The role of interleukin-24 in atopic dermatitis
Atopic dermatitis (AD) is characterized by skin barrier disruption, type 2 immune dysregulation, chronic pruritus, and abnormal colonization by
Staphylococcus aureus (
S. aureus). Tapinarof, an aryl
[...] Read more.
Atopic dermatitis (AD) is characterized by skin barrier disruption, type 2 immune dysregulation, chronic pruritus, and abnormal colonization by Staphylococcus aureus (S. aureus). Tapinarof, an aryl hydrocarbon receptor modulator, has been demonstrated to attenuate the development of AD in clinical studies. Recently, we found that tapinarof upregulated the expression of filaggrin and loricrin, which are essential proteins in skin barrier functions. Paradoxically, tapinarof induced interleukin (IL)-24 secretion by normal human keratinocytes. IL-24 is produced by T helper 2 lymphocytes and keratinocytes following stimulation by type 2 cytokines, and IL-24 is upregulated in the skin of patients with AD. Furthermore, IL-24 contributes to skin barrier disruption and hyperplasia in AD, and it may exacerbate skin inflammatory responses, itch, and S. aureus infection. In this review, we summarized the current findings regarding the detrimental role of IL-24 in AD, thereby suggesting that co-treatment of tapinarof with therapeutics that block IL-24 signaling may represent a promising strategy for managing AD.
Yen Hai Vu ... Gaku Tsuji
View:6775
Download:234
Times Cited: 0
Atopic dermatitis (AD) is characterized by skin barrier disruption, type 2 immune dysregulation, chronic pruritus, and abnormal colonization by Staphylococcus aureus (S. aureus). Tapinarof, an aryl hydrocarbon receptor modulator, has been demonstrated to attenuate the development of AD in clinical studies. Recently, we found that tapinarof upregulated the expression of filaggrin and loricrin, which are essential proteins in skin barrier functions. Paradoxically, tapinarof induced interleukin (IL)-24 secretion by normal human keratinocytes. IL-24 is produced by T helper 2 lymphocytes and keratinocytes following stimulation by type 2 cytokines, and IL-24 is upregulated in the skin of patients with AD. Furthermore, IL-24 contributes to skin barrier disruption and hyperplasia in AD, and it may exacerbate skin inflammatory responses, itch, and S. aureus infection. In this review, we summarized the current findings regarding the detrimental role of IL-24 in AD, thereby suggesting that co-treatment of tapinarof with therapeutics that block IL-24 signaling may represent a promising strategy for managing AD.
 Immunology of biodegradable nanoparticles: a brief overview on a wide growing fieldOpen AccessReviewImmunity is continuously evolving by evolutionary mechanisms shaped by pathogenic stimuli of different kinds. Man-made nanomaterials (NMs) have been developed in the last decades and represent a nov [...] Read more.Anissa Pisani, Giuseppe BardiPublished: April 30, 2021 Explor Immunol. 2021;1:48–60
Immunology of biodegradable nanoparticles: a brief overview on a wide growing fieldOpen AccessReviewImmunity is continuously evolving by evolutionary mechanisms shaped by pathogenic stimuli of different kinds. Man-made nanomaterials (NMs) have been developed in the last decades and represent a nov [...] Read more.Anissa Pisani, Giuseppe BardiPublished: April 30, 2021 Explor Immunol. 2021;1:48–60 Interleukin-22 and keratinocytes; pathogenic implications in skin inflammationOpen AccessReviewInterleukin (IL)-22 is produced from immune cells such as T helper (Th)22 cells, Th17/22 cells, and group 3 innate lymphoid cells. IL-22 signals via the IL-22 receptor 1 (IL-22R1) and the IL-10 rece [...] Read more.Masutaka Furue, Mihoko FuruePublished: April 30, 2021 Explor Immunol. 2021;1:37–47
Interleukin-22 and keratinocytes; pathogenic implications in skin inflammationOpen AccessReviewInterleukin (IL)-22 is produced from immune cells such as T helper (Th)22 cells, Th17/22 cells, and group 3 innate lymphoid cells. IL-22 signals via the IL-22 receptor 1 (IL-22R1) and the IL-10 rece [...] Read more.Masutaka Furue, Mihoko FuruePublished: April 30, 2021 Explor Immunol. 2021;1:37–47 Correlation of N-glycan dynamics and interaction network with allosteric antigen binding and Fc receptor recognitionOpen AccessOriginal ArticleAim: Fragment crystallizable (Fc) glycans modulate Fc conformations and functions, and glycan may also regulate antigen recognition. In the antibody drug development, glycosylation patterns affect a [...] Read more.Buyong MaPublished: April 30, 2021 Explor Immunol. 2021;1:27–36
Correlation of N-glycan dynamics and interaction network with allosteric antigen binding and Fc receptor recognitionOpen AccessOriginal ArticleAim: Fragment crystallizable (Fc) glycans modulate Fc conformations and functions, and glycan may also regulate antigen recognition. In the antibody drug development, glycosylation patterns affect a [...] Read more.Buyong MaPublished: April 30, 2021 Explor Immunol. 2021;1:27–36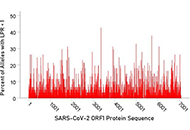 In silico investigation of binding affinities between human leukocyte antigen class I molecules and SARS-CoV-2 virus spike and ORF1ab proteinsOpen AccessOriginal ArticleAim: The novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019, a global pandemic. There is hence an urgent need for effective approaches to [...] Read more.Spyros A. Charonis ... Apostolos P. GeorgopoulosPublished: April 30, 2021 Explor Immunol. 2021;1:16–26
In silico investigation of binding affinities between human leukocyte antigen class I molecules and SARS-CoV-2 virus spike and ORF1ab proteinsOpen AccessOriginal ArticleAim: The novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019, a global pandemic. There is hence an urgent need for effective approaches to [...] Read more.Spyros A. Charonis ... Apostolos P. GeorgopoulosPublished: April 30, 2021 Explor Immunol. 2021;1:16–26 The role of interleukin-24 in atopic dermatitisOpen AccessReviewAtopic dermatitis (AD) is characterized by skin barrier disruption, type 2 immune dysregulation, chronic pruritus, and abnormal colonization by Staphylococcus aureus (S. aureus). Tapinarof, an aryl [...] Read more.Yen Hai Vu ... Gaku TsujiPublished: April 30, 2021 Explor Immunol. 2021;1:4–15
The role of interleukin-24 in atopic dermatitisOpen AccessReviewAtopic dermatitis (AD) is characterized by skin barrier disruption, type 2 immune dysregulation, chronic pruritus, and abnormal colonization by Staphylococcus aureus (S. aureus). Tapinarof, an aryl [...] Read more.Yen Hai Vu ... Gaku TsujiPublished: April 30, 2021 Explor Immunol. 2021;1:4–15 Exploration of Immunology: challenging knowledge, developing curiosity and transforming passion into discoveryOpen AccessEditorialDominique J Charron, Reem Al-DaccakPublished: April 30, 2021 Explor Immunol. 2021;1:1–3
Exploration of Immunology: challenging knowledge, developing curiosity and transforming passion into discoveryOpen AccessEditorialDominique J Charron, Reem Al-DaccakPublished: April 30, 2021 Explor Immunol. 2021;1:1–3