Abstract
Aim:
Numerous investigations have revealed sex differences in recovery outcomes in individuals who have sustained work-related musculoskeletal injuries (WRMIs). Previous research has also revealed significant sex differences in the prevalence and severity of post-traumatic stress symptoms (PTSS) following musculoskeletal injury. This study investigated whether PTSS mediated sex differences in recovery outcomes in individuals receiving treatment for a work-related musculoskeletal injury. The recovery outcomes of interest in the present study were pain severity and pain-related disability.
Methods:
The study sample included 137 individuals (68 men; 69 women) with WRMIs who were enrolled in a 7-week physical rehabilitation program. Participants completed measures of pain severity, pain disability and PTSS at admission and termination of the physical rehabilitation program.
Results:
Consistent with previous research, independent samples t-tests revealed that women obtained significantly higher baseline scores on measures of pain severity (P < 0.01), number of pain sites (P < 0.001), depression (P < 0.001) and PTSS (P < 0.001) compared to men. Also consistent with previous research, the measure of PTSS, assessed at baseline, was prospectively associated with treatment-related disability reduction (P < 0.01), and return to work (P < 0.01). Bootstrap regression analyses revealed that PTSS partially mediated the relation between sex and pain-related disability.
Conclusions:
The results of the present study suggest that the experience of PTSS might be one of the factors that explain sex differences in recovery outcomes following a WRMI. The results call for greater attention to the assessment and intervention of PTSS in individuals who have sustained WRMIs.
Keywords
Musculoskeletal injury, pain, disability, post-traumatic stress symptoms, sex differencesIntroduction
Work-related musculoskeletal disorders (WRMDs) are a major cause of disability worldwide [1, 2]. WRMDs involving the spine are considered one of the prevalent and costly non-malignant health conditions affecting the working-age population [1, 3, 4]. In Quebec, work-related musculoskeletal injuries (WRMIs) account for approximately 50% of all time-loss claims [5]. Although, the majority of individuals who sustain a WRMI recover without complication, many will remain work-disabled for prolonged periods of time [6–8]. Of interest in this area of research has been to identify the factors or variables that distinguish between injured workers who will recover and those who will remain occupationally disabled.
Numerous studies have reported significant sex differences in recovery outcomes in individuals who have sustained disabling injuries [9–11]. Recent investigations have reported that women with WRMIs have a significantly longer duration of work absences than men with WRMIs [12]. Research has also indicated that women, compared to men, are more likely to experience multisite pain following musculoskeletal injury and show slower recovery than men from musculoskeletal injuries [13]. Keogh et al. [14] reported that women showed less clinical improvement than men following participation in a multidisciplinary pain management program. Additionally, women were less likely than men to maintain treatment gains when re-assessed at 3-month follow-up. Several investigations have reported that women show less physical improvement than men following participation in rehabilitation interventions for musculoskeletal injuries, and are less likely than men to return to work (RTW) [9, 10].
Research has also revealed significant sex differences in post-traumatic stress symptoms (PTSS) following exposure to traumatic events. The term PTSS is used to refer to the presence of symptoms of post-traumatic stress disorder (PTSD) that do not meet all diagnostic criteria for PTSD [15]. In response to a wide range of traumatic events, women have been shown to be more susceptible to developing PTSS/PTSD than men, with the prevalence of PTSD being twice as high in women compared to men [16, 17]. Though odds ratios vary, sex differences in PTSD prevalence rates have been shown to be robust across differences in trauma type, diagnostic criteria, and study methodology [18].
Recent research points to higher rates of PTSS in women in response to workplace stresses and/or injury. Workplace exposure to trauma can occur in the context of high stress occupations such as health care workers, first responders, or military members. Research suggests that across several high stress occupations, the prevalence and severity of PTSS is higher in women than in men [19]. For example, in a sample of health care professionals in emergency departments, Carmassi et al. [20] observed significantly higher levels of PTSS in women than in men. In a recent study, Pavilanis et al. [21] reported that women scored higher than men on a measure of PTSS following a workplace musculoskeletal injury.
It is possible that PTSS may act as a mediator of sex differences in recovery outcomes following musculoskeletal injury. In light of the research showing that PTSS are more prevalent in women following workplace injury, PTSS might add to the burden of musculoskeletal injury, and in turn, impact negatively of recovery potential [22]. Research examining the processes underlying sex differences in recovery outcomes might help identify key targets for psychosocial interventions designed to improve recovery trajectories following work injury.
The primary objective of the present study was to examine whether PTSS mediate sex differences in recovery outcomes in individuals receiving treatment for WRMIs. Participants completed measures of pain, disability and PTSS at admission to a physical therapy intervention. Pain and disability were re-assessed at treatment termination and RTW was assessed 12-months following treatment termination.
Materials and methods
Participants
The study sample included 137 individuals (68 men; 69 women) who were referred to 1 of 8 primary care physiotherapy clinics in the Greater Montreal region for the treatment of a WRMI, between September 2016 and December 2018. All participants were currently absent from work and had been employed full time prior to the current period of sick leave. Selection criteria included: musculoskeletal injury (i.e., sprain, strain, tear) to the lower back, currently absent from work, and receiving salary indemnity benefits from the provincial work injury insurer. Individuals with complex injuries involving fracture, closed head injury, laceration, or organ damage were not considered for participation.
Measures
Demographic and injury-related information
Participants were asked to provide information about their age, marital status, education, employment, injury site, duration of work disability, and other concurrent treatment they were receiving. Sex was assessed by asking participants to identify as male or female.
Pain severity
Participants rated their current pain severity using an 11-point numerical rating scale (NRS) with the endpoints (0) no pain and (10) excruciating pain. The reliability and validity of NRS pain scales has been demonstrated in previous research [23]. The number of pain sites was used as an index of injury severity and was calculated as the number of areas on a body drawing where participants indicated experiencing pain.
Post-traumatic stress symptoms
The Impact of Events Scale-Revised (IES-R) was used to assess symptoms of PTSS. On this scale, respondents rate the degree to which they are bothered by a range of challenges associated with exposure to a stressful or traumatic event. Ratings are made on a 5-point scale with the endpoints (0) not at all and (4) extremely. Research supports the use of the IES-R as a reliable and valid index of PTSS [24, 25]. Scores on the IES-R discriminate between individuals with and without a diagnosis of PTSD [26]. A cut score of 33 has been recommended as the cut-score for clinically significant PTSS [27]. Cronbach’s alpha for the IES-R in the current sample was 0.95.
Depressive symptoms
The Patient Health Questionnaire-9 (PHQ-9) was used to assess the severity of depressive symptoms. On this scale, respondents indicate how frequently they experience each of 9 symptoms of depression. Ratings are made on a 4-point frequency scale with the endpoints (0) not at all and (3) everyday. Research supports the reliability and validity of the PHQ-9 as a measure of depressive symptom severity [28, 29]. Cronbach’s alpha for the PHQ-9 in the current sample was 0.90.
Self-reported disability
The Pain Disability Index (PDI) [30] was used as a self-report measure of disability. On this scale, respondents rate their current level of pain-related disability in 7 different areas of daily living (home, social, recreational, occupational, sexual, self-care, and life support). Disability ratings are made on an 11-point scale with the endpoints (0) no disability and (10) total disability. Research has supported the reliability and validity of the PDI, as a measure of disability associated with musculoskeletal condition [31]. Cronbach’s alpha for the PDI in the current sample was 0.81.
Return to work
Participants were contacted 12 months following enrolment in the study to respond to interview questions about their RTW status. Interview questions addressed whether participants had returned to full-time, part-time, or transitional work, or whether they remained absent from work.
Procedure
The Institutional Review Board of McGill University approved the study protocol. Participants were recruited through advertisements placed in the waiting rooms of the physical therapy clinics where they were receiving treatment. A telephone screening interview was used to screen participants on inclusion criteria for the study. Participants provided informed consent to enroll in the study. Reporting of the study protocol and findings followed the “Strengthening the Reporting of Observational studies in Epidemiology” (STROBE) guidelines for observational studies [32].
The physical therapy intervention was consistent with clinical practice guidelines for rehabilitation following a musculoskeletal injury emphasizing early mobilization and progressive strengthening exercises [33]. Participants completed self-report measures of pain severity, disability, and PTSS at the time of admission to the physical therapy intervention (T1). Pain and disability were re-assessed at week 4 of treatment (T2) and at week 7 (termination) of treatment (T3). RTW was assessed by telephone interview 12-months following treatment termination. Participants were compensated $25 for completing the self-report questionnaires and $25 for participating in the follow-up interview.
Data analytic approach
Data analyses were conducted with SPSS version 27.0. Initial analyses examined whether study variables varied as a function of the clinics (i.e., recruitment sites) from which participants were recruited. None of the study variables differed significantly as a function of recruitment clinic. As such, recruitment site is not included as a variable in further analyses.
T-tests were used to analyze sex differences on baseline continuous variables (i.e., time since injury, pain severity, number of pain sites, depression, PTSS, and disability). Chi-square (χ2) analyses were used to analyze sex differences on categorical variables (i.e., marital status, education, occupation, and RTW). Mixed (sex × time) Analyses of Variance (ANOVA) were used to analyze treatment-related changes in pain severity and disability. Pearson correlations were used to assess correlates of PTSS.
A bootstrapping procedure described by Preacher and Hayes [34] was used to assess the mediating role of PTSS on the relation between sex and recovery outcomes. In these analyses, the predictor variable (sex) and the mediating variable (PTSS) were assessed at admission (T1); the outcome variables (pain severity, disability) were assessed at termination of treatment (T3); RTW was assessed at 1-year follow-up. Each mediation analysis controlled for known correlates of response to physical rehabilitation interventions including age, education, the number of weeks since injury, and depression [8, 35, 36]. Mediation analyses were conducted using the SPSS macro (PROCESS) [34, 37]. PROCESS uses bootstrapping to test mediation (i.e., indirect) effects. Bootstrapping circumvents power deficiencies of normal theory tests introduced by the non-normality in the sampling distribution. In the current study, the bootstrapping procedure was used to produce 95% confidence intervals (95% CI) of the indirect effects obtained with 5,000 bootstrap resamples [37]. In bootstrapping, mediation is supported if 0 is not within the 95% CI of the indirect effect.
Consistent with previous research, it was predicted that women would report more severe pain, PTSS, and more pronounced disability than men at the time of admission to the physical therapy intervention. Also consistent with previous research, it was predicted that women would show a less favorable response to treatment than men, defined in terms of pain reduction, reduced disability, and RTW. Finally, it was predicted that PTSS would mediate the relation between sex and recovery outcomes.
Power analysis was conducted using the guidelines provided by Fritz and MacKinnon [38]. Assuming a medium effect sizes for the relation between sex and PTSS, and the relation between PTSS and recovery outcomes, in a single sample model with 4 covariates (age, education, time since injury, and depression), with n = 137 and alpha set at 0.01, power exceeds 0.80. The assumption of medium effect sizes is supported by the research that has been conducted to date [21, 39].
Results
Sample characteristics
Means, standard deviations and frequency counts on study variables are presented in Table 1. Women and men did not differ significantly with respect to marital status, χ2 = 3.5, P = 0.08, Phi = 0.16, or occupation, χ2 = 4.7, P = 0.45, Phi = 0.18. Women were more educated than men, χ2 = 18.2, P < 0.001, Phi = 0.36. Women and men did not differ significantly with respect to age, t (135) = –1.3, P = 0.20, d = 0.22, weeks since injury, t (135) = 0.95, P = 0.37, d = 0.13, or self-reported disability at the time of admission, t (135) = 0.31, P = 0.75, d = 0.04. At the time of admission (T1), women reported more severe pain, t (135) = 2.1, P < 0.05, d = 0.36, more pain sites, t (135) = 3.6, P < 0.001, d = 0.63, more severe depressive symptoms, t (135) = 5.5, P < 0.001, d = 0.70, and more severe PTSS, t (135) = 4.6, P < 0.001, d = 0.78, than men. The study sample would be characterized as experienced moderate levels of pain and PTSS [23, 27]. Nine participants (6%) were being treated for depression at the time of admission to the physiotherapy program.
Sample characteristics at the time of admission
| Variable | Men (n = 68) | Women (n = 69) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Marital status | |||||
| Single | 26 | 38.2% | 24 | 34.8% | 0.48 |
| Common law | 14 | 20.6% | 18 | 26.1% | |
| Married | 19 | 27.9% | 14 | 20.3% | |
| Separated/Divorced | 8 | 11.8% | 13 | 18.8% | |
| Widow | 1 | 1.5% | 0 | 0.0% | |
| Education | |||||
| Less than high school | 19 | 27.9% | 10 | 14.5% | 0.01 |
| High school | 25 | 36.8% | 11 | 15.9% | |
| Trade school | 14 | 20.6% | 19 | 27.5% | |
| College | 6 | 8.8% | 18 | 26.1% | |
| University | 4 | 5.9% | 11 | 15.9% | |
| Occupation | |||||
| Labour | 33 | 48.5% | 22 | 31.9% | 0.45 |
| Trade | 2 | 2.9% | 4 | 5.8% | |
| Nursing | 16 | 23.5% | 20 | 30.0% | |
| Admin/Clerical | 9 | 13.2% | 12 | 17.3% | |
| Sales | 3 | 4.4% | 6 | 8.7% | |
| Driver | 5 | 7.4% | 5 | 7.2% | |
| Means | SD | Means | SD | ||
| Age (years) | 38.7 | 9.1 | 36.8 | 7.7 | 0.20 |
| Time since injury (weeks) | 7.0 | 2.8 | 7.4 | 3.0 | 0.37 |
| Disability (PDI-T1; 0–70) | 36.3 | 12.0 | 36.8 | 8.6 | 0.75 |
| Pain severity (NRS-T1; 0–10) | 4.8 | 1.7 | 5.4 | 1.6 | 0.05 |
| Number of pain sites-T1 | 2.1 | 1.0 | 2.7 | 0.9 | 0.001 |
| Depression (PHQ-9; 0–27) | 10.7 | 7.1 | 17.1 | 6.3 | 0.001 |
| PTSS (IES-R-T1; 0–88) | 24.2 | 19.8 | 39.8 | 19.8 | 0.001 |
N = 137. PDI: Pain Disability Index; NRS: numerical rating scale; PHQ-9: Patient Health Questionnaire-9; IES-R: Impact of Events Scale-Revised; SD: standard deviation; Admin: administrator
Correlates of PTSS
Scores on the IES-R were significantly correlated with pain severity (r = 0.31, P < 0.01), number of pain sites (r = 0.37, P < 0.01), and depression (r = 0.53, P < 0.01).
Sex differences in recovery outcomes
The relation between sex and recovery outcomes was assessed in relation to treatment-related changes in pain severity, disability and RTW (Table 2). A sex (women, men) × time (T1, T2, T3) mixed ANOVA was conducted on pain severity ratings. As shown in Table 2, the results revealed significant main effects for sex, F (1, 135) = 13.1, P < 0.001, and time, F (2, 270) = 42.3, P < 0.001. The sex × time interaction was not significant, F (2, 264) = 2.3, P = 0.20. Tests of simple effects revealed that women reported more severe pain than men at all three test points, all P < 0.05. Men and women were also compared on the proportion of participants who showed a 30% or greater reduction in pain through the course of treatment. Slightly more men (36%) than women (29%) showed a 30% or greater reduction in pain, however, the difference was not statistically significant, χ2 = 1.6, P = 0.20.
Treatment-related changes in recovery outcomes
| Variable | AdmissionT1 | Mid-treatmentT2 | TerminationT3 | %ChangeT1 – T3 | d |
|---|---|---|---|---|---|
| Means (SD) | Means (SD) | Means (SD) | |||
| Pain (NRS) | |||||
| Women | 5.4 (1.5) | 4.8 (1.4) | 4.3 (2.2) | 20% | 0.58 |
| Men | 4.8 (1.7) | 3.8 (1.9) | 3.1 (2.0) | 35% | 0.91 |
| Total | 5.1 (1.6) | 4.3 (1.7) | 3.8 (2.1) | 25% | 0.69 |
| Disability (PDI) | |||||
| Women | 36.8 (8.6) | 33.6 (8.9) | 29.1 (9.4) | 21% | 0.85 |
| Men | 36.3 (11.9) | 29.6 (11.1) | 22.7 (10.6) | 37% | 1.25 |
| Total | 36.5 (10.3) | 31.6 (10.2) | 25.9 (10.5) | 29% | 1.01 |
N = 137. PDI: Pain Disability Index; NRS: numerical rating scale; SD: standard deviation
A sex (women, men) × time (T1, T2, T3) mixed ANOVA was conducted on self-reported disability. The results revealed significant main effects for sex, F (1, 135) = 5.8, P < 0.01, and time (2, 270) = 106.2, P < 0.001, qualified by a significant sex × time interaction, F (2, 270) = 8.1, P < 0.001. Tests of simple effects revealed that women and men did not differ significantly on self-reported disability at the time of admission, t (135) = 0.31, P = 0.75. Men reported lower levels of disability than women at mid-treatment, t (135) = 2.3, P < 0.05, and termination, t (135) = 3.7, P < 0.001, test points.
Participants who reported having resumed some forms of employment (transitional, part-time or full-time) were classified as having returned to work. A χ2 analysis revealed that women (52%) were less likely than men (72%) to have returned to work when interviewed 12 months following termination of the physical therapy intervention, χ2 = 5.7, P < 0.01, Phi = 0.17.
PTSS as mediator of sex differences in recovery outcomes
Mediational analyses were conducted for treatment-related disability reduction (T1 PDI – T3 PDI) and RTW. Results of the first mediational analysis confirmed the hypothesis that PTSS mediated the relation between sex and treatment-related disability reduction. The total effect for the model was significant (R2 = 0.18, P < 0.001). As shown in Figure 1, sex was significantly associated with PTSS (Path a; β = –8.5, P < 0.01) and PTSS was significantly associated with treatment-related disability reduction (Path b; β = –0.17, P < 0.001). The bias-corrected bootstrap 95% CI for the indirect effect did not include zero (Path c; β = 1.5, 95% CI = 0.18, 3.2), confirming that PTSS mediates the influence of sex on disability reduction. The results indicated that the direct effect of sex on disability reduction remained significant (Path c’; β = 5.4, P < 0.01) when controlling for PTSS, suggesting partial mediation.
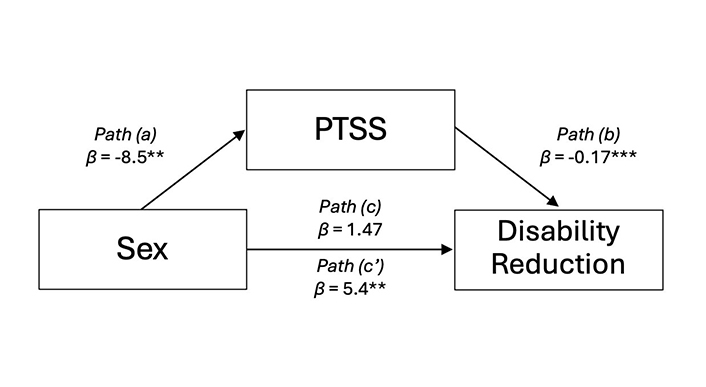
Mediation model of sex on disability reduction by PTSS. Beta (β) coefficients are unstandardized. PTSS: post-traumatic stress symptoms; Sex: sex of participant coded as women (0) men (1); Disability Reduction = PDI (T1) – PDI (T3). ** P < 0.01, *** P < 0.001
The results of the second mediational analysis revealed that PTSS also mediated the relation between sex and RTW. The Nagelkerke pseudo R2 indicated that the final model accounted for approximately 16% of the total variance, P < 0.001. As shown in Figure 2, sex was significantly associated with PTSS (Path a; β = –8.5, P < 0.001) and PTSS was significantly associated with RTW (Path b; β = –0.02, P < 0.01). The bias-corrected bootstrap 95% CI for the indirect effect did not include zero (Path c; β = 0.20, 95% CI = 0.002, 0.50), confirming that PTSS mediates the influence of sex on RTW. The results indicated that the direct effect of sex on RTW was no longer significant (Path c’; β = 0.69, P < 0.12) when controlling for PTSS, suggesting full mediation.
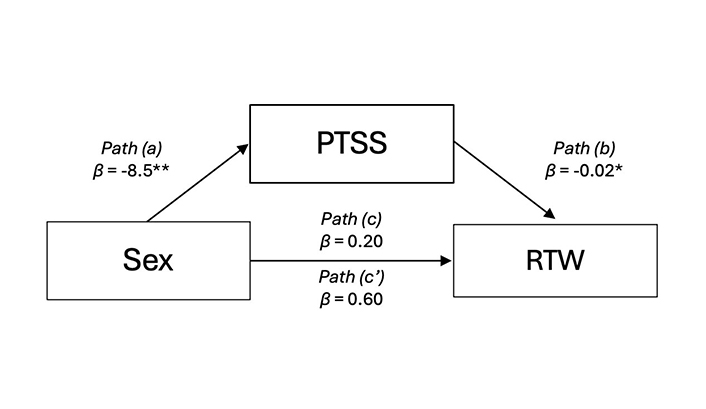
Mediation model of sex on RTW by PTSS. Beta (β) coefficients are unstandardized. PTSS: post-traumatic stress symptoms; Sex: sex of participant coded as women (0) men (1); RTW: return to work. * P < 0.05, ** P < 0.01
Discussion
Study findings were consistent with previous research showing that women report more severe pain than men, show more modest reductions in disability, and are less likely than men to RTW following treatment [14, 21]. Numerous investigations have revealed that women, compared to men, experience more severe pain, more frequent pain, and have a poorer prognosis for recovery [40–43]. Previous research also shows that women make fewer gains than men following participation in rehabilitation interventions and are less likely than men to maintain treatment gains [9, 14, 44]. Significant sex differences in disability outcomes have been reported even when controlling for pain severity and depression [8, 10, 41]. In other words, although women report more severe pain and depression than men following musculoskeletal injury, available research suggests that pain and depression are not the factors that account for sex differences in disability outcomes.
Previous research has also revealed significant sex differences in PTSS following injury or trauma [45, 46]. In a recent longitudinal study of patients admitted to a trauma centre, women were more likely than men to screen positive for PTSD and showed more pronounced long term functional limitations [47]. Pavilanis et al. [21] found that women reported more severe PTSS than men in the weeks immediately following a WRMI. The findings of the present study also showed that women obtained significantly higher scores than men on a measure of PTSS. On the basis of recommended cut-scores for the IES-R, 18% of women, compared to 9% of men in the present study, scored above threshold for clinically significant PTSS. These data suggest that there is a high prevalence of clinically significant PTSS in the early weeks post-injury, particularly in women.
The findings join a growing body of literature suggesting that debilitating injuries or illnesses can give rise to clinically significant levels of PTSS, even though the triggering event might not satisfy DSM-5 Criterion A (defining features of a trauma) for a diagnosis of PTSD [48–50]. In the DSM-5, the “event” criterion for a diagnosis of PTSD is quite broad, encompassing “exposure to actual or threatened death or serious injury” [51]. It is a challenging task to define “actual or threatened serious injury” in objective terms since degree of “threat” is a subjective appraisal. A musculoskeletal injury resulting in pain and limitations sufficient to comprise individuals’ ability to perform their occupational activities could be appraised by many as a serious injury.
Recent studies have yielded findings suggesting that health conditions associated with persistent pain are particularly likely to contribute to elevated levels of PTSS, even though the onset of the conditions would not necessarily be considered “traumatic” [52]. For example, significant relations between pain and PTSS has been reported in several groups including individuals with musculoskeletal pain [48], chronic pain [53, 54], arthritis [55], fibromyalgia [49], cancer [50], and burns [56]. The experience of persistent pain may act as a vulnerability factor for PTSS following occupational injury [57].
Bootstrap mediation analyses were conducted for treatment-related reductions in disability and RTW. Mediation was not assessed for treatment-related reductions in pain severity given that the sex × time interaction for treatment-related changes in pain severity was not significant. Mediation was supported for the role of PTSS in accounting for sex differences in disability reduction and RTW. These results suggest that heightened levels of PTSS in women with WRMIs partially explain sex differences in recovery outcomes following disabling work injury.
Research points to a number of factors that might be implicated in the mediational role of PTSS in the relation between sex and recovery outcomes. As noted earlier, the findings of numerous studies show that women are more likely than men to develop PTSS following exposure to trauma [18]. In the context of occupational injury, women’s smaller physical size and strength might contribute to heightened threat appraisals of the possible negative consequences of physical injury. Women typically score higher than men on psychosocial correlates of PTSS such as catastrophic thinking or fear of re-injury, raising the possibility that these variables might also account for the relation between sex and recovery outcomes [58]. There are also important sex differences in role demands where women are more likely than men to assume a disproportionate share of household and caregiving responsibilities [59, 60]. The prospect of disruption in role functioning might also foster heightened threat appraisals of the consequences of injury. Women have also been shown to be more likely to engage in rumination in stressful situations, which could in turn, heighten susceptibility to the development of PTSS [61].
The results of previous studies suggest that PTSS adds to the burden of disability associated with injury [21, 52, 62]. PTSS can interfere with full participation in family, social, recreational, and occupational activities [21, 63, 64]. Avoidance is a central feature of the experience of PTSS where individuals are motivated to avoid situations or activities that might trigger memories of the trauma [18, 20]. When trauma exposure has occurred in the workplace, the workplace might become a key object of avoidance and contribute to prolonged work absence. It is also possible that elements of PTSS, such as avoidance, might compromise full engagement in physical therapy interventions, and ultimately reducing the benefit the individual might derive from treatment.
Research has accumulated indicating that individuals with musculoskeletal conditions that have co-morbid mental health problems are likely to face a more prolonged and problematic course of recovery [65, 66]. Pain-related musculoskeletal conditions with co-morbid mental health problems are associated with greater health care costs and longer periods of work absence than musculoskeletal conditions without co-morbid mental health problems [65, 67]. Investigators have called for greater attention to assessing current and previous mental health in individuals who have sustained occupational injuries [68].
Screening measures for PTSS are not routinely administered in primary care, particularly in cases of musculoskeletal injury since the context of the injury might not be considered traumatic. Consequently, PTSS following musculoskeletal injury are likely to go undetected and untreated [69]. In light of research findings pointing to the potential mutual maintenance of symptoms of pain and PTSD left untreated, PTSS may persist over extended periods of time, compromising recovery of the WRMI [70, 71].
Screening tools such as the IES-R or PCL-5 might be usefully incorporated into the intake assessment protocols of primary care physical therapy clinics. Early identification of injured workers experiencing elevated PTSS could permit instituting a pathway of care addressing multiple elements of the client’s problem profile. Although several empirically-supported treatments for PTSD have been described in the literature [72, 73], issues related to duration of treatment (e.g., 12 weeks) and timely access (e.g., long waitlists) limit the degree to which they can be usefully integrated within primary care services for WRMIs. As well, third party payors will likely be reluctant to consider referrals for lengthy psychological services for injured workers who do not satisfy all diagnostic criteria for PTSD.
There are recent reports supporting the effectiveness of brief treatments for PTSD using telehealth delivery platforms although these have yet to be tested with injured workers with elevated PTSS [74, 75]. Sullivan et al. [76] reported promising RTW outcomes following participation in a risk-targeted behavioral activation intervention for PTSD. Brief interventions aimed at reducing PTSS that can be easily integrated within the structure of care offered within primary care might be the most viable option for promoting more complete recovery following WRMI.
Several limitations invite caution in the interpretation of the study findings. First, all participants were employed full-time prior to their injury, and all were receiving a salary indemnity from a work-injury insurer. Participants were recruited from a network of primary care physical therapy clinics to which they had been referred by the work injury insurer. These selection criteria necessarily have implications for the generalizability of the study findings. Another limitation was that PTSS was assessed by self-report questionnaire. As a result, the degree to which participants who scored in the clinical range of the IES-R met diagnostic criteria for PTSD remains uncertain. The binary nature of the sex variable used in the present did not permit a more in-depth exploration of how gender identity might have influenced the pattern of findings.
It is not feasible within the limits of one research project to examine an exhaustive list of all variables that might mediate sex differences in recovery outcomes following work injury. It is possible that psychosocial correlates of PTSD/PTSS such as catastrophic thinking [77, 78], fear of injury [13] may also have a mediating influence on the relation between sex and recovery outcomes. Whether the explanatory value of PTSS is independent of the contributions of other potential mediators of the relation between sex and recovery outcomes following work injury remains to be clarified by future research.
The results of the present study suggest that the experience of PTSS might be one of the factors that explains sex differences in recovery outcomes following a WRMI. The findings suggest that PTSS are prevalent in the weeks following a WRMI, particularly in women. The experience of clinically significant PTSS following WRMI might add to the burden of disability, in turn, impeding timely recovery and RTW. The findings suggest that early screening for PTSS and the development of brief interventions aimed at reducing the severity of PTSS should be considered as potential avenues for fostering timely recovery and RTW in injured workers with elevated levels of PTSS.
Abbreviations
| 95% CI: | 95% confidence intervals |
| ANOVA: | Analyses of Variance |
| IES-R: | Impact of Events Scale-Revised |
| NRS: | numerical rating scale |
| PDI: | Pain Disability Index |
| PHQ-9: | Patient Health Questionnaire-9 |
| PTSD: | post-traumatic stress disorder |
| PTSS: | post-traumatic stress symptoms |
| RTW: | return to work |
| WRMIs: | work-related musculoskeletal injuries |
| χ2: | Chi-square |
Declarations
Author contributions
ADSP: Conceptualization, Methodology, Formal analysis, Investigation, Writing—original draft, Writing—review & editing. VV: Conceptualization, Methodology, Writing—original draft, Writing—review & editing. HA: Conceptualization, Methodology, Writing—review & editing. MJLS: Conceptualization, Methodology, Formal analysis, Investigation, Writing—review & editing, Funding acquisition, Resources, Supervision.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the Institutional Review Board of McGill University.
Consent to participate
Informed consent to participate in the study was obtained from all participants.
Consent to publication
Not applicable.
Availability of data and materials
The data are available from the corresponding author upon reasonable request.
Funding
This research was supported by funds from the Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST) [2017-0024] and the Canada Research Chairs (CRC) Program [246330]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Copyright
© The Author(s) 2024.