-
 Special Issue Topic
Special Issue TopicEmerging Concepts in Subarachnoid Hemorrhage
Submission Deadline: September 30, 2022Guest Editor
Dr. Brandon Lucke-Wold E-Mail
Department of Neurosurgery, University of Florida, Gainesville, FL 32608, USA.
Research Keywords: subarachnoid hemorrhage; neurosurgery; neurotrauma; simulation
About the Special Issue
Subarachnoid hemorrhage (SAH) continues to present serious challenges for clinicians and researchers. High morbidity and mortality exist with 1/3 of patients never making it to the hospital. As endovascular techniques have emerged, safe and more efficient aneurysm securement options are now available. The shift has become a focus on secondary mechanisms that occur after the initial hemorrhage. It is well known that vasospasm and delayed cerebral ischemia develop days to weeks after injury. What is still poorly understood are the contributory mechanisms leading to these downstream cascades. This has limited the development of effective therapeutics. This special issue will focus on those emerging topics. We are interested in both clinical and pre-clinical studies as well as focused reviews. Topics of particular importance include the role of microglia, the neuroinflammatory surge, and how the glymphatic system may contribute. Authors are encouraged to provide novel and innovative research to address such topics and help propel the field forward. This forum offers a unique advantage for sharing ideas and encouraging collaborative efforts.
Keywords: subarachnoid hemorrhage; neuroinflammation; vasospasm; delayed cerebral ischemia; glymphatics
Published Articles
 Tension pneumocephalus as a complication of surgical evacuation of chronic subdural hematoma: case report and literature reviewOpen AccessCase ReportThe management of symptomatic chronic subdural hematoma (CSDH) is surgical evacuation and prognosis in most cases is good. Tension pneumocephalus is the presence of air under pressure in the intracr [...] Read more.Mohammed A. Azab ... Brandon Lucke-WoldPublished: August 23, 2023 Explor Neuroprot Ther. 2023;3:177–185
Tension pneumocephalus as a complication of surgical evacuation of chronic subdural hematoma: case report and literature reviewOpen AccessCase ReportThe management of symptomatic chronic subdural hematoma (CSDH) is surgical evacuation and prognosis in most cases is good. Tension pneumocephalus is the presence of air under pressure in the intracr [...] Read more.Mohammed A. Azab ... Brandon Lucke-WoldPublished: August 23, 2023 Explor Neuroprot Ther. 2023;3:177–185
DOI: https://doi.org/10.37349/ent.2023.00046 Reversible cerebral vasoconstriction syndrome: a clinical and therapeutic challengeOpen AccessReviewReversible cerebral vasoconstriction syndrome (RCVS) is characterized by thunderclap headache and intracranial segmental vasoconstriction with or without signs of neurological deficit with a variabl [...] Read more.Andrés Ricaurte-Fajardo ... Nathalia Melo GonzalezPublished: April 28, 2023 Explor Neuroprot Ther. 2023;3:120–130
Reversible cerebral vasoconstriction syndrome: a clinical and therapeutic challengeOpen AccessReviewReversible cerebral vasoconstriction syndrome (RCVS) is characterized by thunderclap headache and intracranial segmental vasoconstriction with or without signs of neurological deficit with a variabl [...] Read more.Andrés Ricaurte-Fajardo ... Nathalia Melo GonzalezPublished: April 28, 2023 Explor Neuroprot Ther. 2023;3:120–130
DOI: https://doi.org/10.37349/ent.2023.00041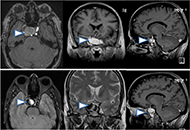 Paraclinoid unruptured giant aneurysm with therapeutic successOpen AccessCase ReportThe global prevalence of intracranial aneurysms (IA) ranges from 5–10%, with a demographic variation. Large and giant aneurysms typically involve cavernous and paraclinoid se [...] Read more.Gonçalo JanuárioPublished: August 30, 2022 Explor Neuroprot Ther. 2022;2:174–181
Paraclinoid unruptured giant aneurysm with therapeutic successOpen AccessCase ReportThe global prevalence of intracranial aneurysms (IA) ranges from 5–10%, with a demographic variation. Large and giant aneurysms typically involve cavernous and paraclinoid se [...] Read more.Gonçalo JanuárioPublished: August 30, 2022 Explor Neuroprot Ther. 2022;2:174–181
DOI: https://doi.org/10.37349/ent.2022.00027 Delayed cerebral ischemia and therapeutic approaches after subarachnoid hemorrhageOpen AccessReviewDelayed cerebral ischemia after subarachnoid hemorrhage is one of the most important causes of mortality and poor functional outcome in patients. Initially, the etiology and treatment of delayed cer [...] Read more.Fettah Eren ... Sueda Ecem YilmazPublished: August 22, 2022 Explor Neuroprot Ther. 2022;2:162–173
Delayed cerebral ischemia and therapeutic approaches after subarachnoid hemorrhageOpen AccessReviewDelayed cerebral ischemia after subarachnoid hemorrhage is one of the most important causes of mortality and poor functional outcome in patients. Initially, the etiology and treatment of delayed cer [...] Read more.Fettah Eren ... Sueda Ecem YilmazPublished: August 22, 2022 Explor Neuroprot Ther. 2022;2:162–173
DOI: https://doi.org/10.37349/ent.2022.00026 The glymphatic system and subarachnoid hemorrhage: disruption and recoveryOpen AccessReviewThe glymphatic system, or glial-lymphatic system, is a waste clearance system composed of perivascular channels formed by astrocytes that mediate the clearance of proteins and metabolites from the b [...] Read more.Stephan Quintin ... Brandon Lucke-WoldPublished: June 21, 2022 Explor Neuroprot Ther. 2022;2:118–130
The glymphatic system and subarachnoid hemorrhage: disruption and recoveryOpen AccessReviewThe glymphatic system, or glial-lymphatic system, is a waste clearance system composed of perivascular channels formed by astrocytes that mediate the clearance of proteins and metabolites from the b [...] Read more.Stephan Quintin ... Brandon Lucke-WoldPublished: June 21, 2022 Explor Neuroprot Ther. 2022;2:118–130
DOI: https://doi.org/10.37349/ent.2022.00023 Subarachnoid hemorrhage: management considerations for COVID-19Open AccessReviewSubarachnoid hemorrhage (SAH) has deleterious outcomes for patients, and during the hospital stay, patients are susceptible to vasospasm and delayed cerebral ischemia. Coronavirus disease 2019 (COVI [...] Read more.Eric J. Panther, Brandon Lucke-WoldPublished: March 02, 2022 Explor Neuroprot Ther. 2022;2:65–73
Subarachnoid hemorrhage: management considerations for COVID-19Open AccessReviewSubarachnoid hemorrhage (SAH) has deleterious outcomes for patients, and during the hospital stay, patients are susceptible to vasospasm and delayed cerebral ischemia. Coronavirus disease 2019 (COVI [...] Read more.Eric J. Panther, Brandon Lucke-WoldPublished: March 02, 2022 Explor Neuroprot Ther. 2022;2:65–73
DOI: https://doi.org/10.37349/ent.2022.00018 -
-
Ongoing Special Issues
-
Completed Special Issues