osteoporosis was diagnosed prior to 2004, i.e., prior to when he was 56 years old. At the time of presentation, his medical history was notable for radiation exposure to his head and neck as part of a clinical trial for the treatment of adenoiditis at age 9 or 10, in addition to goiter, prostate cancer status post resection in 2019, and atrial fibrillation, for which he had been prescribed apixaban since 2021. The patient’s mother had a history of thalassemia, and as the patient was diagnosed with thalassemia minor around the age of 12 to 15 years, we do not have access to his HbA2 testing results. While he follows a with Hematology/Oncology for his anemia and prostate cancer, he has never required a transfusion. Free testosterone, parathyroid hormone, calcium, and serum protein electrophoresis levels evaluated prior to his osteoporosis diagnosis were normal. There is no record or report of the patient receiving anti-androgen therapy following his prostate cancer diagnosis. He had no history of fractures as an adult. He was treated with risedronate for his osteoporosis from approximately 2004 to 2011, with improvement in bone density to osteopenia as measured in the lumbar spine (T-score of –2.8 to –2.1 within that time frame) (Figure 1) and total left hip (T-score of –2.2 to –1.4) (Figure 2), and with no significant adverse effects. Although not measured prior to 2005, bone mineral density in the left femoral neck improved from osteopenia in 2005 (T-score of –1.7) to a normal value (T-score of –0.8) in 2011 (Figure 3), also during the course of risedronate treatment.
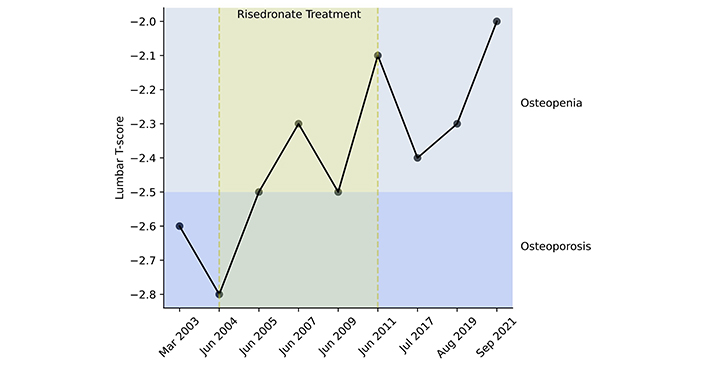
Over the course of the patient’s risedronate treatment (2004–2011), lumbar spine T-scores showed improvement from osteoporosis to osteopenia. Bone mineral density remained stable in the osteopenic range in the 10 years following risedronate treatment (2011–2021), during which the patient engaged in conservative management alone. T-scores of –1 or higher are classified as normal, –1 to –2.5 are classified as osteopenia, and –2.5 or below are classified as osteoporosis. Years on the horizontal axis are not continuous or represented to scale. They represent the dates on which the patient received DXA screening and corresponding records are available
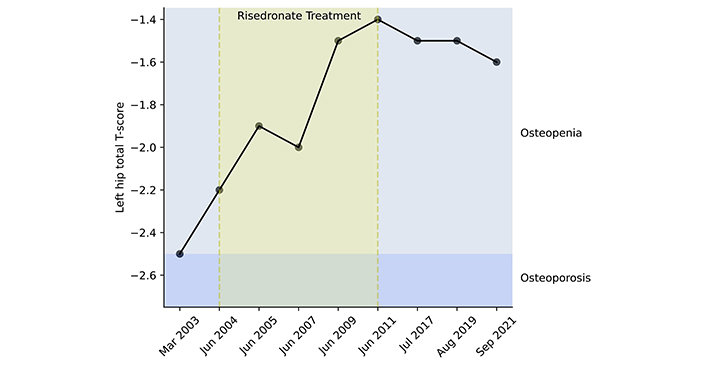
Over the course of the patient’s risedronate treatment (2004–2011), left hip total T-scores showed improvement within the osteopenic range. Bone mineral density remained stable in the osteopenic range in the 10 years following risedronate treatment (2011–2021), during which the patient engaged in conservative management alone. T-scores of –1 or higher are classified as normal, –1 to –2.5 are classified as osteopenia, and –2.5 or below are classified as osteoporosis. Years on the horizontal axis are not continuous or represented to scale. They represent the dates on which the patient received DXA screening and corresponding records are available
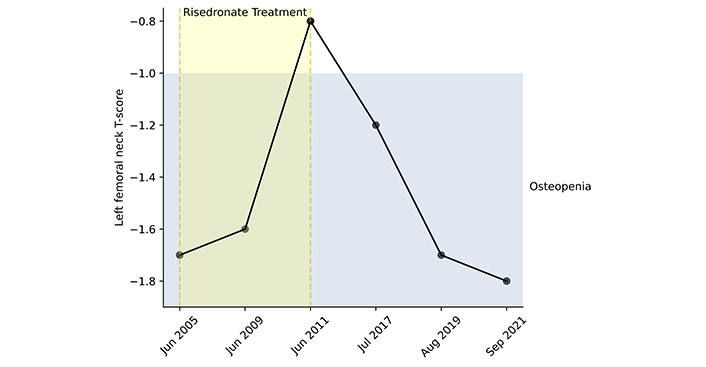
Over the course of risedronate treatment (2004–2011; values only available from 2005 onward), left femoral neck T-scores showed improvement from the osteopenic range to the normal range. T-scores decreased in the 10 years following risedronate treatment (2011–2021), during which the patient engaged in conservative management alone, but remained in the osteopenic range. T-scores of –1 or higher are classified as normal, –1 to –2.5 are classified as osteopenia, and –2.5 or below are classified as osteoporosis. Years on the horizontal axis are not continuous or represented to scale. They represent the dates on which the patient received DXA screening and corresponding records are available
Following his risedronate treatment regimen prior to presentation, the patient underwent conservative monitoring, with a target daily calcium intake (via diet and supplements) of 1,000–1,200 mg and a daily vitamin D3 intake of 2,000 IU. By 2020, his 25-hydroxyvitamin D levels were within the normal range, measuring 39.7 ng/mL, with most recent values of vitamin D levels within normal limits, 36.3 ng/mL in 2022 and 38.9 ng/mL in 2023. Most recently, thyroid levels were within normal range with a TSH in 2019 of 2.53 µIU/mL, and liver and renal function within normal limits as well. He also reported engaging in frequent weight-bearing exercise; specifically, walking and lifting weights multiple times weekly. As of September 2021, his bone mineral density was osteopenic in the lumbar spine (T-score of –2.0) and left hip (T-score of –1.6 in the left hip, and –1.8 in the femoral neck). The patient had no other known risk factors for decreased bone mineral density preceding the onset of his osteoporosis, and a previous workup for secondary causes of his osteoporosis etiology proved negative. The patient has had no fractures subsequent to his original diagnosis of osteoporosis.
Discussion
The absence of other apparent risk factors in our patient, coupled with the established association between osteoporosis and both beta thalassemia major and intermedia, we propose that beta thalassemia minor may be an independent risk factor for low bone mineral density and osteoporosis. While the Thalassemia International Federation advises annual DXA screening and assessment of bone turnover markers for the more severe transfusion-dependent thalassemia patients starting at age 10 [7], there are currently no specific guidelines for osteoporosis screening in non-transfusion-dependent thalassemias, such as beta thalassemia minor, β-thalassemia intermedia, hemoglobin E/β-thalassemia (mild and moderate), and α-thalassemia intermedia [10]. Bisphosphonates have proven to be an effective treatment for osteoporosis in thalassemia patients [4, 7]; however, their long-term safety and efficacy beyond 3–5 years of use remain uncertain [4].
In the case of our patient with beta thalassemia minor, the administration of risedronate for approximately 6–7 years resulted in significant improvements in bone mineral density, transitioning from the osteoporotic to the osteopenic range at the lumbar spine and left total hip. Notably, improvements in bone mineral density T-scores were evident within the first year of treatment initiation. Moreover, left femoral neck T-scores improved from the osteopenic to the normal range throughout the course of treatment.
Following the completion of risedronate therapy, our patient maintained bone mineral density within the osteopenic range at all measured sites from 2011 to at least 2021 by adopting lifestyle modifications similar to those recommended for postmenopausal osteoporosis, including calcium and vitamin D supplementation and regular weight-bearing exercise. Interestingly, despite sun exposure and taking 1,000 IU of vitamin D3, patients with beta thalassemia major can be prone to vitamin D deficiency. While our patient was diagnosed with thalassemia minor, not major, the known association of vitamin D deficiency in a related condition highlights the importance of monitoring vitamin D levels in such patients to ensure the adequacy of supplementation dose [1]. By adhering to these conservative measures, our patient with beta thalassemia minor successfully maintained bone mineral density in the osteopenic range and avoided fractures for at least a decade post-treatment.
Adding to one existing case report in the literature [3], we postulate beta thalassemia minor as a possible independent risk factor for osteoporosis. Clinicians should consider using periodic DXA scans to screen for osteopenia and osteoporosis in this patient population. Similar to postmenopausal or transfusion-dependent thalassemic patients with osteoporosis, bisphosphonate therapy remains an option to improve and maintain bone mineral density in patients with beta thalassemia minor demonstrating osteopenia or osteoporosis. Calcium and vitamin D supplementation, as well as weight-bearing exercise, also remain low-risk management options with likely benefit to bone health in this population.
Declarations
Author contributions
FW: Investigation, Writing—original draft, Writing—review & editing. TA and CH: Writing—review & editing. PM: Conceptualization, Validation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This case report does not require IRB Approval from the University of Connecticut Health Center IRB per their website policy (https://ovpr.uchc.edu/services/rics/hspp/resources/hspp-faqs/) and direct communication with the IRB staff at the health center.
Consent to participate
Informed consent to participate in the study was obtained from the participant.
Consent to publication
Not applicable.
Availability of data and materials
The datasets for this manuscript are not publicly available because they are patient information contained within this patient’s chart. Requests for accessing the datasets should be directed to Parvathy Madhavan (madhavan@uchc.edu).
Funding
Not applicable.
Copyright
© The Author(s) 2024.