Abstract
Hip ultrasound, according to Graf, is a standardized sonographic method for the detection of developmental dysplasia of the hip (DDH) during the neonatal period. Graf established his method during the 1980s in his home country Austria. It was implemented in the Austrian Mother-Child Health Passport in 1992. Since then it served as a general screening method. The aim of this paper is to present the effects of general hip ultrasound screening in Austria by reviewing and analysing the literature of Austrian authors. This article described how the method was further developed and which prerequisites are currently required for a correct diagnosis. Moreover, it reports about the education in ultrasound screening according to Graf in Austria.
Keywords
Developmental dysplasia of the hip, therapy, general screening, Graf method, Austria, effect of general screening, baby hipDevelopmental dysplasia of the hip (DDH) is the most common congenital disorder in new-borns. Untreated, it may result in pain, limping, joint stiffness, and abnormal gait. DDH includes a wide spectrum of conditions ranging from mild acetabular dysplasia to complete dislocation of the femoral head. Breech presentation, female sex, and positive family history are contributing factors [1]. The incidence of DDH varies from 1 per 1,000 live births to as high as 76 per 1,000 depending on the definition used as well as on the region and population considered [2].
The overall treatment goal for DDH is to achieve and maintain a concentric and stable reduction of the femoral head in the acetabulum as early as possible. For a diagnosis of DDH in the neonatal period, sonography is considered the most reliable method [3, 4]. An early diagnosis of DDH by ultrasound allows the earliest possible treatment, which facilitates the conversion of a dysplastic hip to a normal hip in almost all cases, usually possible by nonoperative methods [5].
The foundation of ultrasound examinations is the piezo-electric effect which was detected in 1880 by Jacques and Pierre. In medicine, ultrasound was primarily used by Dussik in 1938 for the examination of brain ventricles [6]. In 1980, a group of Austrian orthopedics, radiologists, and technicians led by Reinhard Graf from Stolzalpe, Styria, researched ultrasound techniques for the infant hip. The group established an examination technique of high diagnostic value. Graf’s technique offers a quick and effective method for the detection of DDH in babies and was soon considered the gold standard [7–9]. In their research, the group set up the parameters for neonatal hip ultrasound. Additionally, they improved and standardized the examination over time. Therefore, they advised using the examination cradle and the probe holder in further studies (Figure 1) [10, 11]. Moreover, the research group determined the standard plane, investigated hip maturation, and determined the differences between an immature and a pathologic neonatal hip. They classified different stages of DDH in detail and proposed a consecutive treatment protocol guided by ultrasound. Moreover, they established a standardized examination technique and guidelines for image description. It was proven that a 7.5 MHz linear transducer was best suited for the neonatal hip examination. The optimum conditions for the ultrasound intensity, the depth compensation, and the contrasts were determined. More intensity is required the deeper the structure is. Medium depth compensation as well as medium contrasts are required.
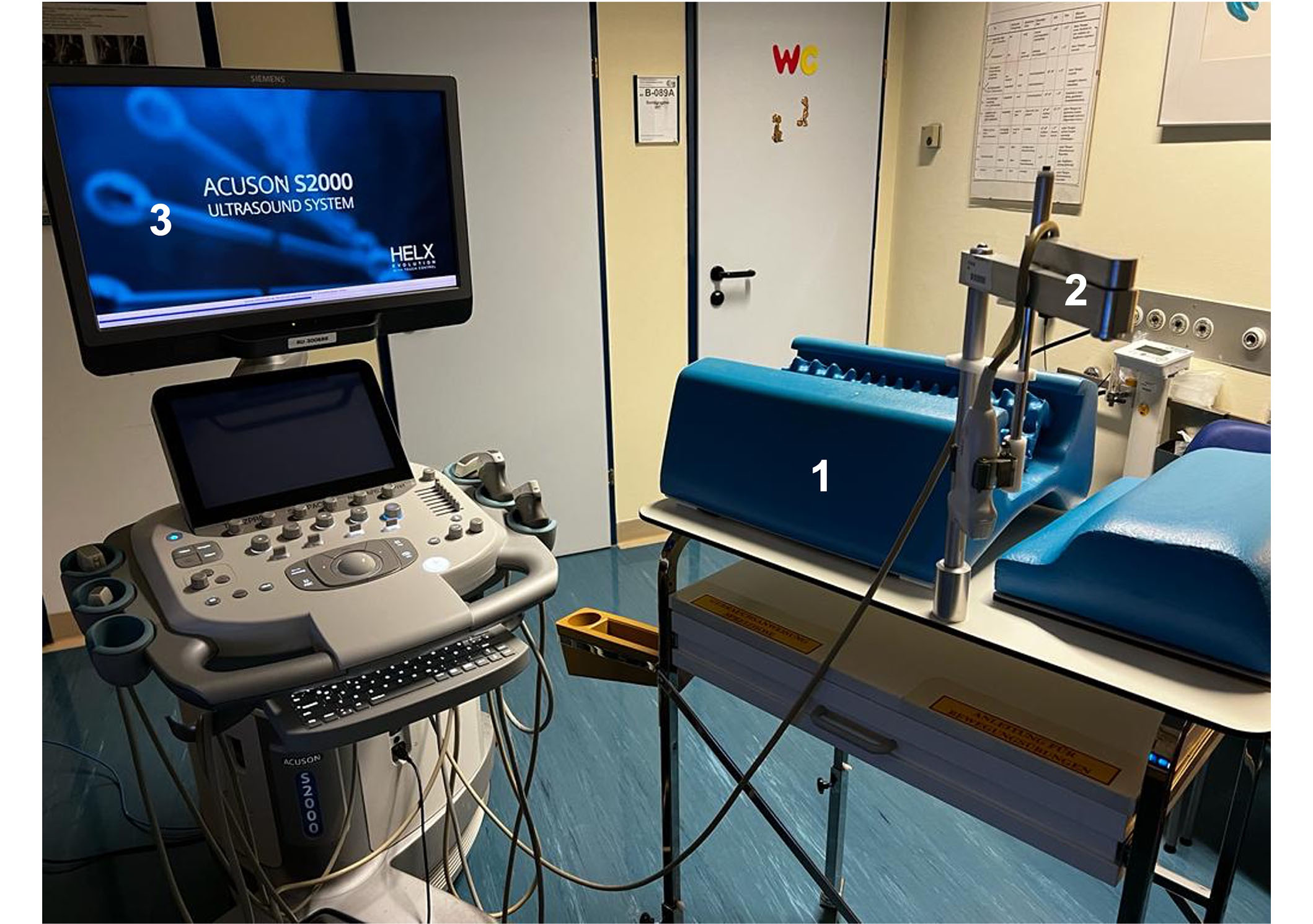
Recommended setting for ultrasound of baby hips. The use of the examination cradle (1) for positioning the baby correctly and the probe holder (2) to fix and position the transducer for every scan is strongly recommended. Position of the ultrasound maschine (3)
The research group established that the best projection for the image is the right coronal position (same as imaging the right hip by a hip X-ray, Figure 2A). The right coronal view offers a better understanding of the anatomy (or the pathology) of the hip joint, thus further standardizing the diagnostic procedure. The image needs to be labelled [right or left side, name of the patient, date of examination, name of examiner or institution, (Figure 2A–C)], and checklist 1 and checklist 2 (Table 1) must be filled out [12]. Rules for magnification were also presented and standardized to ensure the quality of reporting. Therefore, the hip joint should occupy at least two-thirds of the image, extend cranially up to a few millimeters above the proximal perichondrium and clearly demonstrate the chondro-osseous border [12]. Graf’s method soon became a nationwide standard in Austria for screening neonatal DDH. Additionally, it has been accepted by healthcare systems in several states in Central Europe and has rapidly spread to other European and non-European countries (Graf 2006, Graf 2010, Graf 2014). Graf’s ultrasound examination is easy to perform, allows a dynamic examination of the hip and represents all the different hip types in detail (Table 2). It is known as a standardized method with high reproducibility and good interrater reliability [13–15].
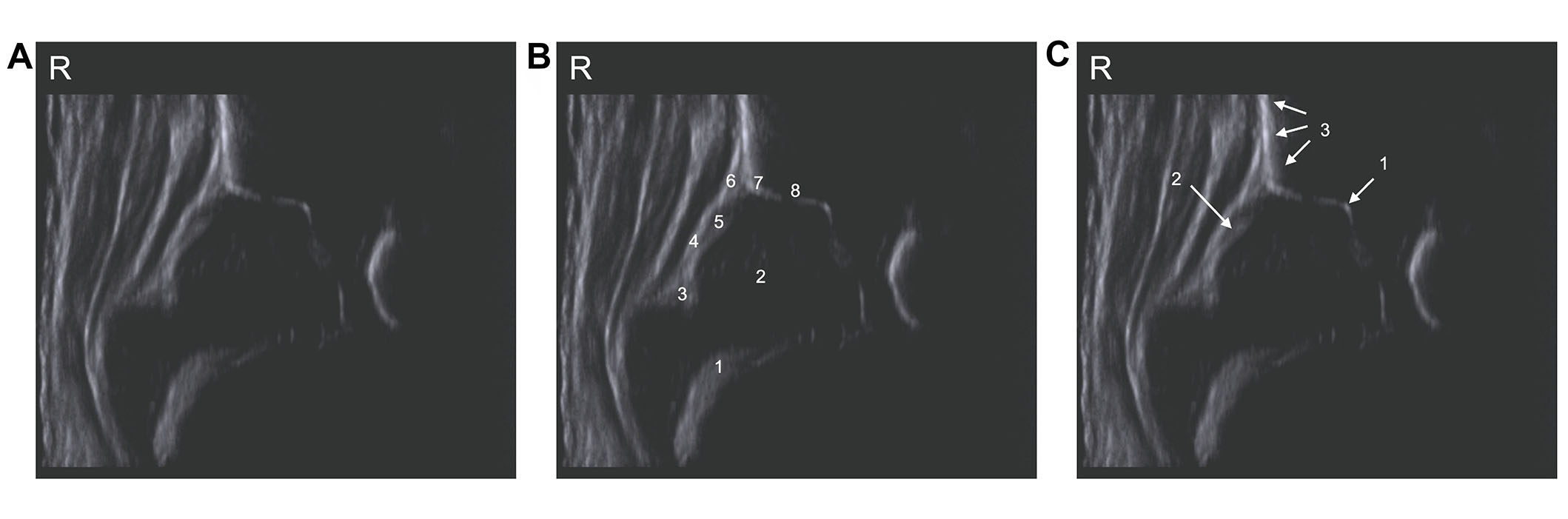
Hip ultrasound in the standard plane. To validate this, all anatomical landmarks have to be identified (see Figure 2B), also a usability test has to be performed (see Figure 2C). (A) Sonogram of a healthy hip; (B) anatomical structures: chondro-osseous border (1), femoral head (2), synovial fold (3), joint capsule (4), labrum acetabulare (5), cartilagineous roof (6), bony roof (7), bony rim (concavity-convexity, 8); (C) landmarks for utility check: lower limb of the os ilium (1), labrum (2), straight silhouette of the os ilim (3)
Checklists to confirm the standard plane
| Checklist 1: anatomical identification | Checklist 2: usability check |
|---|---|
|
|
The different hip types according to Graf [16]
| Graf-type | Age | Bony roof α angle | Bony rim | Cartilaginous roof β angle |
|---|---|---|---|---|
| I: mature hip | Every age | Good, α ≥ 60° | Angular/Blunt | Covering femoral head, β < 55° |
| IIa: physiological immature, age-appropriate | < 12 weeks | Sufficient, α = 50°–59° | Round | Covering femoral head |
| IIa+: physiological immature, age-appropriate | > 6 weeks | |||
| IIa-: physiological immature, maturation deficit | > 6 weeks | Inadequate, α = 50°–59° | ||
| IIb: delay in bony maturation | > 12 weeks | |||
| IIc: critical hip | Every age | Highly insufficient, α = 43°–49° | Round to flattened | Covering femoral head, stable, β < 77° |
| D: hip with beginning decentration | Displaced, β > 77° | |||
| III: decentred hip | Bad, α < 43° | Flattened | Pressed upwards | |
| IV: decentred hip | Pressed downwards |
In Table 2 the different hip types according to Graf are presented. There is a detailed morphology description for the bony and the cartilaginous roof. The Graf classification shows the different forms of DDH in detail with respect to the age and physiological maturity of the neonatal hip.
Austria was the first country that implemented the hip ultrasound examination for the detection of DDH in the “Mother-Child Health Passport” in 1992. This health passport provides health care for pregnant women and their children and includes five medical examinations during pregnancy and five medical examinations of the child after birth [17]. The Mother-Child Health Passport examinations are free of charge for both, the mother and the child. They are covered by the Austrian health insurance providers. In Austria, every citizen is insured for health care.
Parents receive a financial allowance for their children from health insurance. To ensure that the Mother-Child Health Passport examinations are executed, the amount of the childcare allowance is connected to the correct timing of the Mother-Child Health Passport examinations. For every examination, the parents receive a stamp, and the performed examination has to be reported health insurance provider. Therefore, early detection of hip dysplasia and hip dislocation is assured in Austria. The ultrasound examination is performed twice: first, within the first week of life when the child usually is still in hospital with the mother. The second examination takes place between the 6th and 8th week of life during a further required Mother-Child Health Passport examination.
In Austria, the general screening is performed by medical doctors—mainly pediatricians, but also orthopedic surgeons. All of them are specially trained. In case of doubt or if the child requires therapy, it is referred to an orthopedic center. Here, a specially trained pediatric orthopedic surgeon confirms the diagnosis and begins the therapy.
The introduction of a universal screening in Austria soon showed effects. In 1997, Grill et al. [18] published that the rate of open surgery for DDH was significantly reduced by 50% (percentage of clinic patients with the diagnosis DDH: 1992: 8.37%; 1994: 5.56%; open reduction 1992: 0.35%; 1994: 0.24%) and costs for hospital stays due to DDH treatment decreased significantly.
Thallinger et al. [19] confirmed the finding in Austrian nationwide study in 2014. With the introduction of the general screening, the rate of pelvic surgery decreased. Comparing 1992 to 2008, the number of surgical interventions (acetabuloplasty, pelvic osteotomy, triple osteotomy, periacetabular osteotomy) declined from 1.3 per 1,000 to 0.7 per 1,000—a reduction of 46%, and the number of open hip reductions decreased from 0.35 per 1,000 live births in 1992 to 0.16 per 1,000 live births in 1995 in the age group below 4 [19].
In 2011, Thaler et al. [20] presented the positive long-term effect of the Austrian universal screening for DDH: he found that costs for the general health care system referring to DDH increased within the first 5 years after the implementation of general screening. However, costs for hospital stays due to DDH treatment were significantly reduced within the next decade and stayed low [20].
In 2018, Biedermann et al. [5] again pointed out the positive effects of universal screening in Austria. There was a significant switch towards early detection of DDH allowing early treatment performed conservatively in almost all cases. Hence, the rate of open reduction and secondary DDH-related surgery later in life was reduced [5].
Although the beneficial results in Austria (also in Germany and other European countries) strongly support the benefits of general screening, Graf’s technique is questioned concerning its reliability and reproducibility in several scientific articles [13, 14, 21, 22]. The main point of criticism is the one of overdiagnosis with overtreatment leading to increased costs for the health care system [23].
In this context, one needs to be aware that several published papers base their arguments on inadequate scans with major technical errors and therefore their conclusion is questionable [8]. As mentioned before, it must be emphasized again that Graf’s ultrasound scanning technique is a strictly standardized method which is thoroughly described by Graf himself [16]. Before the start, technical requirements must be fulfilled (Figure 1) and the technique must be applied accurately to draw the right conclusions. Therefore, certain steps have to be followed in a certain order to produce a diagnostically valuable sonogram [24] (Figure 2). Figure 3A and 3B are examples for wrong sonograms leading to a wrong diagnosis.
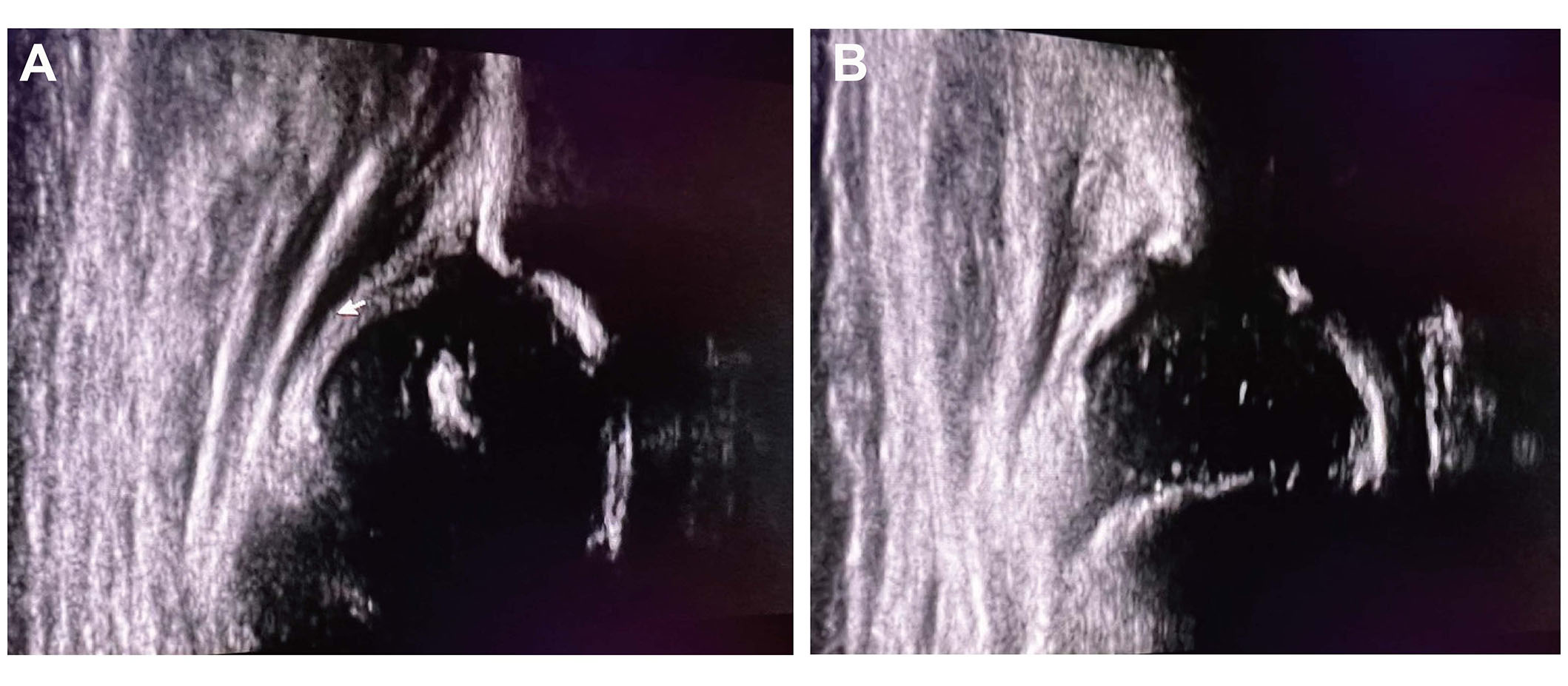
Incorrect sonograms. Not all required anatomical landmarks can be identified, the chondro-osseous border is missing. The usability check is negative. This sonogram presents an anterior tilting error (A). Dorsal tilting error sonogram (B)
Firstly, the baby has to be positioned correctly. Therefore, an examination cradle is required. Moreover, a probe holder to fix and position the transducer is strongly recommended for every scan to avoid tilting errors which result in a wrong diagnosis (Figure 3B). The projection of the image should always be in the right coronal position. Tilting causes a major source of confusion and consecutive errors in the evaluation of a sonogram. Tilting errors stem from the use of the wrong probe type (non-linear probe) or the use of an incorrect scanning technique.
The transducer position is determined by the appearance of anatomical structures (landmarks) and their defined cross-sectional shape on the sonographic images. In 2017, Kolb et al. [25] from the Medical University Vienna investigated the permissible tolerance of the transducer positioning and the resulting effect on the hip measurement respectively the grading system. They found out that notable inclinations of the transducer positions are possible despite a standardized plane defined by Graf’s criteria and the use of a probe holder. Thereby a caudally -nclined transducer position significantly reduces the measured α-angles, whereas a cranially-inclined position significantly increases the measured α-angles. Most importantly, caudal inclination leads to underestimated α-angles, and, in contrast, a combined posterior and cranial transducer inclination may lead to overestimated α-angles with subsequent effects on the classification system [25].
The usability check (checklist 2 in Table 1) confirms that the sonogram is in the “standard plane”, meaning that the sound beam has followed the route, (a) through the (sonographic) center of the acetabulum (lower limb of the osilium), (b) through the middle of the acetabular roof (straight silhouette of the osilium), and (c) through the labrum. Finally, tilting errors due to the wrong examination technique have to be ruled out, before the sonogram may be used for further reporting.
The checklists are followed by a morphological (descriptive) classification. Hereby the hips are categorized into different types according to their morphology. The classification is based on the description of the structures of the acetabulum, the turning point (bony rim), and the cartilaginous roof (hyaline cartilage of the roof of the acetabulum).
All centered hips must fulfill the criteria of the usability check while in decentered hips the lower limb of the osilium can be missing due to the dislocation. Measurements of the α angle and β angle can only be performed after completing checklists 1 and 2 (in Table 1) positively. Only centered hips can be measured.
The Graf method allows to detection of a wide spectrum of DDH by ultrasound and to classification of it in detail. Particularly critical hips (Graf type IIc and D) are detected early, allowing early treatment. Treatment is always ultrasound-guided and the different hip types require different treatments.
To strengthen the training for hip ultrasound according to Graf, the Austrian Society for Orthopedics established a recommendation guideline (Table 3). During residency, 100 ultrasound examinations are recommended. Images and their reports are required.
Hip ultrasond education in Austria
| Suggested requirements for the achievement of an Austrian hip ultrasound diploma |
|---|
| Residency/Resident |
|
| Approval for cost coverage by health insurance (out-patient) |
|
|
| Refresher |
|
The table presents the currently aspired concept for education in hip ultrasound according to Graf. *: person approved by ÖGUM (Austrian Society of Ultrasound) and passed all courses, gives courses, does hip ultrasound regularly (> 3,000 images)
Completion of a basic and advanced course (8 h per course) as well as a final course (8 h) is strongly recommended. The interval between the advanced and final course has to be 6 months. In total 200 hip ultrasounds have to be performed. Every 5 years a refresher course is required.
Hip ultrasound according to Graf is a reliable reproducible method to detect DDH early. It allows to classification of a wide spectrum of DDH in detail and enables ultrasound-guided therapy. The method was refined and critically assessed.
It has been implemented in the Austrian Mother-Child Health Passport since 1992. Since then, the rate of surgical interventions for DDH decreased, and treatment in Austria has shifted towards conservative treatment within the neonatal period, which resulted in positive economic effects for the healthcare system. To guarantee a high-level qualification of examiners, structured education in residency programs and additional educational courses in hip sonography are mandatory.
Abbreviations
| DDH: | developmental dysplasia of the hip |
Declarations
Author contributions
TK and CC: Conceptualization, Visualization, Writing—original draft, Writing—review & editing.
Conflicts of interest
Both authors declare that they have no conflicts of interest.
Ethical approval
According to our local ethical comittee, the article does not require ethical approval.
Consent of participate
Informed consent to participate in the study was obtained from all participants.
Consent to publication
Not applicable.
Availability of data and materials
All data for this study are included in the manuscript.
Funding
Not applicable.
Copyright
© The Author(s) 2024.