Urate lowering therapy in primary care: rheum for improvement
Primary care physicians (PCPs) play a critical role in the management of gout worldwide. However, significant gaps in gout care persist, underscoring the need for improved approaches to its manageme
[...] Read more.
Primary care physicians (PCPs) play a critical role in the management of gout worldwide. However, significant gaps in gout care persist, underscoring the need for improved approaches to its management. While some guidelines, such as those from the American College of Physicians (ACP) published in 2016, support a more reactive treat-to-symptoms approach, others from the American College of Rheumatology (ACR) and the European Alliance Of Associations For Rheumatology advocate for a proactive treat-to-target (TTT) strategy—focused on achieving optimal serum urate levels through urate lowering therapy (ULT). This divergence reflects differing clinical priorities and differential interpretation of the evidence and it may contribute to variability in care delivery. Improving gout management requires greater engagement from both patients and healthcare providers, with particular emphasis on increasing adherence to ULT. Patients need enhanced support to better understand the importance of sustained urate lowering treatment, while healthcare providers may benefit from clearer guidance aligned with evidence-based strategies to foster greater patient trust and confidence. This article provides an overview of the current state of guidelines, highlights areas of agreement and discordance between them, and identifies key areas for improving care delivery. It additionally offers insight into alternative care delivery strategies, such as those involving non-physician health professionals, which have shown promise in enhancing patient outcomes. Future research should focus on continued development of innovative, multi-modal interventions to improve ULT adherence, including health system-based initiatives and collaborative care models.
Emilie Schurenberg ... Kenneth G. Saag
View:98
Download:4
Times Cited: 0
Primary care physicians (PCPs) play a critical role in the management of gout worldwide. However, significant gaps in gout care persist, underscoring the need for improved approaches to its management. While some guidelines, such as those from the American College of Physicians (ACP) published in 2016, support a more reactive treat-to-symptoms approach, others from the American College of Rheumatology (ACR) and the European Alliance Of Associations For Rheumatology advocate for a proactive treat-to-target (TTT) strategy—focused on achieving optimal serum urate levels through urate lowering therapy (ULT). This divergence reflects differing clinical priorities and differential interpretation of the evidence and it may contribute to variability in care delivery. Improving gout management requires greater engagement from both patients and healthcare providers, with particular emphasis on increasing adherence to ULT. Patients need enhanced support to better understand the importance of sustained urate lowering treatment, while healthcare providers may benefit from clearer guidance aligned with evidence-based strategies to foster greater patient trust and confidence. This article provides an overview of the current state of guidelines, highlights areas of agreement and discordance between them, and identifies key areas for improving care delivery. It additionally offers insight into alternative care delivery strategies, such as those involving non-physician health professionals, which have shown promise in enhancing patient outcomes. Future research should focus on continued development of innovative, multi-modal interventions to improve ULT adherence, including health system-based initiatives and collaborative care models.
 The prevalence and risk factors of gouty arthritis among fishermen in the Niger Delta region of NigeriaOpen AccessOriginal ArticleAim: This study aimed to explore the prevalence and risk factors of gout among fishermen in the Niger Delta. Methods: A total of 300 fishermen, aged 25–65 years, were recruited through st [...] Read more.Gogo James Owo ... Enyohwo Dennis KpomahPublished: March 25, 2025 Explor Musculoskeletal Dis. 2025;3:100789
The prevalence and risk factors of gouty arthritis among fishermen in the Niger Delta region of NigeriaOpen AccessOriginal ArticleAim: This study aimed to explore the prevalence and risk factors of gout among fishermen in the Niger Delta. Methods: A total of 300 fishermen, aged 25–65 years, were recruited through st [...] Read more.Gogo James Owo ... Enyohwo Dennis KpomahPublished: March 25, 2025 Explor Musculoskeletal Dis. 2025;3:100789 Urate lowering therapy in primary care: rheum for improvementOpen AccessReviewPrimary care physicians (PCPs) play a critical role in the management of gout worldwide. However, significant gaps in gout care persist, underscoring the need for improved approaches to its manageme [...] Read more.Emilie Schurenberg ... Kenneth G. SaagPublished: March 25, 2025 Explor Musculoskeletal Dis. 2025;3:100788
Urate lowering therapy in primary care: rheum for improvementOpen AccessReviewPrimary care physicians (PCPs) play a critical role in the management of gout worldwide. However, significant gaps in gout care persist, underscoring the need for improved approaches to its manageme [...] Read more.Emilie Schurenberg ... Kenneth G. SaagPublished: March 25, 2025 Explor Musculoskeletal Dis. 2025;3:100788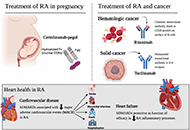 Highly effective treatment options for rheumatoid arthritis afforded by the availability of biosimilarsOpen AccessCommentaryBiosimilars are biologic products that provide equal mechanisms and efficacy to that of their original biologic references. This paper aims to provide a comprehensive overview of the numerous ways b [...] Read more.Leticia A. Shea, Jamshaid S. AhmedPublished: March 03, 2025 Explor Musculoskeletal Dis. 2025;3:100787
Highly effective treatment options for rheumatoid arthritis afforded by the availability of biosimilarsOpen AccessCommentaryBiosimilars are biologic products that provide equal mechanisms and efficacy to that of their original biologic references. This paper aims to provide a comprehensive overview of the numerous ways b [...] Read more.Leticia A. Shea, Jamshaid S. AhmedPublished: March 03, 2025 Explor Musculoskeletal Dis. 2025;3:100787 Re-conceptualizing structural damage in chronic calcium pyrophosphate crystal inflammatory arthritis through ultrasonography: a pictorial essayOpen AccessCommentaryCalcium pyrophosphate deposition (CPPD) disease is the most prevalent crystal related arthropathy in the older-aged population. The clinical spectrum of CPPD arthropathy can include asymptomatic, ac [...] Read more.Janeth Yinh ... Ali GuermaziPublished: February 24, 2025 Explor Musculoskeletal Dis. 2025;3:100786
Re-conceptualizing structural damage in chronic calcium pyrophosphate crystal inflammatory arthritis through ultrasonography: a pictorial essayOpen AccessCommentaryCalcium pyrophosphate deposition (CPPD) disease is the most prevalent crystal related arthropathy in the older-aged population. The clinical spectrum of CPPD arthropathy can include asymptomatic, ac [...] Read more.Janeth Yinh ... Ali GuermaziPublished: February 24, 2025 Explor Musculoskeletal Dis. 2025;3:100786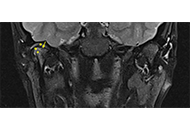 Perspective on clinical and imaging tools for early identification of temporomandibular joint involvement in juvenile idiopathic arthritisOpen AccessPerspectiveThe temporomandibular joint (TMJ) involvement is an underestimated feature of juvenile idiopathic arthritis (JIA) since it is usually asymptomatic at presentation for an undeterminable time. Late di [...] Read more.Silvia Magni-ManzoniPublished: February 11, 2025 Explor Musculoskeletal Dis. 2025;3:100785
Perspective on clinical and imaging tools for early identification of temporomandibular joint involvement in juvenile idiopathic arthritisOpen AccessPerspectiveThe temporomandibular joint (TMJ) involvement is an underestimated feature of juvenile idiopathic arthritis (JIA) since it is usually asymptomatic at presentation for an undeterminable time. Late di [...] Read more.Silvia Magni-ManzoniPublished: February 11, 2025 Explor Musculoskeletal Dis. 2025;3:100785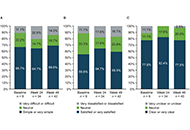 Transition from reference adalimumab to biosimilar SB5 in patients with rheumatoid arthritis: sub-analysis of Spanish patients in the PROPER studyOpen AccessShort CommunicationThis sub-analysis of the PROPER study aimed to evaluate outcomes following the transition from reference adalimumab (ADL) to SB5 (Imraldi™) in routine clinical practice in Spanish patients with rh [...] Read more.Fernando Pérez-Ruiz ... Eugenio Chamizo CarmonaPublished: February 10, 2025 Explor Musculoskeletal Dis. 2025;3:100784
Transition from reference adalimumab to biosimilar SB5 in patients with rheumatoid arthritis: sub-analysis of Spanish patients in the PROPER studyOpen AccessShort CommunicationThis sub-analysis of the PROPER study aimed to evaluate outcomes following the transition from reference adalimumab (ADL) to SB5 (Imraldi™) in routine clinical practice in Spanish patients with rh [...] Read more.Fernando Pérez-Ruiz ... Eugenio Chamizo CarmonaPublished: February 10, 2025 Explor Musculoskeletal Dis. 2025;3:100784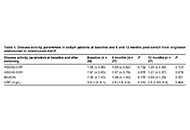 Efficacy of switching from originator adalimumab to biosimilar adalimumab-AACF in patients with axial spondyloarthritis: a 12-month observational studyOpen AccessOriginal ArticleAim: The use of anti-TNF drugs is well-established for treating axial spondyloarthritis (axSpA). The introduction of biosimilars offers a more accessible alternative, but data on the switching of [...] Read more.Fanny Alcira Reyes Neira ... Andrea Yukie ShimabucoPublished: February 10, 2025 Explor Musculoskeletal Dis. 2025;3:100783
Efficacy of switching from originator adalimumab to biosimilar adalimumab-AACF in patients with axial spondyloarthritis: a 12-month observational studyOpen AccessOriginal ArticleAim: The use of anti-TNF drugs is well-established for treating axial spondyloarthritis (axSpA). The introduction of biosimilars offers a more accessible alternative, but data on the switching of [...] Read more.Fanny Alcira Reyes Neira ... Andrea Yukie ShimabucoPublished: February 10, 2025 Explor Musculoskeletal Dis. 2025;3:100783 Optimizing development of anti-TNFα biosimilars based on 10 years’ experienceOpen AccessReviewRoutine regulatory requirements for large comparative efficacy trials (CETs) to support marketing approval of monoclonal antibody (mAb) biosimilars have been the focus of extensive debate in the las [...] Read more.Cecil NickPublished: February 08, 2025 Explor Musculoskeletal Dis. 2025;3:100782
Optimizing development of anti-TNFα biosimilars based on 10 years’ experienceOpen AccessReviewRoutine regulatory requirements for large comparative efficacy trials (CETs) to support marketing approval of monoclonal antibody (mAb) biosimilars have been the focus of extensive debate in the las [...] Read more.Cecil NickPublished: February 08, 2025 Explor Musculoskeletal Dis. 2025;3:100782 Patterns and inequities in pyogenic arthritis-related mortality in the United States from 1999–2020Open AccessShort CommunicationPyogenic arthritis (PA) related mortality trends have not been studied well across various demographics in the United States (US). This cross-sectional study aimed to evaluate these trends among the [...] Read more.Usama Qamar ... Eisha MazharPublished: January 27, 2025 Explor Musculoskeletal Dis. 2025;3:100781
Patterns and inequities in pyogenic arthritis-related mortality in the United States from 1999–2020Open AccessShort CommunicationPyogenic arthritis (PA) related mortality trends have not been studied well across various demographics in the United States (US). This cross-sectional study aimed to evaluate these trends among the [...] Read more.Usama Qamar ... Eisha MazharPublished: January 27, 2025 Explor Musculoskeletal Dis. 2025;3:100781 Chronic pain, fibromyalgia, and long COVIDOpen AccessReviewChronic pain is a common problem in rheumatology. A distinction is made between nociceptive pain and nociplastic pain. Nociceptive pain is, for example, mechanistically explained by persistent infla [...] Read more.Jürgen BraunPublished: January 22, 2025 Explor Musculoskeletal Dis. 2025;3:100780
Chronic pain, fibromyalgia, and long COVIDOpen AccessReviewChronic pain is a common problem in rheumatology. A distinction is made between nociceptive pain and nociplastic pain. Nociceptive pain is, for example, mechanistically explained by persistent infla [...] Read more.Jürgen BraunPublished: January 22, 2025 Explor Musculoskeletal Dis. 2025;3:100780 Musculoskeletal ultrasound in rheumatologic diseasesOpen AccessPerspectiveMusculoskeletal ultrasound has become a valuable imaging tool in the diagnosis and management of rheumatologic disorders. Expertise in recognizing sonographic findings of pathology is the basis for [...] Read more.Antje L Greenfield, Riti Kanesa-ThasanPublished: January 19, 2025 Explor Musculoskeletal Dis. 2025;3:100779
Musculoskeletal ultrasound in rheumatologic diseasesOpen AccessPerspectiveMusculoskeletal ultrasound has become a valuable imaging tool in the diagnosis and management of rheumatologic disorders. Expertise in recognizing sonographic findings of pathology is the basis for [...] Read more.Antje L Greenfield, Riti Kanesa-ThasanPublished: January 19, 2025 Explor Musculoskeletal Dis. 2025;3:100779 Dysbiosis as a common pathogenetic mechanism in psoriasis and gastrointestinal diseasesOpen AccessLetter to the EditorChristos ZavosPublished: January 10, 2025 Explor Musculoskeletal Dis. 2025;3:100778
Dysbiosis as a common pathogenetic mechanism in psoriasis and gastrointestinal diseasesOpen AccessLetter to the EditorChristos ZavosPublished: January 10, 2025 Explor Musculoskeletal Dis. 2025;3:100778