Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
ORCID: https://orcid.org/0000-0002-6466-9825
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Email: annarita.signoriello@univr.it
ORCID: https://orcid.org/0000-0002-9761-4046
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Affiliation:
Dentistry and Maxillo-Facial Surgery Unit, Department of Surgery, Dentistry, Paediatrics and Gynaecology (DIPSCOMI), University of Verona, 37134 Verona, Italy
Explor Med. 2024;5:852–869 DOI: https://doi.org/10.37349/emed.2024.00260
Received: August 09, 2024 Accepted: October 22, 2024 Published: November 19, 2024
Academic Editor: Giuseppe Minervini, University of Campania “Luigi Vanvitelli”, Italy
The article belongs to the special issue Oral Health Interconnections and Multidisciplinary Approaches
Background: Parkinson’s, a degenerative disease characterized by motor and non-motor symptoms, gradually leads to disability and affects ordinary gestures, including patients’ home oral hygiene. Given that poor oral conditions, with decayed teeth, halitosis, and periodontal inflammation, can represent a critical issue in patients with low compliance in oral hygiene, the aim of this review was to investigate overall oral health in patients with Parkinson’s disease (PD).
Methods: A search on PubMed, Cochrane Library and Scopus databases was conducted to identify relevant publications: studies concerning patients with PD, their oral health conditions, and oral hygiene, also in terms of inflammation and plaque control, were included. Risk of bias analysis and qualitative analysis were performed.
Results: Of 226 records found through the electronic search, a total of 16 studies were finally included in the systematic review. Outcomes without consistent differences between PD patients and healthy patients (control group) mainly regarded: the frequency of brushing (at least twice a day), the brushing methods (generally variable) and the frequency of dental visits (mostly regular for both groups). In patients with PD, use of interdental devices was lower, and presence of plaque was higher: due to self-reported difficulties, 15–29% of them need help for oral care, against the 1% in the healthy group. Furthermore, the longer duration and higher severity of PD seem to adversely affect overall oral health conditions.
Discussion: Since poor oral conditions of patients with PD are associated with their disability in conducting proper home procedures, it is necessary for dental practitioners to focus on specific and personalized instructions, to be easily delivered to caregivers.
New technologies for diagnostics and therapy significantly extended the average lifespan of worldwide population, with remarkable improvement in quality of life. Along with the reduction of morality rates and consequent increase of life expectancy, geriatric individuals represent the fastest growing part of the population [1]. In 2019, approximately 7 million people over the age of 65 presented at least three chronic diseases, with almost half of them suffering from one severe pathology [2], such as diseases of the heart, malignant neoplasms, cerebrovascular diseases, chronic obstructive pulmonary disease, pneumonia, diabetes mellitus, Alzheimer’s disease, renal diseases, septicemia, liver diseases, and Parkinson’s disease (PD).
When the risk for developing these conditions increases with longevity, a cascade effect of morbidity is established and even treatments impair other organ system, causing susceptibility to further problems [2]. The presence of multi-morbidity negatively affects the autonomy of elderly patients in daily life activities. While physical implications related to normal aging are generally perceived, cognitive impairment is usually slow and insidious: one of the most frequent and disabling neurodegenerative pathologies, second to Alzheimer’s disease, is PD. From 1990 to date, the overall number of people affected by PD reached 9.4 million: this estimation is expected to double [3] within 2040, with a prevalence of 1% for patients aged over 60 and of 4% for older age-groups [4].
PD is characterized by a slow and progressive evolution, which causes the deterioration of dopaminergic neurons of the substantia nigra, leading to severe impairment at both motor (bradykinesia, resting tremor, rigidity, postural instability, and difficulty in walking) and non-motor (neuropsychiatric dysfunctions, such as depression, dementia, and apathy) level. As phenotypic differences make PD complex to manage [5], its onset and progression have an impact on daily activities, leading to scarce compliance with oral hygiene and increasing the risk for the main oral pathologies, that are caries and periodontitis. Furthermore, missing regular dental appointments results in decline of oral health and motivation [6], for the interference of individual changes (such as psychiatric conditions) with proper dental care.
Current therapies for PD are symptomatic treatments which slow down or restore the affected dopaminergic neurons [7]: specific drugs, taken alone or in combination with other, are however linked to oral side effects, e.g., xerostomia, bruxism, dry throat, gingivitis, lingual edema, dysgeusia and glossitis [8–10]. On the other hand, as gradual disability affects ordinary gestures, including patients’ home care procedures, poor oral hygiene is usually associated with a greater number of decayed and extracted teeth, halitosis, and periodontal inflammation.
Recent systematic reviews focus on: (i) factors associated with oral health problems [11], mainly caries, periodontal inflammation and prosthetic needs, and less frequently orofacial pain and dysfunction; (ii) on the role of health care providers [12]. As interdisciplinary approach is recommended to overcome difficulties of dental treatments, a complete overall assessment of oral conditions in PD patients can be relevant in carrying out procedures safely [13].
In the light of these considerations, the aim of this review was to investigate overall oral conditions in patients with PD, underlying that it is fundamental to focus on their limited manual skills in daily life, providing tailored supportive oral care instructions.
This review was performed based on the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) statement [14, 15], and registered as CRD42024570627 (31/07/2024) with PROSPERO (the international prospective register of systematic reviews).
The PICOS principle is described as follows:
Patients: patients with PD.
Interventions: home oral hygiene procedures and oral health conditions.
Comparators: healthy group (patients without PD).
Outcomes: frequency of brushing, brushing methods, frequency of dental visits, use of interdental devices, use of mouthwashes, self-reported difficulties with oral hygiene, oral conditions in terms of plaque control and inflammation (plaque score, gingival score), carious lesions, factors associated with the presence of periodontal disease (duration and severity).
Study design: prospective studies, Randomized clinical trials (RCTs), cross-sectional studies.
The focused question was: “How is the overall oral health and how are oral hygiene conditions reported in literature for patients with PD?”.
The Standard for Reporting Qualitative Research (SRQR) was used to conduct the qualitative review [16]. To identify relevant publications, a search on PubMed, Cochrane Library and Scopus databases was conducted. The search strategy is described as follows:
Pubmed: (“Parkinson Disease”[MeSH Major Topic] AND (“oral health”[All Fields] OR “oral hygiene”[All Fields] OR “periodontal diseases”[All Fields] OR “dental plaque”[All Fields]).
Cochrane Library: [Parkinson Disease] explode all trees AND (“Oral Hygiene” OR “Oral Health” OR “Oral Biofilm”).
Scopus: TITLE-ABS-KEY (“Parkinson Disease” AND “oral health”) OR TITLE-ABS-KEY (“Parkinson Disease” AND “oral hygiene”) OR TITLE-ABS-KEY (“Parkinson Disease” AND “periodontal diseases”) OR TITLE-ABS-KEY (“Parkinson Disease” AND “dental plaque”).
Studies included were in accordance with the following criteria:
Patients affected by PD (the specific systemic disease considered).
Factors related to patients’ oral health conditions and home oral hygiene procedures:
Frequency of brushing and brushing methods.
Frequency of dental visits.
Use of interdental devices.
Use of mouthwashes.
Self-reported difficulties with oral hygiene.
Plaque control and inflammation (plaque score and gingival score).
Carious lesions.
Factors associated with the presence of periodontal disease (duration and severity).
Articles written in English.
Not available full texts, letters, editorials, interviews, systematic literature reviews and articles published before 2013 were excluded (a temporal limitation of the last 10 years was considered as suitable for a concrete assessment, based on current and updated knowledge, regarding the topic of the review).
The records selection was conducted by two independent reviewers, removing duplicates as the first step, analyzing titles and abstracts of the remaining records, and finally selecting relevant full texts for the abovementioned inclusion criteria. In case of disagreement between the two reviewers, a third party intervened in the decision-making process.
The methodological quality of the selected full text articles was assessed using:
The Cochrane Risk Bias Tool for RCTs [17], with a fixed set of domains of bias, regarding different aspects of trial design, conduct, and reporting; bias was declared for individual elements from five domains of bias (selection, performance, attrition, reporting, and other).
The AXIS-Tool for cross-sectional studies was instead used [18], with a score varying from 14 points to 18 points, based on the result of 20 questions, which were as follows:
Q1 = where the aims/objectives of the study clear?
Q2 = was the study design appropriate for the stated aim(s)?
Q3 = was the sample size justified?
Q4 = was the target/reference population clearly defined (is it clear who the research was about?)?
Q5 = was the sample frame taken from an appropriate population base so that it closely represented the target/reference population under investigation?
Q6 = was the selection process likely to select subjects/participants that were representative of the target/reference population under investigation?
Q7 = were measures undertaken to address and categorise non-responders?
Q8 = were the risk factor and outcome variables measured appropriate to the aims of the study?
Q9 = were the risk factor and outcome variables measured correctly using instruments/measurements that had been trilled, piloted, or published previously?
Q10 = is it clear what was used to determine statistical significance and/or precision estimates (e.g., P-values, confidence intervals)?
Q11 = were the methods (including statistical methods) sufficiently described to enable them to be repeated?
Q12 = were the basic data adequately described?
Q13 = does the response rate raises concerns about non-responders bias?
Q14 = if appropriate, was information about non-responders described?
Q15 = were the results internally consistent?
Q16 = were the results presented for all the analyses described in the methods?
Q17 = were the author’s discussions and conclusions justified by the results?
Q18 = were the limitations of the study discussed?
Q19 = were there any funding sources or conflicts of interest that may affect the authors’ interpretation of the results?
Q20 = was ethical approval or consent of participants attained?
A number of 226 articles were obtained from the initial search, 84 in PubMed, 69 in Cochrane Library and 73 in Scopus. After removing duplicates, 200 were evaluated. After following the study selection procedure, 16 were included (see Figure 1).
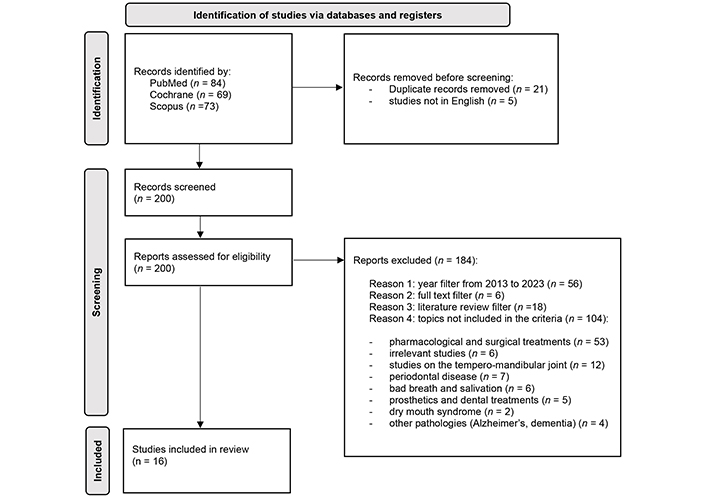
Research flow diagram according to PRISMA statement. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta Analyses
Note. Adapted from “The PRISMA 2020 statement: an updated guideline for reporting systematic reviews” by Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. BMJ. 2021;372:n71 (https://doi.org/10.1136/bmj.n71). CC BY.
Overall characteristics of participants of selected studies are presented in Table 1. Concerning the evaluation of disease stage and severity, two methods were used in the studies examined:
The Movement Disorders Society-Unified Parkinson Disease Rating scale-part III (MDS-UPDRS-III) [19]: it is a clinical rating scale structured in four parts. The first part concerns the non-motor experiences of everyday life, the second considers motor experiences, the third section evaluates motor skills, and the last section evaluates complications.
The Hoehn & Yahr Scale [20]: this method describes the progression of the disease through the various stages and allows the severity of the case to be measured. The evaluation takes place on the basis of in-depth examination and anamnesis provided by the patients, including 5 stages: in the first stage the patient has unilateral symptoms; in the second stage the patient has bilateral involvement without compromise in balance; in the third stage bilateral disease is mild to moderate with postural instability; stage 4 indicates severe disability and the patient is still able to walk or stand unaided; in stage 5 the patient is confined to a wheelchair or bed if unassisted.
Overall characteristics of participants of the selected studies
| Article | Design | Country | Number of PD patients | Number of healthy patients (control) | Age of PD patients (years) | Age of healthy patients (years) | Disease stage (Hoehn & Yahr) [20] | Disease severity (MDS UPDRS-III) [19] | Disease duration (years) |
|---|---|---|---|---|---|---|---|---|---|
| Baram et al. [21], 2020 | RCT | Denmark | 29 | - | 32–72 | - | 2.9 ± 0.4 | 20.6 ± 4.9 | 11.7 ± 5.0 |
| Baram et al. [22], 2023 | CS | Denmark | 6,874 | 34,285 | 71 (58–82) | 71 (58–82) | - | - | - |
| Barbe et al. [23], 2017 | CS | Germany | 100 | - | 71 ± 8.7 | - | - | 17.5 ± 8.6 | - |
| Barbe et al. [24], 2017 | CS | Germany | 26 | 26 | 69 ± 9.0 | 69 ± 9.0 | - | 13.0 ± 9.0 | 9.0 ± 4.0 |
| Barbe et al. [25], 2017 | CS | Germany | 30 | 30 | 69.3 ± 8.0 | 69.3 ± 7.9 | - | 12.0 ± 8.8 | - |
| Fleury et al. [26], 2021 | CS | Switzerland | 20 | 20 | 62.8 | 64.3 | 2 | 15 | 4.7 |
| García-De-La-Fuente et al. [27], 2022 | CS | Spain | 104 | 106 | 66.2 ± 9.2 | 59.2 ± 14.1 | - | - | - |
| García-de-la-Fuente et al. [28], 2023 | CS | Spain | 104 | 106 | 66.2 ± 9.2 | 66.2 ± 9.2 | - | - | - |
| John et al. [29], 2021 | CS | India | 32 | 42 | 58.4 ± 10.6 | 66.2 ± 9.2 | - | - | - |
| Lyra et al. [30], 2020 | CS | Portugal | 28 | - | 72.3 ± 8.1 | - | 2.7 | - | - |
| Pradeep et al. [31], 2015 | CS | India | 45 | 46 | 54.5 ± 9.1 | 63.9 ± 13.1 | - | - | - |
| Ribeiro et al. [32], 2016 | CS | Brazil | 17 | 20 | 69.41 ± 4.65 | 72.00 ± 5.69 | - | - | 6.76 ± 3.80 |
| Ribeiro et al. [33], 2017 | CS | Brazil | 17 | 17 | 69.4 ± 4.7 | 70.7 ± 4.7 | - | - | 6.76 ± 3.80 |
| Rozas et al. [34], 2021 | CS | USA | 30 | 30 | 69.2 ± 9.4 | 69.1 ± 8.4 | - | - | - |
| van Stiphout et al. [35], 2018 | CS | Netherlands | 74 | 74 | 70.2 ± 8.8 | 67.9 ± 10.1 | 2.4 | - | - |
| Verhoeff et al. [36], 2022 | CS | Netherlands | 341 | 411 | 65.5 ± 8.4 | 62.6 ± 5.3 | - | 11.5 ± 7.5 | 7.0 ± 5.5 |
-: unknown; CS: cross sectional; RCT: randomized clinical trial; MDS-UPDRS-III: Movement Disorders Society-Unified Parkinson Disease Rating scale-part III; PD: Parkinson’s disease. Age, disease stage/severity/duration are expressed in years as mean ± SD (standard deviation)
The quality assessment for cross-sectional studies conducted with AXIS TOOL evidenced a moderate/good quality for articles analyzed (see Table 2).
The quality assessment for cross-sectional studies conducted with AXIS TOOL (item is reverse scored)
| Article | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 | Q17 | Q18 | Q19 | Q20 | Axis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baram et al. [22], 2023 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | - | Y | 17 |
| Barbe et al. [23], 2017 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | - | Y | 17 |
| Barbe et al. [24], 2017 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | - | Y | 17 |
| Barbe et al. [25], 2017 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | - | Y | 17 |
| Fleury et al. [26], 2021 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | Y | N/A | Y | Y | Y | N | N | Y | 17 |
| García-De-La-Fuente et al. [27], 2022 | Y | Y | N | Y | Y | Y | - | Y | Y | Y | Y | N | N | N/A | Y | Y | N | N | N | Y | 14 |
| García-de-la-Fuente et al. [28], 2023 | Y | Y | N | Y | Y | Y | - | Y | Y | Y | Y | N | N | N/A | Y | Y | N | N | N | Y | 14 |
| John et al. [29], 2021 | Y | Y | Y | Y | Y | - | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | N | Y | 17 |
| Lyra et al. [30], 2020 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | N | Y | 17 |
| Pradeep et al. [31], 2015 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | ? | Y | Y | N | N | Y | 15 |
| Ribeiro et al. [32], 2016 | Y | Y | Y | Y | Y | - | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | - | - | Y | 15 |
| Ribeiro et al. [33], 2017 | Y | Y | Y | Y | Y | N | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | - | Y | 16 |
| Rozas et al. [34], 2021 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | N | Y | 17 |
| van Stiphout et al. [35], 2018 | Y | Y | Y | Y | Y | Y | - | Y | Y | Y | Y | Y | N | N/A | Y | Y | Y | Y | N | Y | 18 |
| Verhoeff et al. [36], 2022 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | 18 |
-: unclear; Q: question; Y: yes; N: no; N/A: not applicable
The quality of the RTC study assessed with the Cochrane Risk of Bias Tool reported an unclear risk of bias (see Table 3).
Instrument for methodological quality for RCT studies using Cochrane Risk of Bias Tool
| Paper | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias |
|---|---|---|---|---|---|---|
| Baram et al. [21], 2020 | - | + | + | - | - | + |
+: bias present; -: bias not present; RCT: randomized clinical trial
Approximately 60% of PD patients (see Table 4) brush their teeth at least twice a day [25, 34, 36]. In this proposal, García-de-la-Fuente et al. [27, 28], analysed 104 PD subjects and 106 control cases, with non-homogeneous age: 5.8% of patients in the first group (vs. 1.9% in the control) declared to not perform oral hygiene manoeuvres at home. Rozas et al. [34] presented two groups homogeneous for age, gender, and number of participants: 73% of healthy patients mechanically removed their plaque, while only 60% of PD patients used to brush twice daily.
Home oral hygiene habits: frequency and methods of brushing
| Home oral hygiene habits | Article | Parkinson group | Healthy group |
|---|---|---|---|
| Brushing frequency | Barbe et al. [23], 2017 | 21% 1 × day | N/A |
| 64% 2 × day | N/A | ||
| 15% 3 × day | N/A | ||
| Fleury et al. [26], 2021 | 100% ≥ 1 × day | 100% ≥ 1 × day | |
| García-De-La-Fuente et al. [27], 2022 | 2 × day | 2 × day | |
| 5.8% none | 1.9% none | ||
| 22.1% 1 × day | 17% 1 × day | ||
| 26% 2 × day | 31.1% 2 × day | ||
| 46.20% > 2 × day | 50% > 2 × day | ||
| Lyra et al. [30], 2020 | 32.1% 1 × day | N/A | |
| 67.9% ≥ 2 × day | N/A | ||
| Pradeep et al. [31], 2015 | 76% > 1 × day | 76% > 1 × day | |
| Rozas et al. [34], 2021 | 60% ≥ 2 × day | 73% ≥ 2 × day | |
| Verhoeff et al. [36], 2022 | 72.7% ≥ 2 × day | N/A | |
| Brushing methods | Barbe et al. [23], 2017 | 43% electric toothbrush | N/A |
| García-De-La-Fuente et al. [27], 2022 | 4% electric toothbrush | 7.6% electric toothbrush | |
| Lyra et al. [30], 2020 | 25% electric toothbrush | N/A | |
| van Stiphout et al. [35], 2018 | 48.6% electric toothbrush | 40.5% electric toothbrush | |
| Verhoeff et al. [36], 2022 | 78% electric toothbrush | N/A |
N/A: not applicable. Frequency of brushing is reported in percentage (%) of participants for each group brushing teeth 1, 2 or 3 times × day, or only in number of times × day for each group; type of device is reported in percentage (%) of participants for each group
Regarding brushing methods (see again Table 4), only two studies [25, 35] indicate a good percentage (40–50%) of electric toothbrush users among PD patients. Verhoeff et al. [36] found 78% of users among 341 PD patients. van Stiphout et al. [35] analyzed 74 PD patients (at a mild disease stage) and 74 healthy patients, finding that electric toothbrush was respectively used in 48.6% and 40.5% of cases.
García-De-La-Fuente et al. [27] highlighted (see Table 5) a lower frequency of interdental cleaning, as well as a lower use of brush and dental floss, in PD patients compared to healthy subjects. Verhoeff et al. [36] described use of dental floss, toothpicks, metal brush and rubber brush. Regarding the use of mouthwash (see again Table 5), no substantial differences between groups were reported [20, 22].
Home oral hygiene habits: interdental devices and use of mouthwash
| Home oral hygiene habits | Article | Parkinson group | Healthy group | Type of device |
|---|---|---|---|---|
| Interdental devices | Barbe et al. [23], 2017 | No | N/A | |
| García-De-La-Fuente et al. [27], 2022 | 33.7% | 49.1% | Interdental cleaning | |
| 19.2% | 29.2% | Interdental brush | ||
| 10.6% | 16% | Dental floss | ||
| 1.9% | 2.8% | Water flosser | ||
| 10.6% | 16.2% | Mouthwash alcol-free | ||
| 51.9% | 51.9% | Mouthwash | ||
| Lyra et al. [30], 2020 | 39% | N/A | ||
| Pradeep et al. [31], 2015 | 13% | 19.5% | Dental floss | |
| Rozas et al. [34], 2021 | 47% | 50% | Dental floss | |
| Verhoeff et al. [36], 2022 | 39% ≥ 1 times/die | N/A | ||
| 50% toothpick | ||||
| 34.8% rubber pipe cleaner | ||||
| 43.2% metal pipe cleaner | ||||
| Use of mouthwash | García-De-La-Fuente et al. [27], 2022 | 10.6% | 16.2% | Mouthwash alcol-free |
| 51.9% | 51.9% | |||
| Pradeep et al. [31], 2015 | 35.60% | 39.10% | ||
| Barbe et al. [23], 2017 | 38% | N/A |
N/A: not applicable. Use of interdental devices or mouthwah is reported in percentage (%) of participants for each group, with eventual specification of device type
Self-reported difficulties (see Table 6) were assessed through the delivery of questionnaires. According to Barbe et al. [25] and van Stiphout et al. [35] 29% and 15% of PD patients respectively required help and assistance.
Home oral hygiene habits: self-reported difficulties and subjective oral hygiene measures awareness
| Home oral hygiene habits | Article | Parkinson group | Healthy group | Self-report |
|---|---|---|---|---|
| Self-reported difficulties | Barbe et al. [23], 2017 | 29% need help | N/A | |
| van Stiphout et al. [35], 2018 | 15% need help | 1% need help | ||
| Subjective oral hygiene | García-De-La-Fuente et al. [27], 2022 | 31.7% | 45.3% | Good |
| 48.1% | 40.6% | Moderate | ||
| 20.2% | 14.2% | Bad |
N/A: not applicable. Variable is reported in percentage (%) of participants for each group, with eventual specification of degree
Subjective oral hygiene measures awareness of the patient’s level of oral hygiene (see again Table 6) was determined by García-de-la-Fuente et al. [28], administering a questionnaire on home oral hygiene habits: the degree of subjective hygiene was categorized into three options: “insufficient”, “sufficient”, “good”.
Most of the articles (see Table 7) revealed a greater presence of biofilm in the test group, with significant data in plaque indices [9, 13, 14, 16–18]. García-De-La-Fuente et al. [27] reported the full mouth plaque index (FMPI) as below 25% in 2.9% of PD patients, vs. 12.3% of healthy ones; as above 50% in 76.9% of PD patients, vs. 60.4% of healthy ones. Ribeiro et al. [32] considered the Visible Plaque Index in 17 PD and 20 healthy patients with a homogeneous average age, reporting values of 91.8 ± 16.9 in PD and 64.10 ± 48.9 in healthy patients, respectively. Rozas et al. [34] found differences in the Oral Hygiene Index-Simplified plaque index between the two groups before brushing, while a notable decrease, in both, after brushing. van Stiphout et al. [35] declared 60% plaque deposits in PD patients, compared to 31% in healthy patients.
Home oral hygiene habits: presence of plaque and gingival inflammation
| Home oral hygiene habits | Article | Parkinson group | Healthy group | Additional information |
|---|---|---|---|---|
| Presence of plaque | Baram et al. [21], 2020 | 1.1 ± 0.6 OH-DSI | N/A | |
| Barbe et al. [23], 2017 | 1.7 (0.9%) PI | 1.0 (0.8%) PI | ||
| Fleury et al. [26], 2021 | 1.29 PI | 0.97 PI | ||
| García-De-La-Fuente et al. [27], 2022 | 72.2 ± 22.2 PI | 62 ± 25.9 PI | ||
| 2.9% | 12.30% | FMPI < 25% | ||
| 17.3% | 24.5% | FMPI 25–50% | ||
| 76.90% | 60.4% | FMPI > 50% | ||
| John et al. [29], 2021 | 3.1 ± 0.81 OHI | 1.3 ± 0.4 OHI | ||
| Lyra et al. [30], 2020 | 37.0 ± 29.4 PI | N/A | ||
| Ribeiro et al. [32], 2016 | 91.8 ± 16.9 PI | 64.1 ± 48.9 PI | ||
| Rozas et al. [34], 2021 | 1.6 ± 0.13 OHI-S | 1.0 ± 0.16 OHI-S | Before brushing | |
| 0.54 ± 0.08 OHI-S | 0.39 ± 0.1 OHI-S | After brushing | ||
| van Stiphout et al. [35], 2018 | 60% | 31% | ||
| Presence of bleeding | Fleury et al. [26], 2021 | 57.90% | 51.50% | |
| Lyra et al. [30], 2020 | 19.3 ± 21.2 BoP | N/A | ||
| van Stiphout et al. [35], 2018 | 20% | 18.50% | ||
| Presence of gingivitis | Barbe et al. [25], 2017 | 1.8 ± 0.8 | N/A | |
| Barbe et al. [24], 2017 | 1.9 ± 0.8 GI | 0.8 ± 1.1 GI | ||
| John et al. [29], 2021 | 1.5 ± 0.4 MGI | 0.7 ± 0.2 |
N/A: not applicable; PI: plaque index; OHI: oral hygiene index; OHI-S: oral hygiene index semplified; OH-DSI: oral hygiene-debris semplified index; FMPI: full mouth plaque index; BoP: bleeding on probing; GI: gingivitis index; MGI: modified gingival index. Presence of plaque or bleeding is reported in percentage (%) of participants for each group presenting the condition, if not otherwise specified through the use of specific parameters, expressed in % or mean ± SD (standard deviation), depending on the study
Gingival inflammation (see again Table 7) was evaluated with the presence of bleeding on probing (BoP) [26, 30] and the presence of gingivitis. van Stiphout et al. [35] considered the self-assessment performed by patients, identifying gum bleeding during brushing: the test group revealed 20% cases in PD patients, compared to 18.5% of the control group. Regarding the presence of gingivitis, studies [25, 29] generally reported higher values in PD patients compared to healthy patients: Barbe et al. [25] examined the gingivitis index (GI), which analyses the presence of bleeding, changes in colour and consistency of the mucosa, while John et al. [29] examined the modified gingival index (MGI).
As regards the frequency of dental visits (see Table 8), the two groups analysed appeared mostly regular [22], for and approximate frequency of ≥ 2 times a year [25, 34, 36]. Some studies [30, 35] found that periodic checks were performed with a follow-up of less than 6 months.
Frequency of dental visits
| Article | Parkinson group | Healthy group | Frequency |
|---|---|---|---|
| Barbe et al. [23], 2017 | 53.10% | 2 times/year | |
| 34.70% | once/year | ||
| Baram et al. [22], 2023 | 21.40% | 23.60% | No dental care |
| 21% | 16.90% | Irregular | |
| 57.50% | 59.50% | Regular | |
| 5.40% | 2.70% | 0 times/year | |
| 17.60% | 23% | 1–5 times/year | |
| 40.50% | 48.60% | 6–10 times/year | |
| 36.50% | 25.70% | > 11 times/year | |
| Fleury et al. [26], 2021 | 100% | 100% | ≥ once/year |
| Lyra et al. [30], 2020 | 64.30% | < 6 months | |
| 14.30% | 6–12 months | ||
| 21.40% | > 12 months | ||
| Pradeep et al. [31], 2015 | 28.8% | 32.60% | > 1 once/year |
| Rozas et al. [34], 2021 | 57% | 50% | ≥ 2 times/die |
| van Stiphout et al. [35], 2018 | 70.30% | 66.20% | Last visit less than 6 months |
| 20.30% | 29.80% | Between 6 months and 2 years | |
| 5.40% | 2.70% | 0 times/year | |
| 17.60% | 23% | 1–5 times/year | |
| 40.50% | 48.60% | 6–10 times/year | |
| 36.50% | 25.70% | > 11 times/year | |
| Verhoeff et al. [36], 2022 | 73% | ≥ 2 times/year |
Frequency of dental visits is reported in percentage (%) of participants for each group presenting the frequency specified in the third column
Only one article (see Table 9) showed a higher prevalence of caries in PD patients, using the epidemiological tool Decay Teeth, reporting 74 decayed surfaces compared to 12 in the healthy group [35]. The other studies analyzed did not give results with significant differences [27, 29, 32].
Prevalence of caries
| Article | Parkinson group | Healthy group |
|---|---|---|
| Fleury et al. [26], 2021 | 10% | 10% |
| García-De-La-Fuente et al. [27], 2022 | 18.8 ± 7.3 DMFT | 17.8 ± 7.7 DMFT |
| 2.3 ± 3.0 DT | 1.7 ± 2.3 DT | |
| John et al. [29], 2021 | 7.72 ± 4.45 DMFT | 4.57 ± 3.58 DMFT |
| Ribeiro et al. [32], 2016 | 24.8 ± 3.8 DMFT | 26.9 ± 2.2 DMFT |
| van Stiphout et al. [35], 2018 | 74 DT | 12 DT |
DT: decayed teeth; DMFT: decayed, missing, filled teeth. Prevalence of caries is reported in percentage (%) of participants for each group presenting the condition, if not otherwise specified through the use of specific parameters, expressed in mean ± SD (standard deviation) or only mean, depending on the study
Three studies analysed the duration of the disease and its possible correlation with the oral cavity (see Tables 10 and 11). Two studies [25, 29] reported an increase in difficulties in managing oral hygiene at home in relation to the increase in the duration of PD disease (see Table 10): patients with the disease for approximately 10 years (average duration) and limited abilities reported greater limitations in abilities compared to ones with the disease for approximately 7 years. van Stiphout et al. [35] declared an average duration of the disease of 9.1 ± 6.4 years and an increase in the number of teeth with conservative treatments and restorations.
Factors associated with PD: duration
| Article | Variable |
|---|---|
| Barbe et al. [23], 2017 | Self-reported difficulties in IOD associated with disease duration increase 7 years average duration of the disease (4.00–14.00): no limitations |
| 10 years average duration of the disease (6.75–15.50): limited abilities | |
| John et al. [29], 2021 | DMFT < 3 year (8.0 ± 65.1) |
| DMFT > 3 year (7.33 ± 3.73) | |
| OHI < 3 year (2.98 ± 0.82) | |
| OHI > 3 year (3.2 ± 10.85) | |
| MGI < 3 year (1.47 ± 0.39) | |
| MGI > 3 year (1.57 ± 0.39) | |
| van Stiphout et al. [35], 2018 | Increase in the number of teeth with conservative treatment associated with the duration of the disease (average duration 9.1 ± 6.4) |
DMFT: decayed, missing, filled teeth; IOD: home oral hygiene; OHI: oral hygiene index; MGI: modified gingival index; PD: Parkinson’s disease. Specific parameters are expressed in mean ± SD (standard deviation), depending on the study
Factors associated with PD: severity
| Article | Group | OHI | MGI | DMFT | BOP | PI | GI | Findings |
|---|---|---|---|---|---|---|---|---|
| John et al. [29], 2021 | Mild severity | 2.90 ± 0.81 | 1.44 ± 0.38 | 7.24 ± 4.06 | 2.2% | 23.9% | - |
|
| Moderate severity | 3.77 ± 0.52 | 1.82 ± 0.25 | 9.43 ± 5.68 | 2.0% | 16.80% | - | ||
| Pradeep et al. [31], 2015 | Control group | - | - | - | 20.37 ± 6.40 | 1.35 ± 0.61 | 0.55 ± 0.48 | - |
| I H&Y stage | - | - | - | 33.36 ± 6.68 | 2.17 ± 0.46 | 1.24 ± 0.47 | ||
| II H&Y stage | - | - | - | 37.50 ± 4.38 | 2.31 ± 0.79 | 1.34 ± 0.36 | ||
| III H&Y stage | - | - | - | 48.60 ± 5.78 | 2.77 ± 0.74 | 1.92 ± 0.46 | ||
| van Stiphout et al. [35], 2018 | - | - | - | - | - | - | - |
|
DMFT: decayed, missing, filled teeth; OHI: oral hygiene index; MGI: modified gingival index; GI: gingivitis index; BoP: bleeding on probing; H&Y: Hoehn & Yahr stage; PI: plaque index; ↑: increase; PD: Parkinson’s disease. Specific parameters are expressed in % or mean ± SD (standard deviation), depending on the study
As reported in Table 11, the MDS-UPDRS-III scale was used in the studies analysed for the third part to evaluate, facial expressions, rigidity, tremors.
John et al. [29] examined 32 patients suffering from PD, divided according to the Hoehn & Yahr Scale: 25 patients placed in the first and second stages were considered as mild severity, while 7 patients in the third and fourth stages were registered as moderate severity. This study reported an increase of oral hygiene index (OHI) and MGI of the most severe patients. Analysing bleeding and the presence of plaque, Lyra et al. [30] documented an increase in these indices related to the presence of tremors, depressive state, and rigidity. Pradeep et al. [31] also reported an increase in clinical indices related to gingival inflammation associated with disease progression: examining 45 subjects suffering from PD and 46 healthy ones, and dividing the first group into five subgroups based on the Hoehn & Yahr Scale, stages 1 and 2 represented mild severity, stage 3 moderate severity and stages 4 and 5 referred to severe disease. van Stiphout et al. [35] finally highlighted the increased need for home oral hygiene support in patients who have more severe disease, as well as a greater number of decayed teeth and with fillings when the severity of the disease increases. Therefore, in all the studies analysed, a significant worsening of the oral situation was noted when the disease was present for several years or in case of its aggravation.
Patient with PD generally present a lower oral health related quality of life (OHRQoL) compared to healthy individuals [25], due to xerostomia, dysphagia and sialorrhea, which alter the salivary clearance, negatively impact the microflora and cause halitosis [37]. Xerostomia is one of the most common oral manifestations in PD patients, found in 55% of cases [10], implying a decrease of saliva quantity and quality, linked to the disease itself or the drugs taken. Capacity of remineralising/buffering and antimicrobial power therefore determine carious lesions, periodontal pockets, as well as oral ulcers and problems with retention of prostheses [8, 10]. Furthermore, a reduced mobility and rigidity of the muscles, which promote the self-cleansing function, leads to infections and inflammation [34], with proliferation of a distinct microbiota in both saliva and subgingival plaque compared to healthy controls [26]. While dysphagia causes weight loss, social distancing (the patient prefers to isolate himself while eating), problems in taking medications, and acid reflux, with enamel erosion and dentin hypersensitivity [9], sialorrhea is connected to impaired swallowing and reduced lip closure.
Concerning oral habits, outcomes examined in this review revealed for all studies an average frequency of brushing of at least twice a day for PD patients, while non homogenous data are reported for brushing technique used, with authors declaring a prevalent use of the electric toothbrush [36], vs. authors highlighting a prevalent use of the manual one [27]. Discrepancies between studies regarding brushing methods could be related to different samples considered, as PD patients were not always compared with healthy controls, and to different duration and severity of disease assessed. However, authors suggest that clinical recommendations should be driven by the necessity of simplify manoeuvres: electric device can represent a valid option in this sense, especially in case of severe phase of disease.
Use of interdental devices in patients with PD seems to be lower compared to healthy patients in all articles examined, with a mean difference of approximately 15% between groups [27]. Due to evident difficulties at home beside they are aware of the need for good oral conditions [38], lack of adequate interdental cleaning easily leads to accumulation of biofilm, which was reported in greater quantities for PD patients by several studies [25–27, 29, 34, 35]. Although frequency and modality of cleaning teeth can be superimposed with the comparison group, results did not show a sufficient plaque control, also for the presence of apathy, depression, and forgetfulness.
In addition, gingival inflammation, registered through the presence of bleeding and gingivitis, is a consequence of deficient oral hygiene. Most studies reported a predominant presence of gingivitis in PD patients compared to healthy ones [25, 29], with presence of bleeding in 57.9% of cases vs. 51.50% in the control group [26]. Incorrect oral hygiene, in terms of lack of quality (not frequency) of manoeuvres [11], usually promotes gingivitis, which, if prolonged, can evolve into periodontitis or worsen an already compromised periodontal status.
Being chronic periodontitis an infectious disease linked to a variety of systemic disorders [39], several studies suggest a potential connection between chronic periodontitis and neurodegenerative diseases, such as PD [40]. Individuals with PD indeed present a bacterial composition different from healthy people; at the same time, patients with chronic periodontitis seem to have a higher risk of developing multi-organ systemic complications and PD, which can be reduced through improvement of oral health and regular periodontal treatment [39]. Understanding the mechanisms of biofilm alteration, constant inflammation, or even the bacterial products blood-circulation, would be advisable for periodontitis prevention: it was reported that microorganisms typical of red complex, such as P. gingivalis, are involved in neuroinflammation. Oral manifestations can be thus useful for an earlier diagnosis of systemic pathologies, or can represent the first steps of eventual chronic conditions, especially considering the slow and insidious progression of PD [41, 42]. As the microbial profile is associated with cognitive status [26], decrease in quantity of saliva, specific bacteria found in increased proportions (e.g., S. Mutans, Veillonella, Lactobacillaceae, T. Forsythia, P. Intermedia, Fusobacterium, Capnocytophaga, C. Rectus) and worsened periodontal conditions all suggest an increased risk for periodontal disease. Besides that, periodontal bacteria produce endotoxins, which increase the inflammatory impact and induce cells to generate and release pro-inflammatory cytokines, hypothesized to be associated with the damage or apoptosis of dopaminergic cells [43]: in this way, chronic inflammatory response due to periodontal disease seems to be one of the etiological causes of PD.
All studies included in this review found a greater number of missing teeth, plaque accumulation, pronounced bone loss and increased periodontal pockets in PD patients. Specific investigations also demonstrated a greater number of pockets larger than 4 mm and of mobile elements in PD patients compared to control group [29, 35, 44]. The number of elements present in the oral cavity does not seem to differ between PD patients and healthy patients: nevertheless, a greater number of root residues was found in the test group, probably because dental treatments are more difficult to perform in PD patients [35]. Neglection of pathological clinical signs leads to mobility and final loss of the dental elements [45], with consequent difficulty in chewing and swallowing and a further worsening of the quality of life [46, 47]. In this terms, rehabilitation through the use of removable partial dentures can significantly decrease the scores of Oral Health Impact Profile-49 (OHIP-49) [32], a tool employed for measuring the effect of oral health on quality of life. PD patients, however, declared their prostheses as less comfortable than healthy patients [48], reporting a reduced motor control of the facial muscles. The presence of removable prostheses requires a strong effort to be kept in position or to be active during chewing and phonation even in healthy subjects: for PD patients orofacial muscles do no longer properly operate and react in self-control during oral functions, as the device is probably perceived by the patient as foreign compared with natural dentition. Plus, despite patients generally show greater satisfaction in terms of food intake and oral well-being, difficulty in cleaning prostheses, due to cognitive deterioration and motor disorders, can lead to the formation of a reservoir of pathogenic microorganisms [49]. In this regard, use of mouthwash is recommended to prevent opportunistic infections, and it was registered as similar in test and control group: however, it can be noticed that this supplement can generate discomfort in PD for dysphagia or fear of choking.
Patients’ self-assessment of their oral hygiene was reported as moderate in the PD group and good in the control group: this is indicative of awareness, by PD patients, of being not sufficiently efficient and effective in oral hygiene manoeuvres. Despite the frequency of dental visits appears to be homogeneous among all authors, with regular visits at least twice per year, overall oral health in PD patients was finally found as deficient and inadequate [11]. Proper use of toothbrush and interdental aids require complex coordination and manual skills, with increasing difficulties as the disease advances. Even if appointments in dental practices could be frequent, cognitive decline and dementia prevent the patient from reporting symptoms/dental pain to professionals/caregivers and being truly compliant: that’s probably the reason why patients’ perception of oral health results worse than healthy people.
A compromised status with multiple missing teeth can modify eating habits in time [11], as the patient present greater difficulty in chewing and swallowing, finally choosing softer and sweeter foods, which are rich of sugars, and limited self-cleansing of the oral cavity, with an increase in carious receptivity. Despite some authors [38] stated that factors predisposing oral diseases in PD patients include propensity for cariogenic foods, use of drugs reducing salivation, physical and motor problems, and cognitive change, only one paper [35] among five found a higher prevalence of caries in PD patients. Concomitant factors potentially leading to a greater predisposition to carious lesions [50, 51] are poor oral hygiene, plaque accumulation, and change in oral flora with a prevalence of S. Mutans and Lactobacillaceae.
Regarding relevant factors associated with the disease, its duration and severity both lead to general worsening of oral conditions. As the severity increases, functional capacity decreases in terms of motor difficulties and cognitive deficiencies, along with depression and dementia [12]. An evident link between severity/duration of PD and prevalence of untreated cavities and gingival inflammation clearly pointed out that compromised abilities in PD patients have an impact on the quality of self-care in a severe manner [11].
Considering the exacerbation of clinical manifestations proceeding with the disease, the relevance of caregiver becomes extremely important in giving appropriate instructions, to determine an effective support in everyday difficulties. In practical terms, it is necessary for dental staff to focus on tailored oral hygiene protocols, paying attention to the real needs of patients and directly communicating with caregivers, to explain them how to improve oral hygiene with appropriate tools and precautions. Inadequate plaque control, with consequent gingival inflammation and bleeding, is certainly due to tremors, rigidity, dementia, which do not allow adequate manual skills. Furthermore, an unbalanced diet in favor of carbohydrates and sugars (simpler and more palatable), as well as an altered quantity and quality of saliva, can lead to greater carious receptivity. In the light of these considerations, all issues evidenced for PD patients in this review necessarily imply the need for specific assistance. Caregivers should be directly involved in patients oral care after a targeted training given by dentists and dental hygienists. Visual instructions should be performed with the caregiver and the patient present together in the dental office (if the disease allow mobility), or even at home. Appropriate methods of brushing should be verified in patient’s mouth to suggest the easiest and most effective way to eliminate plaque deposits. Manual capacity should be determined in terms of interdental cleaning, and suitable interdental devices should be chosen according to the grade of autonomy and compliance. Finally, informative flyer could be designed with the support with Dental Associations, to widely release knowledge about the orofacial management of PD patients.
Finally, a limitation of the studies included in this review should be mentioned, as some authors [21–25, 27, 28, 32, 33] published on the topic in closed proximity, and probably the same populations were investigated in more than one study. Even if the results cannot be considered as representative of the countries they originated from, it must be underlined that multiple investigations by the same research group were conducted with different samples (PD patients only or PD patients in comparison with healthy group) and considering different factors influencing the disease (duration, stage severity). Despite the groups analyzed were almost homogeneous for age and type of study design (cross-sectional), differences were particularly evident regarding type of populations considered, indexes assessed for plaque and bleeding, oral parameters collected for examination of PD duration/severity. This heterogeneity does not allow a proper comparison between studies in terms of uniform analysis of multiple variables: taken for established the medical characterization of PD (with the known codified scales), this issue could be addressed with standardized methods, through the choice of universal clinical indexes for collection of parameters for an easy and practical evaluation of hard and soft tissues in the mouth.
Considering these findings, the challenges faced by PD patients in home oral hygiene underscore the need for specific care. Areas of future research should encourage longitudinal studies to better understand the impact of oral health interventions on the progression of PD, not only through the action of private practice, but also with the support of families, caregivers and public structures involved in the assistance of PD patients.
BoP: bleeding on probing
FMPI: full mouth plaque index
GI: gingivitis index
MDS-UPDRS-III: Movement Disorders Society-Unified Parkinson Disease Rating scale-part III
MGI: modified gingival index
OHI: oral hygiene index
OHIP-49: Oral Health Impact Profile-49
OHRQoL: oral health related quality of life
PD: Parkinson’s disease
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta Analyses
RCTs: randomized clinical trials
SRQR: Standard for Reporting Qualitative Research
AP: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. AB: Conceptualization, Investigation, Writing—original draft. AS: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. MG: Writing—original draft, Writing—review & editing. GB: Investigation, Writing—review & editing. GC: Investigation, Writing—review & editing. GL: Validation, Writing—review & editing. MA: Validation, Writing-review & editing, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
The data presented in this study are available upon request from the corresponding author.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Martina Costanzo ... Ilenia Campione
Zeina Darwich ... Chadi Azmeh
Francesca Gorassini ... Gabriele Cervino
Olha Denefil ... Natalia Tverdokhlib
Gerardo Pellegrino ... Giuseppe Lizio
Alberto Enrique Varela ... José E. Rodríguez
Aiswarya Polumatla ... Tejaswin Polepalle
Aya Dawoud Agha ... Moudar Bakkour
