Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Email: john.hoy.research@gmail.com
ORCID: https://orcid.org/0009-0000-3031-4359
Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Affiliation:
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL 60612-3833, USA
Explor Musculoskeletal Dis. 2024;2:256–263 DOI: https://doi.org/10.37349/emd.2024.00053
Received: February 06, 2024 Accepted: March 25, 2024 Published: July 10, 2024
Academic Editor: Jürgen Braun, Ruhr Universität Bochum, Germany
The article belongs to the special issue Calcium Pyrophosphate Deposition Disease
Aim: The purpose of this study is to evaluate outcomes and radiographic progression of wrist arthritis after four-corner fusion (4CF) in patients with evidence of calcium pyrophosphate deposition disease (CPPD). The insights derived from this study are expected to improve the understanding of 4CF outcomes in the presence of CPPD, guiding clinical decisions, and management strategies.
Methods: 11 patients with prior 4CF and evidence of CPPD were available for prospective follow-up and imaging, with a mean follow-up time of 5 years. Range of motion measurements, radiographs, and outcome data were collected at the follow-up visit and prior data and imaging were reviewed retrospectively. The chronological progression of arthritis was evaluated on standard three-view wrist radiographs using the Larsen scale.
Results: All participants (11/11) deemed their wrist fusion a success, with an average satisfaction score of 8.8 out of 10.73% (8/11) patients were able to return to their original occupation after the procedure. The mean flexion of the affected wrist preoperatively was 43 degrees (SD: ±12 degrees) and 41 degrees (SD: ±7 degrees) at the final follow-up. The mean extension of the affected wrist was 35 degrees (SD: ±8 degrees) preoperatively and 40 degrees (SD: ±12 degrees) at the final follow-up. Radiographic analysis showed that 82% (9/11) of patients displayed progression of arthritis as per the Larsen scale by the final follow-up. All patients that showed radiographic progression had involvement of the radiolunate (RL) articulation, which is classically persevered in non-inflammatory wrist arthritis.
Conclusions: Scaphoid excision with 4CF is a promising surgical option for managing CPPD-related wrist arthritis, offering significant functional improvements, motion preservation, and high patient satisfaction. However, it does not halt radiographic progression of arthritis for the majority of patients at a mean prospective long-term follow-up of 5 years.
Wrist arthritis presents as a potentially debilitating impairment in function, affecting mobility and quality of life [1]. Identification of specific wrist arthritis patterns is critical to understanding the disease mechanism and guides intervention. Most advanced wrist arthritis cases are non-inflammatory in nature and include primary osteoarthritis and post-traumatic arthritis, or follow typical degenerative patterns such as scapholunate advanced collapse (SLAC) or scaphoid non-union advanced collapse (SNAC). Both of the latter conditions disrupt normal kinematics and lead to dorsal intercalated segment instability (DISI), progressing into carpal collapse and midcarpal arthritis [2]. Other less common instances of wrist arthritis, however, are related to an inflammatory disease process, such as crystalline arthropathy, one of which is calcium pyrophosphate (CPP) deposition disease (CPPD) [3]. Unlike typical SLAC or SNAC arthritis, which generally preserves the radiolunate (RL) joint, CPPD generates a chronic and diffuse inflammatory response that characteristically compromises the RL articulation and could accelerate the progression of arthritis over time.
For most patients with disabling pain unresponsive to conservative measures, surgical interventions are considered to either remove diseased bone or promote bony fusion in the carpus to slow or alter the arthritic process. The most common techniques are proximal row carpectomy (PRC), scaphoid excision with four-corner fusion (4CF), total wrist fusion (TWF), and total wrist arthroplasty (TWA) [1]. Based on current literature, both 4CF and PRC appear preferable for uncomplicated cases and demonstrate comparable efficacy in wrist motion preservation [4]. 4CF specifically entails the least native bone excision and is defined as the removal of the scaphoid only, followed by fusion of the capitate, hamate, lunate, and triquetrum. Overall, this approach has been associated with positive long-term functional outcomes and patient satisfaction [5].
The specific implications of wrist CPPD on postoperative outcomes remain under-studied and are an area of current research. We examined the outcomes and radiographic progression of wrist arthritis after 4CF in CPPD patients using a screened cohort of our patients. The insights derived from this study are expected to improve the understanding of 4CF outcomes in the presence of CPPD, guiding clinical decisions and management strategies.
This study received approval from the Institutional Review Board (IRB) before initiation. To identify eligible patients, we conducted a search using Current Procedural Terminology (CPT) codes spanning from January 1, 2011, to November 1, 2021. The included CPT codes were:
25800: arthrodesis, wrist joint (including radiocarpal and/or ulnocarpal fusion); without bone graft.
25805: arthrodesis, wrist joint (including radiocarpal and/or ulnocarpal fusion); with sliding graft.
25820: intercarpal fusion; without bone graft.
25825: intercarpal fusion; with autograft (includes obtaining graft).
Initial 4CF surgeries were performed by one of three fellowship-trained hand surgeons, except in one instance where the initial partial fusion was conducted outside our institution and subsequently required revision at our facility. Patients below 18 years of age were excluded. Patients underwent 4CF to treat disabling pain secondary to wrist arthritis refractory to conservative treatment.
In total, 152 patients who underwent 4CF were identified. Among these, 43 patients displayed radiographic evidence of CPPD in the wrist, as indicated by calcifications in the triangular fibrocartilage complex (TFCC). Eleven of these patients were available for prospective follow-up examination and imaging. Polarized light microscopy showing CPP crystals in synovial fluid aspirated from the affected wrist confirmed diagnosis in these patients.
Demographic information was systematically collected for analysis. For radiographic evaluation, standard three-view (posteroanterior, oblique, and lateral) wrist radiographs were reviewed from the preoperative stages through to the final follow-up visit. A single fellowship-trained hand surgeon (XCS) reviewed the chronological imaging. The severity of the radiographic progression of inflammatory arthropathy was assessed using the Larsen scale, a tool traditionally employed in evaluating conditions such as rheumatoid arthritis [6]. Larsen scale gradings were assigned for radiographs taken preoperatively, postoperatively, at intervals between the operation and final follow-up, and at the final follow-up.
An incision is made on the dorsal aspect of the wrist, working through the floor of the third dorsal compartment. After capsulotomy, the scaphoid is excised, and a high-speed burr is used to prepare the fusion surfaces. A distal radius autograft is obtained through a separate incision, which is impacted into the midcarpal joint between the capitate, lunate, hamate, and triquetrum. Fixation is obtained through pin fixation alone or through compression screw fixation. Pre and postoperative radiographs are seen in Figure 1.
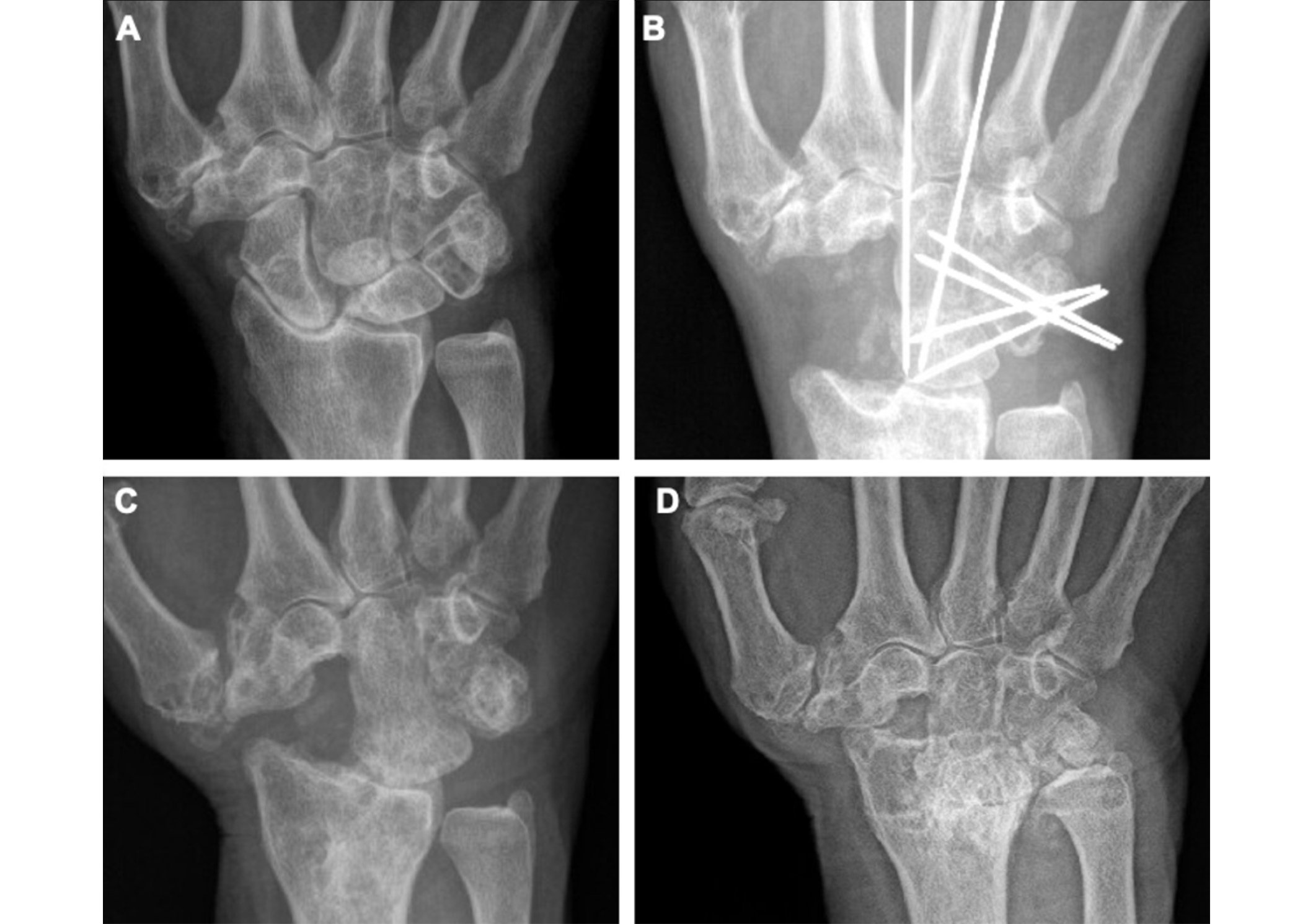
Progression of inflammatory arthritis in included patient 3. (A) Preoperative posterior-anterior (PA) radiograph of affected hand; (B) postoperative PA radiograph of affected hand; (C) PA radiograph of affected hand two years after four-corner fusion (4CF) with scaphoid excision; (D) PA radiograph of affected hand 10 years after 4CF. This figure shows the progression of inflammatory arthritis for one of the included patients in the series
11 patients with radiographic evidence of CPPD and CPP crystals on synovial fluid analysis were available for in-person examinations and imaging. Patients who were not available for in-person examination and imaging were not included in the analysis. The average duration from the index 4CF to the follow-up evaluation and final imaging was 5.09 years (SD: ±2.69 years). The group consisted of ten males and one female, with an average age of 62.7 years (SD: ±7.98 years) at the time of the initial surgery. All patients were right-hand dominant, with eight cases involving the right hand and three involving the left. 18% of patients (2/11) reported being on medications for their inflammatory arthropathy at final follow-up. One patient had a revision 4CF performed at our institution after an initial surgery by an external surgeon. A separate patient had a subsequent flare related to CPPD in the ipsilateral elbow. Clinical information regarding previous flares or CPPD involvement of joints for other patients was not readily available. None of the included patients converted to TWA thereafter.
The range of motion (ROM) analysis revealed that the mean flexion of the affected wrist preoperatively was 43 degrees (SD: ±12 degrees), decreasing to 26 degrees (SD: ±9 degrees) postoperatively. However, at the final follow-up, it improved to 41 degrees (SD: ±7 degrees). The mean extension of the affected wrist was 35 degrees (SD: ±8 degrees) preoperatively, which reduced to 26 degrees (SD: ±10 degrees) postoperatively, and then increased to 40 degrees (SD: ±12 degrees) at the final follow-up (Table 1).
Range of motion for affected wrist
| Interval | Flexion, mean (SD) | Extension, mean (SD) |
|---|---|---|
| Preoperative | 43° (12°) | 35° (8°) |
| Postoperative | 26° (9°) | 26° (10°) |
| Final follow-up | 41° (7°) | 40° (12°) |
In terms of occupational and recreational recovery, 73% (8/11) of patients were able to return to their original occupation after the procedure, while 27% (3/11) were not. For those who resumed work, the average recovery of full work function was 39% at the final follow-up. Regarding recreational activities, the average recovery of function was reported to be 45%.
All participants (11/11) deemed their wrist fusion a success, with an average satisfaction score of 8.8 out of 10. Post-surgery, 36% (4/11) of patients reported a worsening in wrist motion, and 18.2% (2/11) experienced an increase in pain. Regular pain medication for wrist pain was reported by 27.3% (3/11) of patients. Additionally, 36% (4/11) noticed a decrease in wrist strength, and 18.2% (2/11) received cortisone injections post-surgery. The mean Visual Analog Scale (VAS) for pain was 3.7 (SD: ±2.95).
Radiographic analysis showed that 82% (9/11) of patients displayed progression of arthritis as per the Larsen scale by the final follow-up (Table 2). Initially, all patients scored zero on the Larsen scale both preoperatively and immediately postoperatively. At the mid-interval, 64% (7/11) showed signs of progression, with those patients having a mean Larsen score of 1.86 (SD: ±0.69) and an overall mean score of 1.18 (SD: ±1.08). By the final follow-up, the mean Larsen score among patients who showed progression (9/11) was 3.56 (SD: ±1.13), and the overall mean score was 2.91 (SD: ±1.76).
Radiographic progression of arthritis and involvement of the radiolunate (RL) articulation [Larsen scale grading (scale of 1–5)]
| Patient | Preoperative | Postoperative | Middle interval | Final follow-up | Involvement of RL articulation |
|---|---|---|---|---|---|
| 1 | 0 | 0 | 1 | 2 | Y |
| 2 | 0 | 0 | 0 | 0 | N |
| 3 | 0 | 0 | 3 | 5 | Y |
| 4 | 0 | 0 | 0 | 3 | Y |
| 5 | 0 | 0 | 2 | 4 | Y |
| 6 | 0 | 0 | 1 | 2 | Y |
| 7 | 0 | 0 | 2 | 4 | Y |
| 8 | 0 | 0 | 2 | 5 | Y |
| 9 | 0 | 0 | 0 | 3 | Y |
| 10 | 0 | 0 | 2 | 4 | Y |
| 11 | 0 | 0 | 0 | 0 | N |
Preoperative: before index four-corner fusion (4CF); Postoperative: after index 4CF; Middle interval: radiographs closest to halfway between postoperative and final follow-up radiographs. Y: yes; N: no
Our study found: (1) the 4CF procedure is effective for CPPD-related wrist arthritis, with all patients (11/11) reporting satisfaction and 73% (8/11) returning to work; (2) long-term motion-preservation at preoperative ROM despite disease progression; (3) high patient satisfaction despite complications such as pain; but (4) continued radiographic progression of arthritis post-4CF in nearly all patients.
Prior studies have shown 4CF to be a reliable technique, with good long-term outcomes and low rates of conversion to TWF in non-inflammatory wrist arthritis [7]. However, the literature on 4CF in patients with CPPD is sparse.
CPP has been shown to mediate tissue damage by various mechanisms [3]. CPP crystals activate components of the NACHT, LRR, and PYD domains-containing protein 3 (NLRP3) inflammasome, resulting in the production of proinflammatory cytokines [8]. Diffuse chronic inflammation could compromise the quality of the RL articulation and lead to a more rapid deterioration after 4CF. In addition, CPP crystals have direct catabolic effects on chondrocytes and synoviocytes and can deposit into articular cartilage [9–11]. 82% of patients (9/11) in our cohort showed evidence of radiographic progression of arthropathy after 4CF at final follow-up. The pathologic alteration of cartilage, joint mechanics, and inflammation could help explain the accelerated progression of arthritis seen post-4CF.
Motion-preserving treatments for advanced wrist arthritis have become more popular in recent years [12]. This trend towards 4CF and PRC and away from TWA suggests an evolving understanding of the treatments of wrist arthritis. In the context of CPPD, where crystal deposition and inflammation can cause challenges with joint preservation, understanding the relative costs and benefits of treatment modalities can inform how best to manage these complex cases. Heifner et al. [13] recently demonstrated a nearly twofold increase in the risk of disabilities of the arm, shoulder, and hand (DASH) questionnaire score over 30 in patients under 45 years of age who underwent 4CF. CPPD tends to affect older patients, and the mean age in our cohort was 63. Given the evidence that 4CF may be more beneficial for older patients, 4CF may still be a viable option for older CPPD patients despite the accelerated radiographic progression of arthritis demonstrated in our study. PRC is another motion-sparing surgical option for the treatment of advanced wrist arthritis. Gaballah et al. [4] showed lower overall DASH and VAS scores for PRC versus 4CF, but superior grip strength for 4CF compared to PRC. However, after PRC, there is a 4-fold increase in contact pressures in the lunate fossa, as well as a reduction of contact area within the lunate fossa. In addition, there is an increase in the translation of the lunate fossa following PRC, together leading to increased shear forces [14]. These altered mechanics in combination with the pathophysiology of CPPD could theoretically prove to be more detrimental than with 4CF. Further research is needed to determine the optimal surgical management for wrist arthritis for patients with CPPD.
Traverso et al. [15] assessed outcomes for 4CF in patients without inflammatory arthritis with a minimum 10-year follow-up and found that 27% of wrists demonstrated advanced joint space narrowing at the final follow-up. Our cohort had a larger proportion of patients showing advanced arthritis in shorter follow-up times, suggesting accelerated disease progression in CPPD, possibly due to the inflammatory nature of the disease.
Newer studies have utilized patient-reported outcomes to elucidate differences in inflammatory and noninflammatory wrist arthritis for the same surgical intervention. Recently, Chong et al. [16] in their systematic review of 12 studies including 359 patients, found valuable insights for understanding TWA in both inflammatory and non-inflammatory arthritis. They found significant improvements in DASH/Quick-DASH scores post-TWA in both inflammatory and noninflammatory arthritis types. Interestingly, while patient-rated wrist evaluation (PRWE) scores improved in non-inflammatory arthritis, this was not observed in the inflammatory group. They also found that patients with inflammatory arthritis were more than five times more likely to experience complications including stiffness, infection, and implant-related problems [16].
There are a few limitations to our study. First, there was a small sample size of 11 patients available for follow-up and there was no control group of patients who underwent 4CF without evidence of CPPD. Next, conventional radiography detects only 40% of clinically relevant CPPD [17]. It is possible by using only radiographic evidence of CPPD in the wrist to initially screen for CPPD, patients with CPPD without radiographic evidence could be missed. Including synovial fluid analysis to screen patients for CPPD would lead to higher sensitivity to detect CPPD in patients without chondrocalcinosis on radiographs but would be largely impractical. Future research should focus on establishing comprehensive diagnostic protocols that combine advanced imaging and biomarkers for better disease characterization in CPPD patients undergoing 4CF, helping to guide treatment decisions and establish patient expectations following surgery.
Scaphoid excision with 4CF is a promising surgical option for managing CPPD-related wrist arthritis, offering significant functional improvements, motion preservation, and high patient satisfaction. However, it does not halt radiographic progression of arthritis for the majority of patients at a mean prospective long-term follow-up of 5 years.
CPPD: calcium pyrophosphate deposition disease
DASH: disabilities of the arm, shoulder, and hand
PRC: proximal row carpectomy
RL: radiolunate
SLAC: scapholunate advanced collapse
SNAC: scaphoid non-union advanced collapse
TWA: total wrist arthroplasty
JH: Investigation, Data curation, Formal analysis, Writing—original draft. FA: Writing—original draft, Writing—review & editing. MC, RW, and JF: Conceptualization, Investigation, Supervision. XS: Conceptualization, Project administration, Supervision, Investigation, Writing—review & editing.
The authors declare that they have no conflicts of interest.
This study was approval by Rush University Institutional Review Board (22092801).
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Michael Schirmer, Johannes Dominikus Pallua
Anna J. Turlej, Angelo L. Gaffo
Fernando Perez-Ruiz ... Frédéric Lioté
Maria L. Voulgari, Herbert Kellner
Gamze Dilek ... Kemal Nas
Ebru Atalar, Hatice Bodur
