Abstract
Bell’s palsy is a rapid unilateral peripheral paralysis of cranial nerve VII whose etiology is varied, most commonly associated with an acute infectious or inflammatory demyelinating process. Nerve injury can result in edema because of increased permeability of vascular structures, which can sometimes be seen as a locus of enhancement of magnetic resonance imaging (MRI). Bell’s palsy is typically considered a clinical diagnosis and the specificity and sensitivity of imaging have been poorly studied. Herein is describe a case of a 73-year-old male who presented to the emergency department with left-sided facial droop and no other focal neurological abnormalities. With a history of a Janus kinase 2 (JAK2) mutation and the new initial facial drooping, acute cerebrovascular insult was high on the differential. Initial labs and computerized tomography (CT) head were inconclusive, but MRI showed pronounced enhancement of the left distal internal carotid artery (ICA) with contiguous enhancement of the labyrinthine, geniculate, and tympanic segments of the left facial nerve. Diagnosing Bell’s palsy can be a challenge as there are numerous postulated etiologies stemming from trauma, infection, and neoplasm; with infection (particularly viral) postulated to be the most likely source. Though MRI is currently not validated as a tool in expediting Bell’s palsy diagnosis, findings such as the enhancement seen here provide some insight into the benefit of MRI as a diagnostic modality in some cases. This case is unique both for the diagnostic dilemma between stroke and Bell’s palsy and the potential for MRI imaging to help guide clinical decision-making into treatment.
Keywords
Magnetic resonance imaging, diagnostic imaging, Bell’s palsy, cranial nerve VII palsy, diagnostic dilemmaIntroduction
Bell’s palsy is characterized by a rapid and unilateral peripheral paralysis of cranial nerve (CN) VII, affecting 11.5–53.3 per 100,000 people per year [1]. The facial nerve is uniquely susceptible to palsy due to its complex and extended pathway from the facial nerve nucleus in the pons, to a petrous route including a labyrinthine, horizontal tympanic, and vertical mastoid segment, extending to the stylomastoid foramen and parotid gland. The etiology of Bell’s palsy is varied, and often thought to be due to infection by reactivated viruses, particularly those in the Herpesviridae family [2]. Numerous lines of evidence additionally implicate an acute inflammatory demyelinating process in the etiology of Bell’s palsy, but other etiologies include idiopathic, traumatic, and idiopathic causes. Facial nerve injury can lead to edema, increased permeability of vascular structures, and increased extracellular fluid [1]. This damage can appear as abnormal nerve enhancement on magnetic resonance imaging (MRI), nevertheless, Bell’s palsy is a clinical diagnosis and the role of imaging in diagnosis is poorly studied.
Case report
Case summary
The patient is a 73-year-old male with a past medical history of Janus kinase 2 (JAK2)-positive polycythemia vera (PV), hypertension, hyperlipidemia, type II diabetes, atrial fibrillation on anticoagulation, and prior cerebrovascular accident (CVA) who presented to the emergency department with left sided facial droop. His symptoms began approximately 24 h prior to presentation when he noticed some slurred speech and difficulty keeping liquids inside his mouth. He denied paresthesias, dysphagia, trauma, fever, chills, recent upper respiratory infection, gastrointestinal illness, rashes, prior radiation therapy, or travel. On exam, the patient was noted to be alert and oriented with left-sided facial droop in the distribution of CN VII. Neurological examination was otherwise unremarkable with CNs II–VI and VIII–XII intact to various testing strategies. His speech was only affected phonetically with no aphasia or changes in his mentation.
Labs were notable for elevated hemoglobin (Hgb) of 196 g/L and hematocrit (HCT) of 55.3% with no hemolysis or other complete blood count (CBC) abnormalities. Of note, the patient had been worked up in the past for elevated Hgb in 2017 by the hematology and oncology service, and a JAK2 mutation was found. Troponin was within normal limits and electrocardiogram (EKG) showed no acute changes.
CT of the head showed no evidence of acute intracranial abnormality. Secondary to his history of CVA and PV, a CT angiogram to evaluate for loss of vascular flow was ordered. CT angiogram of the head and neck found no stenosis at any level, no aneurysm, no vascular malformations, or abnormal enhancements within the calvarium. MRI with gadolinium contrast of the head was negative for acute stroke but showed pronounced enhancement of the left facial nerve suggestive of Bell’s palsy. The MRI was notable for enhancement of the left distal internal carotid artery (ICA) with contiguous enhancement of the labyrinthine, geniculate, and tympanic segments of the left facial nerve (Figure 1 and Figure 2).
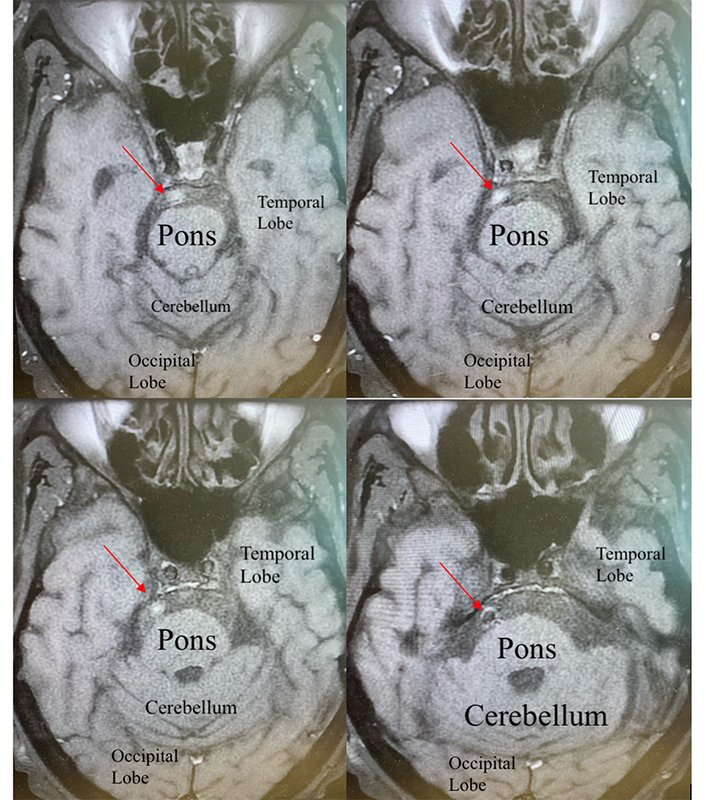
This image is an MRI of the brain using the T2-weighted-fluid-attenuated inversion recovery (T2-FLAIR), where polarized molecules are bright but the cerebrospinal fluid is subtracted in order to make lesions more visible. Gadolinium was utilized in order to improve the quality of seeing any area of potential damage or demyelinating lesions. The red arrows highlight the areas in which there is enhancement of the facial nerve on the patient’s right seen coming off the pons
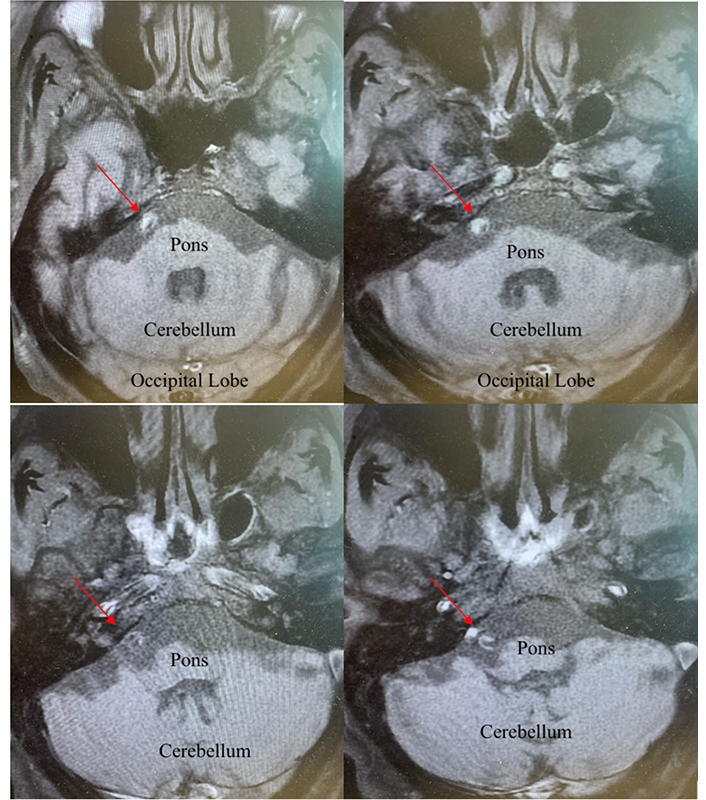
This image is an MRI of the brain using the T2-FLAIR where polarized molecules are bright, but the cerebrospinal fluid is subtracted in order to make lesions more visible. Gadolinium was utilized in order to improve the quality of seeing any area of potential damage or demyelinating lesions. The red arrows highlight the areas in which there is enhancement of the facial nerve entering the intern acoustic meatus
Differential diagnosis and final diagnosis
The differential diagnosis of isolated, unilateral facial paralysis is wide and includes cerebrovascular insults of the peripheral nerve or the central nervous system (CNS), infections (Lyme disease, herpes zoster, herpes simplex, mumps, and cytomegalovirus), autoimmune (e.g., Guillain-Barre syndrome, sarcoidosis), CNS demyelinating diseases, and tumors (e.g., cerebellopontine tumors, parotid). As Lyme disease and sarcoidosis were less likely causes due to the patient’s lack of risk factors or related presenting symptoms, these were not tested for at the time of presentation. Because of the patient’s history of JAK2 mutation-positive PV, it was necessary to evaluate for potential cerebrovascular insult. Secondary to the MRI with gadolinium, metastatic disease was eliminated from the differential as was potential ischemic disease. Based on the constellation of symptoms, rapid onset, and the lack of evidence on imaging, classical post-viral Bell’s palsy was deemed to be the most likely diagnosis.
Treatment
To treat the patient’s symptoms, the patient was started on glucocorticoids (prednisone) with an initial dose of 60 mg daily for 7 days with a taper to follow, and valacyclovir 1,000 mg three times a day for one week. Following initial reduction of symptoms, the patient was discharged two days after initial hospitalization to complete the medication regimen in his own home. He was given clear instructions for follow-up with his primary care physician in the following weeks. The events that the patient experienced that were relevant to the overall case are listed in Table 1.
Timeline of clinically relevant events
| 2017 (5 years prior to presentation) | 24 h before presentation | In the emergency department (4 h duration) | During the hospitalization (2 days duration) | At discharge |
|---|---|---|---|---|
| The patient had been worked up for elevated Hgb by the hematology and oncology service and a JAK2 mutation was found. | The patient was noticed left-sided facial droop, slurred speech, and difficulty keeping liquids in his mouth. | A CBC, a complete metabolic panel, a head CT, a head CT angiogram, an EKG, and a blood troponin level were obtained. | An MRI of the head with gadolinium contrast was obtained, and the patient was started on 60 mg of prednisone for 7 days for treatment of his Bell’s palsy. | The patient was provided detailed instructions on the need for representation to the emergency department and provided education on his condition and its cause. He was set up to see outpatient neurology and his primary care doctor. |
Patient perspective
During the treatment, the patient was provided with the information regarding his care and was appreciative of a detailed explanation as to why there was a need for an MRI. Before discharge, he was provided with information regarding how and why to represent and what the warning signs were of a worsening of his clinical condition. The patient expressed thanks that the team was willing to spend the time to perform a thorough examination and he was glad that his treatment was explained clearly with contingency planning at the time of discharge to home.
Discussion
Bells’ palsy causes a rapid neurological derangement of the seventh CN. Its pathophysiology is believed to be caused by an inflammatory response causing compression, possible demyelination, and ischemia of CN VII at the geniculate ganglion. This leads to a rapid debilitating weakness and/or complete unilateral paralysis of muscles on the face as presented in our patient. It often also presents problems with speech, loss of taste, salivation, lacrimation, and stapedial reflex. These effects can create a heavy biopsychosocial burden on the individual, so proper and timely diagnosis is key.
Diagnosing Bell’s palsy can be a challenge as there are numerous postulated etiologies stemming from trauma, infection and/or neoplasm; with infection especially, viral infection is postulated to be the most likely source. Often a diagnosis of exclusion, accurately defining Bell’s palsy is critical so as to not miss life threatening pathology such as tumors and/or acute stroke. In cases in which patients have either slow progressive palsy, demonstrate facial or bodily spasms preceding the palsy, there are multiple CNs involved, there is recurrent palsy, or there is no recovery after 6–8 weeks, other diagnoses must be considered. There is currently no gold standard imaging or clinical modality in the diagnosis of Bell’s palsy, but some case reports note facial nerve enhancement on MRI as demonstrated in this case. Reports, however, are notably limited. One report described a 25-year-old female with facial weakness two weeks following a motor vehicle collision, found to have diffuse enhancements on all segments of CN VII on MRI [1]. In one study, 10 patients with facial paralysis were identified to have facial nerve enhancements on MRI [3]. However, only 4 of those patients with Bell’s palsy, and the rest had facial nerve paralysis after temporal bone surgery [3]. Enhancement alone was a nonspecific finding in this paper [3]. As case reports are minimal with regard to this specific imaging finding, data is limited regarding the utility of MRI as a diagnostic tool for Bell’s palsy. MRI was useful in all of the above-described cases, primarily to rule out more damaging acute intracranial abnormalities—the CN enhancement on MRI currently can only be described as an incidental finding that can potentially support a clinical diagnosis, as the literature does not support anything more definitive.
Ultimately, Bell’s palsy remains a clinical diagnosis. The workup for facial nerve paralysis involves acquiring a complete history, physical examination, and appropriate labs and imaging. The history collected from the patient showed no specific risk factors and physical examination showed no signs other than the acute ipsilateral upper and lower facial paralysis. The MRI excluded metastatic disease, ischemic stroke, intracerebral hemorrhage, and soft tissue damage. In the case of the patient, it is important to note that this distinction between idiopathic facial palsy and acute stroke could be made through the physical examination as the patient presented with weakness in the ipsilateral upper and lower face and no other neurological signs or symptoms leading more towards a facial palsy and was confirmed with no apparent intracranial abnormalities on further neuroimaging apart from the CN VII enhancement.
Patients with Bell’s palsy often have a good prognosis, with resolution of symptoms within weeks to months. Nevertheless, approximately 30% of individuals who are untreated have poor recovery with long-term facial disfigurement, facial pain, speech difficulties, and psychological impacts on quality of life [4]. Initial data from the literature demonstrates that facial nerve enhancement on MRI is likely not predictive for long-term damage, with one study of 14 patients showing no difference in outcomes between those who had CN VII enhancement and those who did not [5].
Treatments for Bell’s palsy are geared toward reducing long-term complications and expediting recovery. During the acute phase of the disease, corticosteroids can be used for their anti-inflammatory effects. Randomized control trials have shown a recovery rate of 94% with corticosteroid treatment at 9 months in comparison to 81.6% in those who did not receive treatment. In addition to corticosteroids, antivirals such as acyclovir or valacyclovir are often used to target the postulated viral pathology as etiology. In meta-analysis [6], it has shown that the use of antivirals in conjunction with corticosteroids has significant reduction in the rate of incomplete recovery (relative risk 0.64, 95% confidence interval 0.41 to 0.99, n = 478).
JAK2 mutations and neurological sequelae
The JAK2 mutation is a well-described mutation of a Janus kinase pathway and is found in nearly every single case (95%) of PV [7–9]. In patients suffering from JAK2 mutations, there is an increase in the proliferation signaling cascade which leads to an increase in the number of cells that the body produces for circulation throughout the cardiovascular flow of the body [7–9]. In these cases, as a direct result of the increase in cells, there is an increased likelihood of potential blockage events within the vascular spaces of the individual. In PV, neurological sequelae have been commonly reported secondary to this pathophysiology [9–12]. Therefore, in the case of the patient, while he may have had all the key findings for a classical Bell’s palsy, this pertinent piece of pathophysiological disease state required that the team pursue further work up to ensure that this was not a microvascular insult of one of the pontine perforators. While microvascular damage is rarer than large vessel occlusions or inflammatory processes, only in considering the patient’s actual pretest probability were the appropriate steps taken and this potential diagnosis was ruled out.
Conclusion
This case study discussed the diagnosis, care, and management of a patient with acute facial paralysis, with notable CN VII enhancement on MRI. MRI was useful as a supportive diagnostic tool, but ultimately Bell’s palsy remains a clinical diagnosis as the literature does not support a more definitive use for MRI in the case of this pathology. Thorough history and proper physical examination were the key indicators for this particular case. Nevertheless, the use of imaging with a high pretest probability for cerebrovascular insult or ischemic nerve damage was key.
Abbreviations
| CN: |
cranial nerve |
| CT: |
computerized tomography |
| Hgb: |
hemoglobin |
| JAK2: |
Janus kinase 2 |
| MRI: |
magnetic resonance imaging |
| PV: |
polycythemia vera |
Declarations
Acknowledgments
The authors acknowledge the bedside nurses who constantly provide watchful eyes and care for our patients in order to ensure safe care around the clock. And this material is based upon work supported (or supported in part) by the Department of Veterans Affairs, Veterans Health Administration.
Authors contributions
AS, AA, and AB: Conceptualization, Writing—original draft. TCV: Conceptualization, Supervision, Writing—review & editing, Writing—original draft. All authors were involved in approving the final project for publication.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The ethical approval of this manuscript is exempted by the Institutional Review Board (IRB) of the Phoenix VA Health Care System Special Hospital.
Consent to participate
Informed consent to participate in this study was obtained from the patient.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2023.