Affiliation:
Sport Science Institute, Saarland University, 66123 Saarbrucken, Germany
Email: thomas.haab@uni-saarland.de
ORCID: https://orcid.org/0000-0002-0133-1245
Affiliation:
Sport Science Institute, Saarland University, 66123 Saarbrucken, Germany
ORCID: https://orcid.org/0009-0006-6233-8797
Explor Musculoskeletal Dis. 2024;2:391–407 DOI: https://doi.org/10.37349/emd.2024.00065
Received: June 28, 2024 Accepted: August 08, 2024 Published: September 12, 2024
Academic Editor: Fernando Pérez-Ruiz, Cruces University Hospital, Spain
Background: The aim of the study was to conduct a literature review within the fields of sports and orthopedic rehabilitation to evaluate the efficacy of interventions incorporating electromyographic feedback (EMG FB) training compared to same interventions without EMG FB.
Methods: A systematic search of three databases (PubMed, Cochrane, and Web of Science) was conducted until February 2023, without limitation on the publication date. The search strategy adhered to the PRISMA guidelines. Inclusion criteria and data extraction protocol were established a priori. The methodological quality of the included primary studies was assessed by using the PEDro scale.
Results: A total of ten randomized controlled trials (RCTs; 2 in sports and 8 in orthopedic rehabilitation) involving 397 participants were included. The outcomes were categorized into three areas: 1) muscle strength and activation, 2) pain perception, and 3) functionality and joint range of motion. The quality of these studies ranges from 5 to 8 on the PEDro scale. The findings demonstrate both significant and non-significant differences between the interventions with and without EMG FB across all categories. The calculated effect sizes vary from small to large.
Discussion: This review suggests that EMG FB training can be effective to enhance muscle strength, muscle control, pain reduction, functionality, and joint range of motion. The studies provide evidence for the varying impacts of EMG FB training, demonstrating both significant and non-significant outcomes across different populations and intervention types. These differences within the findings not only highlight the potential of EMG FB, but also emphasize the need for further research to identify the conditions and populations in which EMG FB is most effective.
Surface electromyography (sEMG) feedback has emerged as a valuable tool in sports and orthopedic rehabilitation, providing insights into muscle activity and function during various movements. Biofeedback makes individuals aware of their bodily processes which typically occurs unconsciously and can only be detected with special equipment. sEMG measures muscle activity by detecting muscle action potentials via electrodes. This detected activity can be presented graphically or acoustically for the user. Early experiments by Dale et al. [1] used EMG feedback (EMG FB) from the frontalis muscle, translating muscle activity into an auditory signal. Participants were instructed to alter the tone frequency by tensing or relaxing their facial muscles. Despite significant advancements in EMG technology, that allow muscle activity to control avatars and perform actions like flying or jumping in digital environments [2], the core principle of EMG FB training remains the same. By increasing awareness of muscle activity, individuals can improve their voluntary control over specific muscles. This technique is particularly relevant in orthopedic and neurological rehabilitation, where patients often suffer from muscle atrophy due to impaired voluntary innervation [3]. EMG FB training can enhance the functional recovery of these muscles. Furthermore, such feedback systems are applied in sports to enhance performance and to correct muscular imbalances and weaknesses [4].
An attempt has been made to summarize the current state of knowledge about EMG FB training in a few systematic reviews. However, each of these reviews is limited to the outcomes of EMG FB within a specific subset of research. For instance, Karaborklu Argut et al. [5] focused on the effectiveness of therapeutic EMG FB after orthopedic knee surgeries by examining eight randomized controlled trials (RCTs). They concluded that the feedback method was beneficial for muscle activation, strength, and function. However, they found a lack of evidence for the superiority of feedback training in pain relief and increased joint range of motion (ROM) due to largely non-significant results. In contrast to Karaborklu Argut et al. [5], Xie et al. [6] investigated the effect of such training post-knee surgery through a meta-analysis of six RCTs and concluded that feedback training was superior to regular training in terms of ROM but not in pain relief and physical function. In addition, Kamonseki et al. [7] who reviewed five RCTs, concluded that additional EMG FB had no added positive effect on shoulder pain and function after shoulder surgeries.
The findings of existing systematic reviews appear contradictory. The limited scope of the reviewed studies as well as the small number of included studies result in limited applicability and generalizability of the conclusions. Therefore, a more comprehensive review, without restricting the intervention background, is needed to evaluate the method of sEMG feedback training. This systematic review aims to address this research gap and explore the role and effectiveness of sEMG feedback in sports and orthopedic rehabilitation.
The literature search process was performed systematically and followed to guidelines of the Cochrane Handbook for Systematic Reviews of Interventions [8]. Initially, during the title screening phase, the titles of studies identified in three databases (PubMed, Cochrane, and Web of Science) using specified descriptors (Table S1) were reviewed to identify suitable studies. During the second phase, the abstracts of these studies were compared against the inclusion criteria to exclude unsuitable studies. At this stage, it was crucial that EMG FB was explicitly mentioned in the study. Studies that only referred to biofeedback or feedback in general in their abstracts were excluded. In the full-text screening phase, the complete text of the studies was examined for inclusion.
Throughout the screening process, the web-based platform Rayyan.ai [9] was used to streamline and enhance the efficiency of literature selection.
The research was conducted by using the online databases PubMed, Cochrane, and Web of Science. These databases were searched utilizing keywords combined into search strings with Boolean operators (AND, OR, NOT). To identify relevant keywords, a preliminary search was performed. This involved entering various keyword combinations into the three databases to observe changes in search results. This approach ensured that all significant keywords were identified for the subsequent systematic search and that all irrelevant or disruptive keywords could be excluded. Filters, such as restricting publication type or publication date, were deliberately not applied to avoid prematurely excluding potentially relevant primary studies.
The combination of the search terms resulted in various search strings, tailored to each database. It is important to note that three different search strings were utilized, as each database accepts different combinations and connections of keywords. For instance, Medical Subject Headings (MeSH) Terms were applied only within the PubMed and Cochrane searches; using them in the Web of Science database would result in a faulty search with no results. Table S2 exemplifies the search string created in PubMed after entering and linking the search terms in the “Advanced Search” feature. This example demonstrates the use of MeSH terms specific to PubMed, ensuring a precise and targeted search within this database. Similar approaches were tailored for Cochrane and Web of Science, with adjustments made to meet their specific search requirements.
The inclusion criteria were established to filter the studies regarding their relevance and quality for the systematic review. These criteria were defined a priori and are detailed in Table S3.
The methodological quality of the primary studies was assessed using the PEDro scale (Table 1) [10]. Each item on the scale was rated as either positive (fulfilled) or negative (not fulfilled). The criteria were considered fulfilled if the study description explicitly mentioned meeting the criterion or implicitly indicated fulfillment by providing relevant data. Given the nature of exercise and orthopedic intervention studies, it is often challenging to blind subjects (Item 5), therapists (Item 6), or assessors (Item 7). Therefore, in this review, a score of 8 points on the PEDro scale is already considered as high quality.
Methodological quality assessment of included studies (PEDro scores)
| Study | Item* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ∑ | |
| Ahmed et al. [21] | + | + | – | + | – | – | – | + | + | + | + | 7 |
| Anwar et al. [14] | + | + | – | + | – | – | – | – | – | + | + | 5 |
| Anwer et al. [15] | + | + | – | + | + | – | – | + | + | + | + | 8 |
| Croce [22] | + | + | – | + | – | – | – | – | – | + | + | 5 |
| Farì et al. [19] | + | + | – | + | – | – | – | – | – | + | + | 5 |
| Lucca and Recchiuti [23] | + | + | – | + | – | – | – | + | + | + | + | 7 |
| Oravitan and Avram [16] | + | + | – | + | – | – | – | – | – | + | + | 5 |
| Raeissadat et al. [17] | + | + | – | + | + | – | – | + | + | + | + | 8 |
| Tiryaki et al. [20] | + | + | – | + | – | – | – | – | + | + | + | 6 |
| Yilmaz et al. [18] | + | + | – | + | – | – | – | + | + | + | + | 7 |
* 1: eligibility criteria were specified; 2: subjects were randomly allocated to groups; 3: allocation was concealed; 4: groups were similar at baseline regarding the most important prognostic indicators; 5: blinding of all subjects; 6: blinding of all therapists who administered the therapy; 7: blinding of all assessors who measured at least one key outcome; 8: measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups; 9: all subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analyzed by “intention to treat”; 10: results of between-group statistical comparisons are reported for at least one key outcome; 11: study provides both point measures and measures of variability for at least one key outcome
Data extraction was performed using a predefined coding scheme (Table S4). For each primary study, data were extracted from only two groups: the intervention group that received treatment with EMG FB (EMG FB Group), and a Control Group that received the same treatment without EMG FB. Other groups, such as alternative feedback, or passive control groups, were not considered. The intervention period was defined by the duration of the training intervention. Follow-up assessments or post-intervention measurements conducted after the intervention period were not included. Data for effect size (ES) calculation were extracted and transferred to Microsoft Excel (Microsoft Office, 2019) for analysis.
The ES of the primary studies were calculated according to Hedges and Olkin [11], using the pooled standard deviation. The assessment of the ES was based on Cohen’s criteria [12]: small effect (≥ 0.2), medium effect (≥ 0.5), and large effect (≥ 0.8). It is important to note that for some outcomes, lower values indicate the success of the intervention. For example, in certain pain scales, lower values correspond to reduced pain. To simplify and standardize interpretation, the ES are presented as absolute values, accompanied by descriptive data of the pre- and post-test measurements for the corresponding variables.
This systematic review focused on the role and effectiveness of EMG FB training in sports and orthopedic rehabilitation. A total of 13,707 studies were identified across three databases. After removing 9,017 irrelevant studies (e.g., inappropriate title) and 4,225 duplicates during the Level-1 screening, additional 18 studies were identified from the references of the remaining 465 studies. A flow diagram according to Page et al. [13] is presented in Figure 1. Following a thorough review of titles (Level-1 screening), abstracts (Level-2 screening) and full-text articles (Level-3 screening), 10 primary studies were included in the systematic review, encompassing a total of 397 participants.
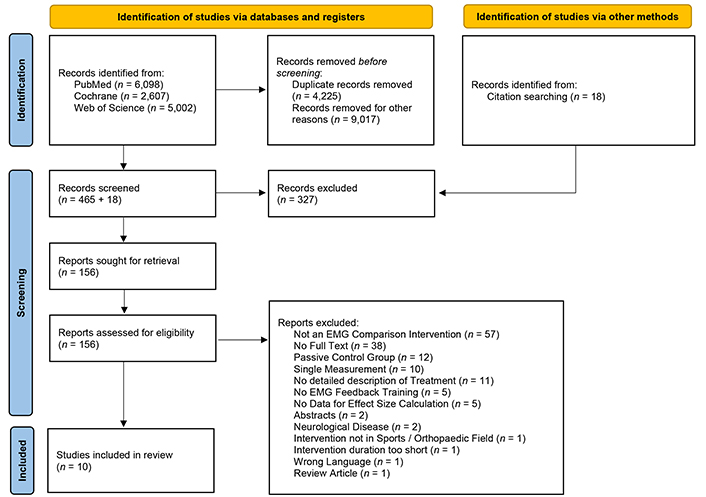
Flow diagram of literature search. EMG: electromyography
Note. Adapted from “The PRISMA 2020 statement: an updated guideline for reporting systematic reviews” by Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. BMJ. 2021;372:n71 (https://www.bmj.com/content/372/bmj.n71). CC BY.
The reviewed studies utilizing EMG FB can be categorized into three sections:
The characteristics of these studies are shown in Tables 2, 3, and 4. The intervention duration varied from 19 days to 8 weeks. The examined muscles included the upper thigh (e.g., quadriceps or hamstrings; n = 7), shoulder (e.g., deltoideus; n = 2), and abdominal muscle (e.g., rectus abdominis; n = 1).
Details of the primary studies for muscle strength and activation
| Study | Treatment | Biofeedback mode | EMG device | Outcome parameter | Outcome values | ES | |
|---|---|---|---|---|---|---|---|
| EMG FB Group | Control Group | ||||||
| [16] | 8 weeks (daily)
| Visual
| Myomed 134 | EMG onset | Pre:562.09 ± 55.33Post:487.92 ± 46.71 | Pre:548.21 ± 64.76Post:538.41 ± 53.58 | 1.01* |
| EMG offset | Pre:687.54 ± 75.39Post:570.17 ± 62. 11 | Pre:701.23 ± 69.52Post:682.31 ± 65.68 | 1.76* | ||||
| Knee flexor strength | Pre:38.23 ± 11.03Post:84.02 ± 6.95 | Pre:37.42 ± 10.48Post:86.04 ± 5.43 | 0.32 | ||||
| Knee extensor strength | Pre:41.75 ± 10.54Post:87. 11 ± 6.54 | Pre:42.92 ± 12.49Post:86.39 ± 6.74 | 0.11 | ||||
| [17] | 8 weeks (12 × 15 min sessions)
| Visual & acoustic
| MyoTrac Infiniti | Electrical activity VM | Pre:207.7 ± 86.7Post:342. 1 ± 108.5 | Pre:223.0 ± 82. 1Post:347.3 ± 86.0 | 0.05 |
| [18] | 3 weeks (3 times every day)
| Visual & acoustic
| Myomed 932 | Knee extension strength 60°/s | Pre:47.84 ± 17.87Post:54.47 ± 17.97 | Pre:50.25 ± 24.2Post:62.95 ± 22.8 | 0.41 |
| Knee flexion strength 60°/s | Pre:32.94 ± 14.38Post:42.26 ± 23.94 | Pre:27.75 ± 18.9Post:40.6 ± 19.79 | 0.08 | ||||
| Knee extension strength 180°/s | Pre:23.68 ± 7.31Post:31.89 ± 9.28 | Pre:24.85 ± 11. 1Post:35.55 ± 12.6 | 0.33 | ||||
| Knee extension strength 180°/s | Pre:17.10 ± 12.95Post:24.10 ± 13.87 | Pre:13.85 ± 11.4Post:22.95 ± 15.5 | 0.08 | ||||
| Knee isometric extension strength | Pre:77.94 ± 28.47Post:103.57 ± 63. 1 | Pre:79.3 ± 26.61Post:83.35 ± 21.4 | 0.43 | ||||
| [20] | 6 weeks (3 times per week)
| Visual & acoustic
| NeuroTrac MyoPlus4 Pro | Shoulder flexion strength | Pre:65.00 ± 20.16Post:78.20 ± 22.87 | Pre:70.55 ± 24. 11Post:74.74 ± 23.54 | 0.15* |
| [21] | 8 weeks (3 times per week)
| Visual
| Myomed 932 | Activation capacity TA | Pre:17.69 ± 2.23Post:35.09 ± 1.31 | Pre:17.59 ± 2.49Post:33.60 ± 2.2 | 0.82* |
| [19] | 4 weeks (2 times per week)
| Visual
| mDurance system | RMS SPlimb affected | Pre:100. 1 ± 13. 1Post:171.5 ± 5.1 | Pre:101.2 ± 11.9Post:145. 1 ± 12.9 | 2.72* |
| RMS SPlimb free | Pre:172.3 ± 6.0Post:182.5 ± 5.2 | Pre:170.9 ± 4.8Post:182.6 ± 8.7 | 0.01 | ||||
| [15] | 5 weeks (5 times per week)
| Visual
| Myomed 932 | Knee isometric extension strength | Pre:9.07 ± 1.87Post:13.68 ± 1.99 | Pre:9.42 ± 1.86Post:11.06 ± 1.56 | 1.47* |
| [22] | 5 weeks (2 times per week)
| Visual & acoustic
| Ouroboros EMG-1821 | IEMG activity QM | Pre:442.95 ± 95.65Post:525.90 ± 112.20 | Pre:407.34 ± 40.81Post:454.97 ± 53.20 | 0.81* |
| Knee extension peak torque | Pre:165.28 ± 30.10Post:234.28 ± 52.63 | Pre:165.85 ± 37.08Post:211.57 ± 40.57 | 0.48* | ||||
| [23] | 19 days (5 times per week)
| Visual
| Cyborg J-33 | Knee extension peak torque trained leg | Pre:113.26 ± 37.01Post:138.59 ± 19.38 | Pre:103.73 ± 25.07Post:103.23 ± 27.50 | 1.49* |
| Knee extension peak torque untrained leg | Pre:114.04 ± 35.27Post:127.78 ± 32.92 | Pre:97.60 ± 22.46Post:95.57 ± 17.52 | 1.22* | ||||
* Significant effects between EMG FB Group and Control Group post intervention. ES: effect size; VL: vastus lateralis muscle; VM: vastus medialis muscle; BF: biceps femoris muscle; SM: semimembranosus muscle; AD: anterior deltoid muscle; RA: rectus abdominis muscle; SP: supraspinatus muscle; RF: rectus femoris muscle; TA: transversus abdominis muscle; QM: quadriceps femoris muscle; IEMG: integrated electromyography; RMS: root mean square
Details of the primary studies for pain perception
| Study | Treatment | Biofeedback mode | EMG device | Outcome parameter | Outcome values | ES | |
|---|---|---|---|---|---|---|---|
| EMG FB Group | Control Group | ||||||
| [14] | 3 weeks (5 days per week)
| Visual
| Myomed 932 | VAS | Pre:6.13 ± 0.18Post:1.53 ± 0.74 | Pre:6.06 ± 1.03Post:2.93 ± 0.88 | 1.72* |
| [16] | 8 weeks (daily)
| Visual
| Myomed 134 | KOOS | Pre:38.23 ± 11.03Post:84.02 ± 6.95 | Pre:37.42 ± 10.48Post:86.04 ± 5.43 | 0.32 |
| [17] | 8 weeks (12 × 15 min sessions)
| Visual & acoustic
| MyoTracInfiniti | VAS | Pre:5.9 ± 1.7Post:2.9 ± 1.6 | Pre:6.1 ± 1.6Post:4.3 ± 1.2 | 0.99* |
| WOMAC pain | Pre:6.0 ± 3. 1Post:4.5 ± 2.6 | Pre:6.5 ± 3.3Post:4.8 ± 2.2 | 0.12 | ||||
| Lequesne pain | Pre:3.6 ± 1.9Post:3.0 ± 1.6 | Pre:4.5 ± 1.4Post:3.8 ± 1.3 | 0.55 | ||||
| [18] | 3 weeks (3 times every day)
| Visual & acoustic
| Myomed 932 | VAS rest | Pre:3.89 ± 2.28Post:1.63 ± 2.06 | Pre:3.65 ± 2.23Post:1.35 ± 1.69 | 0.15 |
| VAS walking | Pre:5.42 ± 2.83Post:2.68 ± 2.49 | Pre:5.95 ± 2.06Post:2.75 ± 2.02 | 0.03 | ||||
| VAS stairs | Pre:7.47 ± 1.95Post:4.52 ± 2.54 | Pre:7.05 ± 1.53Post:3.55 ± 1.84 | 0.44 | ||||
| WOMAC pain | Pre:14.78 ± 4.93Post:9.52 ± 4.42 | Pre:14.30 ± 0.99Post:9.3 ± 3,07 | 0.60 | ||||
| NHPS pain | Pre:63.69 ± 27.71Post:31.72 ± 24.19 | Pre:63.54 ± 25.29Post:28.52 ± 23.67 | 0.13 | ||||
| [20] | 6 weeks (3 times per week)
| Visual & acoustic
| NeuroTrac MyoPlus4 Pro | NPRS | Pre:4.91 ± 1.69Post:2.72 ± 1.72 | Pre:5.52 ± 1.44Post:3.27 ± 1.97 | 0.30* |
| [21] | 8 weeks (2 times per week)
| Visual
| Myomed 932 | VAS | Pre:5.62 ± 0.96Post:0.49 ± 0.69 | Pre:5.57 ± 0.72Post:1.06 ± 0.68 | 0.83* |
| [19] | 4 weeks (2 times per week)
| Visual
| mDurance system | WUSPI | Pre:121.8 ± 8.9Post:54.2 ± 8.5 | Pre:121.60 ± 9.6Post:81.70 ± 6.3 | 3.66* |
* Significant effects between EMG FB Group and Control Group post intervention. ES: effect size; VL: vastus lateralis muscle; VM: vastus medialis muscle; BF: biceps femoris muscle; SM: semimembranosus muscle; RF: rectus femoris muscle; VAS: Visual Analog Scale; KOOS: Knee Injury and Osteoarthritis Outcome Score; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; NHPS: Nottingham Health Profile Score; AD: anterior deltoid muscle; RA: rectus abdominis muscle; SP: supraspinatus muscle; NPRS: Numeric Pain Rating Scale; WUSPI: Wheelchair User’s Shoulder Pain Index
Details of the primary studies for functionality and joint ROM
| Study | Treatment | Biofeedback mode | EMG device | Outcome parameter | Outcome values | ES | |
|---|---|---|---|---|---|---|---|
| EMG FB Group | Control Group | ||||||
| [16] | 8 weeks (daily)
| Visual
| Myomed 134 | KOOS ADL | Pre:29.92 ± 11.72Post:66.83 ± 7.40 | Pre:27.74 ± 9.62Post:64.05 ± 8.48 | 0.35 |
| KOOS sport and recreation function | Pre:6.37 ± 5.26Post:88.41 ± 8.57 | Pre:7.03 ± 6.51Post:83.24 ± 9.29 | 0.58* | ||||
| KOOS quality of life | Pre:27.45 ± 7.38Post:90.54 ± 10.39 | Pre:29.63 ± 5.72Post:88.76 ± 9.54 | 0.18 | ||||
| [21] | 8 weeks (2 times per week)
| Not specified
| Myomed 932 | MODQ | Pre:32.00 ± 5.02Post:2.66 ± 3.04 | Pre:32.04 ± 4.73Post:6.80 ± 3.44 | 1.28* |
| [17] | 8 weeks (12 × 15 min sessions)
| Visual & acoustic
| MyoTrac Infiniti | WOMAC stiffness | Pre:1.8 ± 1.7Post:1.2 ± 1.2 | Pre:2.3 ± 1.6Post:1.7 ± 1. 1 | 0.43 |
| WOMAC function | Pre:19.8 ± 13.0Post:14.6 ± 10.7 | Pre:22.4 ± 11.6Post:17.8 ± 9.4 | 0.32 | ||||
| Lequesne walking | Pre:1.7 ± 1.5Post:1.2 ± 1.2 | Pre:1.6 ± 1. 1Post:1.3 ± 0.8 | 0.10 | ||||
| Lequesne ADL | Pre:3.7 ± 1.8Post:3.1 ± 1.6 | Pre:3.6 ± 1.3Post:3.0 ± 1. 1 | 0.07 | ||||
| [18] | 3 weeks (3 times every day)
| Visual & acoustic
| Myomed 932 | WOMAC stiffness | Pre:4.31 ± 1.7Post:3.42 ± 1.57 | Pre:4.15 ± 1.81Post:3.0 ± 8.07 | 0.07 |
| WOMAC function | Pre:49. 1 ± 12.44Post:33.42 ± 11.74 | Pre:47.6 ± 0.07Post:32.45 ± 9.08 | 0.09 | ||||
| NHPS physical mobility | Pre:45.03 ± 21.46Post:28.10 ± 17.08 | Pre:37.59 ± 21.15Post:25.33 ± 18.41 | 0.16 | ||||
| [19] | 4 weeks (2 times per week)
| Visual
| mDurance system | ROM abduction | Pre:100.8 ± 3.8Post:114.5 ± 5.8 | Pre:100.7 ± 3.4Post:109.8 ± 2.6 | 1.03* |
| ROM external rotation | Pre:59.6 ± 6.9Post:74.0 ± 3.2 | Pre:59. 1 ± 7.9Post:66.9 ± 7.2 | 1.29* | ||||
| [20] | 6 weeks (3 times per week)
| Visual & acoustic
| NeuroTrac MyoPlus4 Pro | ROM flexion | Pre:121. 11 ± 17.45Post:137.50 ± 18.16 | Pre:118.88 ± 23.92Post:135.55 ± 19.47 | 0.10* |
| ROM abduction | Pre:121.82 ± 21.96Post:133.64 ± 18.17 | Pre:109.57 ± 25.35Post:127.89 ± 18.24 | 0.32 | ||||
| ROM external rotation | Pre:45.83 ± 9.74Post:58.89 ± 6.76 | Pre:45.00 ± 10.58Post:59.17 ± 6.69 | 0.04 | ||||
| ROM internal rotation | Pre:30.83 ± 5.05Post:35.83 ± 6.02 | Pre:28.44 ± 6.42Post:37.50 ± 4.92 | 0.30 | ||||
* Significant effects between EMG FB Group and Control Group post intervention. ES: effect size; VL: vastus lateralis muscle; VM: vastus medialis muscle; BF: biceps femoris muscle; SM: semimembranosus muscle; RA: rectus abdominis muscle; KOOS: Knee Injury and Osteoarthritis Outcome Score; MODQ: Modified Oswestry Disability Questionnaire; WOMAC: Western Ontario and McMaster Universities osteoarthritis index; ADL: activities of daily living; NHPS: Nottingham Health Profile Score; AD: anterior deltoid muscle; SP: supraspinatus muscle; ROM: range of motion
The evaluation of the individual studies is summarized in Table 1. All primary studies explicitly reported the random assignment of participants (Item 2). Additionally, all studies provided both point measures and measures of variability (Item 11) for at least one key outcome, as well as results of statistical group comparisons (Item 10). All studies described the inclusion and exclusion criteria for participant recruitment (Item 1).
The studies included various participants:
Four studies included patients with knee osteoarthritis [14, 15, 17, 18].
One study included patients in a knee meniscal repair program [16].
One study included patients in shoulder pain rehabilitation [19].
One study included patients with shoulder rotator cuff tears [20].
One study included patients with chronic low back pain [21].
Two studies included healthy participants for strength acquisition [22, 23].
All studies provided information on the comparability of prognostic indicators at the start of the study (Item 4). In five studies, at least one key outcome was measured in which at least 85% of the participants originally assigned to groups (Item 8). In order to rate Item 9 positive, studies had to report the number of participants who received the intervention or control treatment and the number of participants available for outcome measurement. If these numbers matched, it was assumed that they referred to the same individuals.
No study reported concealed allocation (Item 3). As mentioned earlier, Items 5, 6, and 7 related to blinding are rarely met in most sport science studies, due to inherent difficulties. However, Anwer et al. [15] and Raeissadat et al. [17] reported blinding of participants by placing electrodes on the muscles in the non-EMG FB group without activating the feedback device.
Overall, the methodological quality of the included studies was moderate, with a score of 6.3 ± 1.2 points on the PEDro scale.
Muscle strength was assessed through dynamic and isometric strength measurements and joint angle torque, while muscle activation was evaluated using EMG parameters such as root mean square (RMS) or integrated electromyography (IEMG).
Five studies examined muscle activation following EMG FB training (Table 2). Croce [22] found that the EMG FB Group exhibited significantly greater increases in integrated electromyographic levels compared to the non-feedback group. Oravitan and Avram [16] demonstrated that electromyographic feedback in a rehabilitation program post-meniscal repair increased the electrical potential of thigh muscles during contraction and decreased the time to initiate (EMG onset) and relax muscle contraction (EMG offset). Farì et al. [19] reported a significant increase in muscle activity (RMS) in the supraspinatus muscle after rehabilitation exercises for shoulder pain in the EMG FB Group compared to the Control Group. Ahmed et al. [21] indicated that adding EMG FB to trunk stabilization exercises led to greater improvement in transverse abdominis activation capacity of patients with chronic low back pain. Raeissadat et al. [17] observed significant increases in vastus medialis muscle activity of patients with knee osteoarthritis in both groups (EMG FB Group and Control Group). However, no greater improvements were seen in the EMG FB Group compared to the Control Group.
Six studies evaluated muscle strength following EMG FB training (Table 2). Oravitan and Avram [16] found that EMG FB training did not significantly affect muscle strength. Yilmaz et al. [18] reported significant improvements in muscle strength in both the strengthening exercise group and the EMG FB-assisted strengthening exercise group, with no significant difference between the two groups. Tiryaki et al. [20] observed statistically superior improvements in shoulder flexion strength in the EMG FB Group compared to the Control Group among participants with rotator cuff tears; however, the ES was low (ES = 0.15). Anwer et al. [15] found that adding EMG biofeedback to a 5-week isometric exercise program led to greater increases in quadriceps muscle strength compared to the exercise program alone in individuals with knee osteoarthritis. Croce [22] demonstrated that the EMG FB Group showed significantly greater increases in peak torque of knee extension exercises compared to the non-feedback group. Lucca and Recchiuti [23] revealed that the combination of isometric exercise and EMG FB led to greater gains in knee extension peak torque compared to isometric exercise alone over a 19-day training period in female undergraduate students.
Pain perception was assessed using various questionnaires and indexes, including the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Visual Analog Scale (VAS), Knee Injury and Osteoarthritis Outcome Score (KOOS), Nottingham Health Profile Score (NHPS), Wheelchair User’s Shoulder Pain Index (WUSPI), Numeric Pain Rating Scale (NPRS), and Lequesne Questionnaire (Table 3).
Anwar et al. [14] revealed that adding EMG FB to an isometric exercise program led to greater reductions in pain intensity compared to isometric exercise alone in patients with knee osteoarthritis over a 3-week period. Oravitan and Avram [16] showed that pain was not significantly influenced by adding EMG FB training to a meniscal rehabilitation program, as no significant differences were found between the EMG FB Group and the Control Group. Raeissadat et al. [17] used three different pain measurements and found that the EMG FB Group showed significantly greater improvements only in the VAS score. Yilmaz et al. [18] revealed significant improvements in pain scores in both the strengthening exercise group and the EMG feedback-assisted strengthening exercise group, while there was no significant difference between the two groups.
Farì et al. [19] reported that the WUSPI decreased significantly in the EMG FB Group compared to the Control Group after rehabilitation exercises for shoulder pain. Tiryaki et al. [20] observed significant improvements in pain scores but noted no significant differences between the groups. Ahmed et al. [21] found that the EMG FB Group showed a significant reduction in pain intensity after six weeks of an eight-week intervention compared to the Control Group.
Functionality was assessed using various questionnaires and indexes, including the WOMAC, KOOS, NHPS, Modified Oswestry Disability Questionnaire (MODQ), and Lequesne Questionnaire. Joint ROM was assessed through joint angle measurements (ROM).
Four studies scrutinized functionality after EMG FB training (Table 4). Oravitan and Avram [16] found better results in the KOOS subscale for sport and recreational function in the EMG FB Group compared to the Control Group. Ahmed et al. [21] revealed a significant reduction in functional disability in the EMG FB Group after six weeks of an eight-week intervention compared to the Control Group. Raeissadat et al. [17] showed a significant increase in functionality in patients with knee osteoarthritis in both the EMG FB Group and Control Group, but no difference between groups. Yilmaz et al. [18] reported significant improvements in functionality in both the strengthening exercise group and the EMG feedback-assisted strengthening exercise group, but no significant difference between the two groups.
Two studies examined joint ROM after EMG FB training. Farì et al. [19] revealed that the group performing exercises with EMG FB showed greater and faster improvements in shoulder joint ROM compared to the group undergoing a standard rehabilitation program. Tiryaki et al. [20] observed significant improvements in shoulder joint ROM but found no significant differences between the groups.
This systematic review examined the role and effectiveness of surface EMG FB training in sports and orthopedic rehabilitation based on 10 primary studies.
Muscle strength and activation showed partial benefits of additional EMG FB. For instance, Ahmed et al. [21] found significant differences in the muscle activity of the transversus abdominis muscle after an eight-week core training program with a gym ball and visual feedback, compared to the same training without feedback. Similarly, Croce [22] observed significantly higher EMG values of the quadriceps femoris muscle in the dominant leg after a five-week isokinetic machine training when both visual and auditory feedback were provided simultaneously. The authors suggested that EMG FB leads to higher recruitment of motor units at the onset of contraction, which can be maintained throughout the contraction. Additionally, they proposed that EMG FB increases motivation, which in turn promotes higher electrical activity in the brain and positively impacts the recruitment rate. Anwer et al. [15] demonstrated that isometric strength of the quadriceps femoris muscle in a population with knee osteoarthritis significantly increased by 23% after a five-week isometric strength training with visual EMG FB, compared to training without EMG FB. They attributed the strength gains to an increase in the motor unit firing rate and recruitment patterns. In contrast, Yilmaz et al. [18] revealed significant improvements in muscle strength in both the strengthening exercise and the EMG FB-assisted strengthening exercise groups, but there was no significant difference between the two groups.
We found large ES in favor of additional EMG FB for pain reduction, even though there were also non-significant differences between the EMG FB Group and the Control Group. Raeissadat et al. [17] measured subjective pain perception using the VAS before and after a two-month isometric strength training program of participants with knee osteoarthritis. They found significant differences between the groups, and subsequent calculations showed a large ES. Since all other dependent variables in the study by Raeissadat et al. [17] showed no significant differences between the groups, the authors attributed the subjective pain relief to a purely psychological effect. Similarly, Anwar et al. [14] observed pain reductions using VAS through EMG FB in participants with knee osteoarthritis.
Ahmed et al. [21] demonstrated an increase in muscle activity of the transversus abdominis muscle, which, according to the authors, corresponded with pain reduction mediated by enhanced spinal stability. Pain reductions in control groups that exceeded those in the intervention groups were minimal to small. Several non-significant effects were found in the pain category. For instance, Yilmaz et al. [18] reported improvements in both the EMG FB Group and Control Group with small ES after a three-week lower extremity strength training program for participants with knee osteoarthritis in terms of pain at rest, during walking, and during stair climbing, without significant differences between the groups (P > 0.05).
These findings indicate that EMG FB training can have varying effects on pain perception, with some studies showing significant benefits, while others report no significant differences between intervention and control groups.
Functionality was predominantly measured in orthopedic interventions using questionnaires such as the KOOS and the WOMAC. Oravitan and Avram [16] assessed functionality after a rehabilitation program in participants who had undergone meniscus surgery using subscales of the KOOS scores. After eight weeks, a medium ES was calculated in favor of the EMG FB Group only in the sport and recreation function subcategory. All other primary studies in this review, except for the study by Ahmed et al. [21], showed no differences between treatment with or without EMG FB.
Joint ROM, primarily involving the shoulder joint, was generally positively influenced by EMG FB. Farì et al. [19] observed larger ES values in shoulder abduction and external rotation in wheelchair basketball players with shoulder pain after EMG FB training of the supraspinatus compared to the control intervention. However, the study by Tiryaki et al. [20] showed significant differences favoring the EMG FB Group only in shoulder flexion, with a very small ES. All other ROM measurements in this study showed no significant differences between the groups.
These findings indicate that EMG FB training can lead to significant improvements in muscle strength and activation, pain perception and functionality and joint ROM in some cases, although results may vary depending on the specific condition and intervention protocol used. Further research is needed to better understand the specific contexts in which EMG FB training is most effective.
In conclusion, the present literature review indicates that EMG FB training can be effective to enhance muscle strength, pain reduction, and functional recovery in specific contexts. However, it should be noted that the studies were too heterogeneous to draw a general conclusion. Most of the studies were conducted in a rehabilitation setting, with only two studies involving healthy athletes.
In sports, EMG FB can play a crucial role in enhancing athletic performance and optimizing training protocols by providing real-time data on muscle activation patterns. This allows athletes to fine-tune their movements and improve efficiency. In orthopedic rehabilitation, EMG FB contributes to assessing muscle recruitment patterns, aiding in the design of personalized rehabilitation programs and monitoring progress post-injury or surgery. The use of surface EMG FB in rehabilitation programs offers numerous benefits. In addition to the effects reported in this review, such as targeted muscle strengthening and enhanced functional outcomes, the studies also reported increased patient engagement and improved muscle coordination. EMG FB helps patients gain better control over their muscles, which is essential for recovery and performance improvement. Despite the positive indications, further research is needed to establish standardized protocols and determine the most effective applications of EMG FB training across different populations and settings.
EMG FB: electromyographic feedback
ES: effect size
KOOS: Knee Injury and Osteoarthritis Outcome Score
MODQ: Modified Oswestry Disability Questionnaire
NHPS: Nottingham Health Profile Score
NPRS: Numeric Pain Rating Scale
RCTs: randomized controlled trials
RMS: root mean square
ROM: range of motion
sEMG: surface electromyography
VAS: Visual Analog Scale
WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index
WUSPI: Wheelchair User’s Shoulder Pain Index
The supplementary material for this article is available at: https://www.explorationpub.com/uploads/Article/file/100765_sup_1.pdf.
The authors would like to thank Laura Batliwala for her proofreading and suggestions for improvement during the preparation of this manuscript.
TH: Conceptualization, Validation, Investigation, Writing—original draft, Supervision. PL: Conceptualization, Validation, Writing—review & editing. PB: Conceptualization, Investigation, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
All datasets for this study are included in the manuscript and the supplementary files.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
