Affiliation:
1Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, 3584 CG Utrecht, The Netherlands
2Centre for Human Psychopharmacology, Swinburne University, Melbourne VIC 3122, Australia
Email: j.c.verster@uu.nl
ORCID: https://orcid.org/0000-0002-6455-2096
Affiliation:
1Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, 3584 CG Utrecht, The Netherlands
ORCID: https://orcid.org/0009-0000-5263-2833
Affiliation:
1Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, 3584 CG Utrecht, The Netherlands
3Global Centre of Excellence Immunology, Nutricia Danone Research, 3584 CT Utrecht, The Netherlands
ORCID: https://orcid.org/0000-0002-8678-9182
Explor Immunol. 2023;3:500–505 DOI: https://doi.org/10.37349/ei.2023.00116
Received: June 14, 2023 Accepted: October 19, 2023 Published: October 27, 2023
Academic Editor: Dominique J. Charron, Hospital Saint Louis, France
Immune fitness refers to the capacity of the body to respond to health challenges (such as infections) by activating an appropriate immune response, essential to maintain health, prevent and resolve disease, and improve quality of life [1]. Analogue to mental resilience, immune fitness is the ability to bounce back from physical events such as disease states and health complaints. Adequate immune fitness is thus crucial in determining longevity and plays an essential role from early life to healthy aging. In fact, reduced immune fitness may be the most important reason why patients visit their physician. As such, reduced immune fitness is an important health sign, and adequate assessment is therefore vital.
An example of the impact of immune fitness on health is evident from the coronavirus disease 2019 (COVID-19) pandemic. It was demonstrated that immune fitness was the best predictor of both the number and severity of symptoms of COVID-19 [2]. In this study, the immune fitness of 87 subjects who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was assessed. Regression analysis, considering many demographic variables (e.g., sex and age) and health correlates (e.g., body mass index and the presence of underlying diseases), revealed that immune fitness in 2019 (i.e., before the pandemic) was the single predictor of the number (27.2%) and severity (33.1%) of COVID-19 symptoms during the pandemic. The significant correlation between immune fitness in 2019 and the severity of COVID-19 symptoms once infected with SARS-CoV-2 during the COVID-19 pandemic is shown in Figure 1. The data suggest that, in terms of pandemic preparedness, maintaining adequate immune fitness is essential.
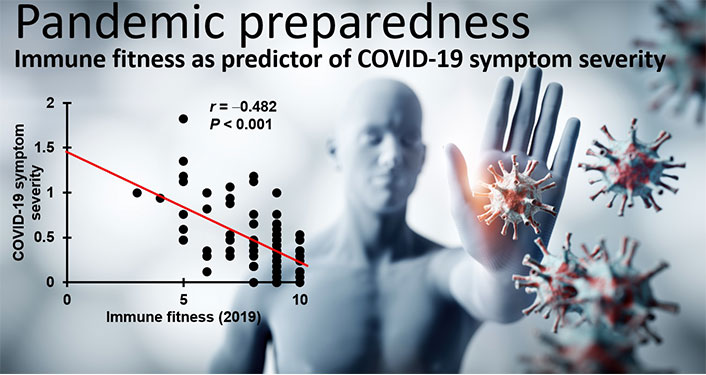
Relationship between immune fitness and the severity of COVID-19 symptoms [2, 3]. Immune fitness was assessed for 2019 with the immune status questionnaire (ISQ). COVID-19 symptom severity was assessed in 2020–2021 in n = 87 subjects with confirmed infection with SARS-CoV-2
Note. Adapted from “Emotion regulation and mood during the COVID-19 pandemic,” by Verster JC, Hendriksen PA, Kiani P, Merlo A, Balikji J, Garssen J, et al. J Clin Med. 2023;12:2758 (https://www.mdpi.com/2077-0383/12/8/2758/html). CC BY.
Traditionally, studies investigate the presence of possible systemic inflammation by assessing biomarkers in blood, saliva, or stool. Examples of these proxy measures of immune fitness are cytokines [e.g., interleukin 6 (IL-6)] and C-reactive protein. The obtained measures are then compared to normal ranges, and for example, used by physicians for diagnostic purposes. However, individuals are often unaware of bodily physiological changes that are considered a health risk. For example, unless they measure their blood pressure, individuals are usually not aware of having hypertension. In contrast to the forthcoming immune-related complaints, it is unclear to what extent individuals are aware of changes in biomarkers of systemic inflammation (e.g., an increase in certain cytokine concentrations). Also, changes in biomarkers may not be present in healthy subjects that report reduced immune fitness [1]. For example, if on a scale ranging from 0 (very poor) to 10 (excellent), an individual reports a decline of immune fitness from a score of 8 at baseline to a score of 6, this clearly indicates a state of reduced immune fitness, which may however not be reflected by changes in biomarkers, as the immune fitness scores remain in the “healthy” range (a score ≥ 6). Thus, biomarkers may be of particular interest in subjects that have underlying diseases characterized by chronic systemic inflammation.
In contrast to changes in biomarkers, people are usually well aware of experiencing reduced immune fitness. When assessing immune fitness, various determinants should be taken into account. These are summarized in Figure 2. Individuals weigh the characteristics and impact of immune-related complaints they experience when judging the status of their immune fitness. Considered factors include the type of complaint (e.g., coughing or fever), the number of experienced complaints, their frequency of occurrence, severity, and duration of these complaints, and to what extent they impact daily activities and interactions with others [2]. Having immune-related complaints may result in (chronic) systemic inflammation, and vice versa [4].
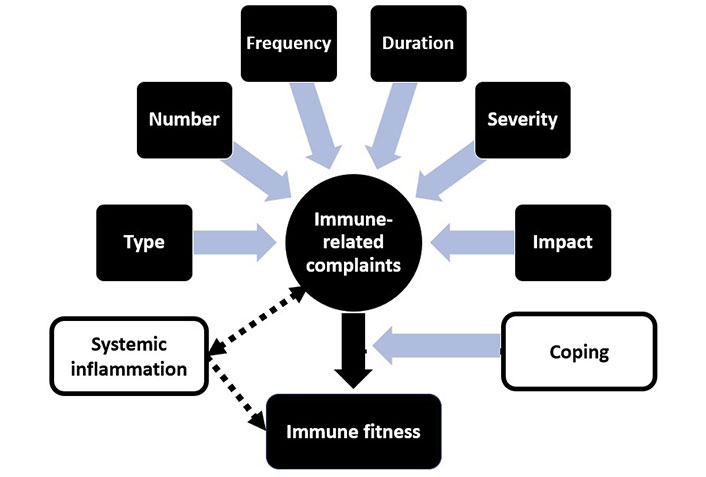
Determinants of immune fitness. The type, number, frequency of occurrence, duration, severity, and impact on daily life have an impact on how immune-related complaints are experienced (indicated by blue arrows). The extent to which immune-related complaints are experienced determines immune fitness (black arrow). The latter is influenced by how well subjects can cope with the experienced immune-related complaints (indicated by the black uninterrupted arrow). Immune-related complaints may result in systemic inflammation, and vice versa (indicated by the broken bi-directional black arrow). Systemic inflammation may have an impact on immune fitness, but can also go unnoticed (indicated by the broken black arrow)
To assess immune fitness directly, in 1999, Petrie et al. [5] used a 10 cm visual analog scale (the “immune system perception scale”) where subjects had to place a mark on the line what they thought was the state of their immune system. However, subsequent research did not adopt this scale. Over the past 8 years, significant progress has been made with regard to the methodology of assessment of immune fitness. Several patient-reported outcome measures were developed to assess the perception of an individual of his/her immune fitness [1]. In 2015, Donners et al. [6] conducted a survey among 574 Dutch young adults and used a yes/no question to assess reduced immune fitness. The sample with reduced immune fitness (36.4%) reported significantly more sleep disturbances (significantly higher scores on sleep apnea, insomnia, and circadian rhythm disorder), poorer sleep quality, and greater impairment of daytime functioning. In the same year, the multiple-item immune function questionnaire (IFQ) was introduced [7]. The IFQ has only been used in one study thereafter [8]. In this study, an 11-point single-item scale, ranging from 0 (very poor) to 10 (excellent), was used to assess immune fitness. The IFQ showed a modest correlation with the single-item immune fitness rating. The 23 IFQ items, complemented with some other items, were evaluated in a series of studies by Wilod Versprille et al. [9] to develop the 7-item ISQ. The ISQ retrospectively assesses the frequency of occurrence of 7 common immune-related complaints.
It can be assumed that single-item assessments automatically encompass all determinants of immune fitness (Figure 2) [1]. In contrast, the multiple-item scales such as the IFQ and ISQ consider only the number and frequency of immune-related complaints. Biomarker assessments can objectively demonstrate possible systemic inflammation but do not adequately represent the overall concept of immune fitness [1]. As a result, correlations between single-item assessments of immune fitness and biomarker assessments of systemic inflammation are usually poor-to-modest at best [10]. The latter is in line with the observed modest correlations between self-reported general health and biomarkers outcomes [11]. In contrast, there is a clear relationship between the burden of disease and the overall concept of immune fitness. This is illustrated in Figure 3, showing that immune fitness significantly decreases when individuals report one or more underlying diseases.
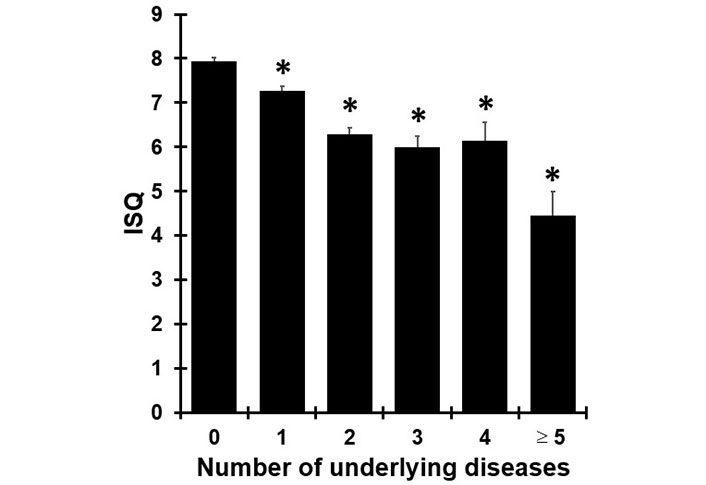
Immune fitness in individuals with and without underlying disease [12]. Subjects reported whether they suffered from one or more underlying diseases, including cardiovascular disease or hypertension, diabetes, liver disease, neurological diseases, immune disorders, allergy, kidney disease, pulmonary diseases, anxiety, depression, sleep disorders, and “other”. The relationship between the number of reported underlying diseases and immune fitness in 2019, assessed with the ISQ among n = 1,400 Dutch adults, is shown. Subjects reported none (n = 485), one (n = 484), two (n = 253), three (n = 108), four (n = 42), or five or more underlying diseases (n = 28). Significant differences from individuals without underlying diseases are indicated as * P < 0.001
The ISQ has been translated into several languages and used worldwide for research purposes [13–22]. In addition, the ISQ is also used in clinical practice to screen patients’ immune fitness [23]. Taken together, the assessment of immune fitness and biomarkers is essential in monitoring health and disease. Both the ISQ and the single-item rating scale are effective methods to assess immune fitness and are widely used in research and clinical practice.
COVID-19: coronavirus disease 2019
IFQ: immune function questionnaire
ISQ: immune status questionnaire
SARS-CoV-2: severe acute respiratory syndrome coronavirus 2
JCV, EI, and JG: Writing—original draft, Writing—review & editing.
The authors have no potential conflicts of interest that are related to the manuscript. Over the past three years, Joris C. Verster has acted as a consultant/advisor for Eisai, KNMP, Sen-Jam Pharmaceutical, Red Bull, and Toast! Johan Garssen is a part-time employee of Nutricia Research and received research grants from Nutricia Research Foundation, Top Institute Pharma, Top Institute Food and Nutrition, GSK, STW, NWO, Friesland Campina, CCC, Raak-Pro, and EU.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2023.
Copyright: © The Author(s) 2023. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
