Abstract
Congenital fused/blocked vertebrae are an incidental finding in most cases. It remains asymptomatic unless there is a traumatic event or there is an increased biomechanical load which may be attributed to a task that is not typically performed by the individual. Symptomatic cases can present with several musculoskeletal symptoms including neck pain. Physiotherapy management strategies may help patients recover from the mechanical strains on the cervical neuromuscular structures. The present case is of a 21-year-old male engineering student who was referred for physiotherapy, he presented with complaints of neck pain (non-radiating in nature) for a week. The intensity of the pain had been intermittently increasing/decreasing for about a year and there were about 2–3 episodes in a month for approximately one year. He presented with an X-ray that showed C3–C4 cervical vertebrae synostosis (block vertebrae). The patient was managed using pain education and exercises along with ergonomic advice. Patient-reported pain decreased significantly from the initial visit and he was able to sit for a longer duration and had a considerable improvement in function.
Keywords
Neck pain, block vertebra, exercise therapy, hypermobilityIntroduction
Anomalies of vertebrae like a congenital fusion/block are always interesting to locate and evaluate. It is often an incidental finding detected by professionals during a radiologic examination [1]. A block vertebra is asymptomatic until adulthood and sometimes till young adolescence [2]. In literature, cervical spine anomalies such as block vertebrae have been well documented with most common levels found at the second cervical vertebra (C2)–C3 or C5–C6 [2]. The clinical manifestations can vary from simple neck pain or range of motion restriction to muscular weakness of one or both upper limbs and even complex neurological deficits or myelopathy [3].
Block vertebrae can result in hypermobility in adjacent vertebrae and biomechanical stress leading to symptomatic presentations in advanced age [4]. Neck pain as a common complaint is a leading cause of disability. Causes like congenital anomalies with neck pain and musculoskeletal changes should be dealt with caution during conservative as well as surgical management [5]. Clinically, an early diagnosis can help document changes in aging, the progression of degenerative processes, and lifestyle modifications to lead a pain-free life. The purpose of this case report was to highlight the presence of rare block vertebrae and how conservative intervention can bring improvement to the symptoms experienced by the patient.
Case report
A 21 years Asian male engineering student who was referred by an orthopedic specialist presented to the clinic with complaints of neck pain (non-radiating) for almost a week. He described his pain to be gradually increasing in intensity every time he sat on a chair and studied. The intensity of the pain had been intermittently increasing/decreasing for about a year and about 2–3 episodes in a month for approximately one year after he participated in a sports event. He presented with an X-ray cervical spine prescribed by the orthopedic surgeon which showed C3–C4 block vertebrae. Earlier, he had consulted a health care provider who had advised him non-steroidal anti-inflammatory drugs (NSAIDs) and rest before being referred to physiotherapy.
The patient was quite definite about the factors which increased his pain, studying on a chair for a prolonged duration and lying with a pillow. His numeric pain rating scale (NPRS) level ranged from 5 (minimum) at rest and 8 (maximum) post activity. He emphasized the inability to sit and study as his examinations were near and were anxious about the same. The most painful position was sitting for a prolonged duration followed by supine lying with a pillow, though a no pillow position helped. There were no red flags identified. For the assessment of the patient, both psychosocial factors as well as physical factors causing pain were identified. On physical examination, his cervical spine range of motion was restricted and painful. Left rotation was limited to 45 degrees and flexion/extension was equally painful and restricted. He had tenderness over spinous processes of C3, C4, and C5 vertebrae and gross tenderness over cervical facet joints, upper trapezius, and cervical flexors. Muscle weakness of deep neck flexors was assumed because of the theoretical concept and chronicity of the pain. On assessing the psychosocial factors, he was anxious and worried about the upcoming examinations as he was not able to focus on his studies. He was also concerned about his performance in the examination. He had a sedentary lifestyle and mainly focused on his studies. The international classification of functioning disability and health (ICF) health domains are described in Figure 1 for the patient.
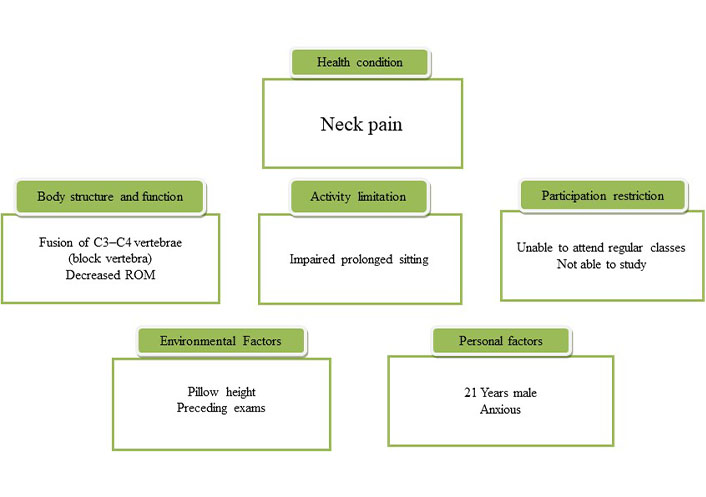
Description of international classification of functioning and disability health domains as per the assessment of the patient. ROM: range of motion
For diagnosis, physiotherapist must try to classify the case either into a pathoanatomic or impairment based. The case was referred by an orthopedic surgeon with a noted diagnosis of non-radiating neck pain. Based on X-ray findings, diagnosis of the patient was considered as a symptomatic block vertebrae. There was fusion at the level of C3/C4 vertebrae. The anteroposterior, lateral views of radiographs are depicted in Figure 2. The aim of the physiotherapists diagnostic process should be to find the divergence that exists between the level of function that is desired by any individual and the capacity of the individual to achieve that level. The patient demonstrated reduced functional capacity and muscle performance. Acknowledgment of pathoanatomical diagnosis and its interpretation into modifying the lifestyle of an individual (if applicable) is a must.
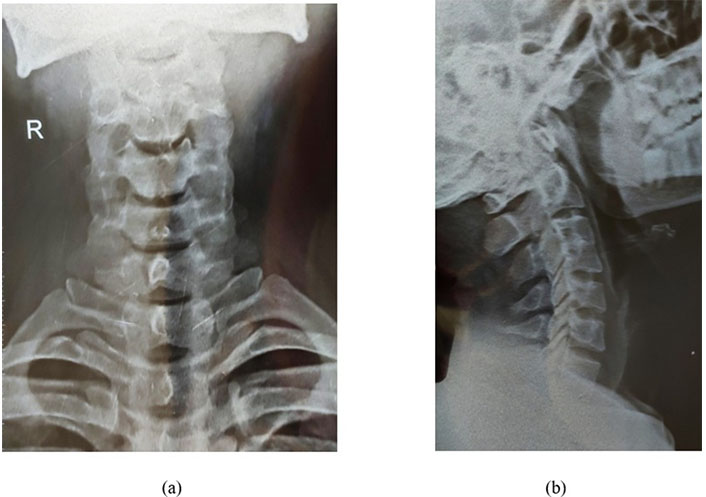
Anteroposterior, lateral views of radiographs showing C3–C4 block vertebrae. (a) Anteroposterior view; (b) lateral view. R: right side of patient
Therapeutic intervention
The patient was treated according to impairments and functions which were most affected irrespective of the congenital anomaly present. Since there were only musculoskeletal impairments that could be identified, the primary goal was to achieve improvement in impaired function and muscle performance. The treatment protocol focused on the endurance of cervical muscles to treat the inability to sit and study. The patient was seen in physiotherapy for 10 visits for 2 weeks. Each time reassessment of significant impairments and post-treatment subjective evaluation were done. Ergonomic education was an important part of each therapy session, and the patient was told not to sit for prolonged duration and was advised to move out of painful postures whenever it becomes painful due to prolonged sustenance. Patient education was an important factor to let the patient acknowledge the pathoanatomical diagnosis and remain active to lead a pain-free life.
Low-load motor control exercises for the upper quarter were initiated along with manual traction to the cervical region. Before initiating the exercise a hot pack application over the painful region was done. Home exercise program focused on a structured set of exercises focused on mobility and strength. The exercise protocol is summarized in Table 1. The pain and sitting duration were significantly better after a week of therapy sessions. After two weeks of supervised management, he was advised for a regular home exercise program for 8 weeks. The home exercise program was necessary to remove the mechanical stressors of pain and improve the lack of strength to maintain a sustained posture for a long period of time.
Rehabilitation protocol
| Exercise | Instruction(s) |
| Supine lying chin tucks | The patient’s head was supported on the couch. The patient is asked to pull the chin towards the sternum or neck area without holding his breath. The position was maintained for five seconds. |
| Middle-trapezius hold relax | The patient’s head is held inside flexion (mid-range) supported on a pillow and the patient is asked to apply pressure on the therapist’s hand which is placed on the side of the patient’s head and held for 10 s and then relax it. |
| Rotations end range (pain-free) | The patient’s head is supported on the pillow and rotation of the neck is done to the maximum available range of the neck which is painless. Holding the range for 10 s on each side. |
| Extension hold | The patient’s head is supported on the couch and the patient was asked to apply pressure on the pillow and hold the contraction for 5 s and repeat it for 5 times. |
| Prone extensions | The patient was made to lay face down, hands parallel to trunk, the patient lifted the chest and shoulder to the level of full available extension of the spine and maintained the position for 10 s. |
| Planks on hands with head neutral | Patient’s feet hip-width apart, hands shoulder-width apart, and directly under shoulders. Form a straight line from shoulders to heels by lifting your body and maintaining the position for 10 s. |
| Prone lying alternate leg and arm lift | Patient’s head in neutral in a face-down position, alternate lifting of arm and opposite leg together holding the position for 10 s. |
| Prone lying scapular retractions T/Y | Patient’s head kept neutral in face-down position, both shoulders in abducted to 90 degrees ‘T’ and doing retractions 10 repeats and with head kept neutral in face-down position, both shoulders in flexed to 120 degrees in thumbs-up position ‘Y’ and doing retractions 10 repeats. |
| ROM exercises | All ROM exercises for the neck and shoulder are to be performed in the seated position. |
Each exercise was performed as 3 sets × 10 repetitions and gradually the sets and repetitions were increased
Outcome measures
The two outcomes used for the patient, NPRS was used to rate pain intensity during rest and at sitting. The other being sitting duration without getting discomfort. On the initial visit, the pain intensity on NPRS was 8 which eventually decreased to 2 on the tenth session. The second outcome was documented as time, on an initial visit he described that after 10 min of sitting the discomfort started which on the tenth session improved to 30 min.
Discussion
The case report demonstrated a significant decrease in the intensity of pain after 2 weeks of supervised physiotherapy management. The pain intensity decreased from 8 (NPRS) to 2 (NPRS) which shows a meaningful clinical change [6, 7]. The patient reported sitting duration without discomfort also showed a significant improvement. To our knowledge, this is the first study that describes physiotherapeutic intervention for neck pain associated with a block vertebra. Literature supports the findings of the case report and suggests that exercise alone or combined with manual therapy does result in significant pain reduction [8, 9]. However, clinical decisions must not simply rely on the radiological findings (ex block vertebra, spondylosis, etc.), these findings must always be correlated clinically.
The used of specific patient-reported issue as an outcome measure, for example, the sitting duration which showed improvement. This change can be attributed to improvement in muscle performance associated with prescribed exercises. Literatures suggest that individuals with neck pain have been found to have lower muscle strength compared to their healthy controls [10]. Although the hypothesis that improvement in sitting capacity may be due to enhance muscle performance there was no direct measurement of muscle performance in the study.
The protocol used demonstrates that an exercise regimen using strengthening exercises can be effective in reducing the patient’s pain and discomfort. The advice for not sustaining a posture prevented loading and helped in the reduction of pain. A recent study demonstrated the use of ergonomic advice combined with exercises improved the health productivity of individuals at their workplace [11]. Present case report has similar findings in terms of improvement in the patient’s ability to do his daily chores. As block vertebra is usually an incidental finding, the authors suggest more case reports and case series to further explain the therapeutic interventions that can be used for this specific subset of the neck pain population.
In conclusion, patient-reported pain was decreased significantly from the initial visit. In the current case report, patient education and structured exercise program demonstrated an improvement in self-reported function deficit. The patient was able to sit for a longer duration and had a considerable improvement in pain associated with prolonged sitting. A supervised exercise program combined with patient education should be the ideal physiotherapy management for the case of neck pain associated with findings of a block vertebra.
Abbreviations
| C2: |
second cervical vertebra |
| NPRS: |
numeric pain rating scale |
Declarations
Author contributions
SQ: Conceptualization, Investigation, Methodology, Resources, Validation, Visualization, Writing—original draft, Writing—review & editing. AS: Conceptualization, Investigation, Methodology, Validation, Visualization, Writing—original draft, Writing—review & editing. All authors read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent to participate in the study was obtained from all participants.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2023.