Biologic drugs and allergen immunotherapy: potential allies
Allergen-specific immunotherapy (AIT) is a proven efficacy treatment for allergic rhinitis (AR), asthma, and Hymenoptera venom allergy, but its use in food allergy (FA) is still under investigation.
[...] Read more.
Allergen-specific immunotherapy (AIT) is a proven efficacy treatment for allergic rhinitis (AR), asthma, and Hymenoptera venom allergy, but its use in food allergy (FA) is still under investigation. Because some efficacy and safety concerns still remain, biologic drugs, including omalizumab and dupilumab, have been studied as an adjunctive therapy to AIT for these conditions. In this article, the evidence supporting the use of monoclonal antibodies (mAbs) as an add-on therapy to AIT for FA, AR, asthma, and Hymenoptera venom allergy has been reviewed. The review will delve into the mechanisms of action of different mAbs, their efficacy, and how they can be integrated into personalized medicine approaches to treat allergic diseases. Furthermore, future research areas will be considered. Evidence suggests that omalizumab in combination with AIT may be a beneficial option for respiratory allergies or food desensitisation, especially during the escalation or build-up phase, when adverse events are more frequent. Currently, there is a small number of well-structured clinical trials in Hymenoptera venom allergy, and the available data consist mainly of single-case reports that provide information of limited value. Dupilumab has been studied as adjunctive therapy in patients with respiratory and FAs. Clinical trials are ongoing to evaluate the efficacy of dupilumab as monotherapy or as an adjunct to oral immunotherapy (OIT) in peanut allergy. Other studies are investigating the use of dupilumab in patients with multiple FAs and as an adjunct to milk OIT. Overall, mAbs have the potential to improve outcomes in various allergic conditions when used as an add-on to AIT, especially during the build-up phase. Further research is needed to fully understand their optimal dosing and duration of treatment, as well as to identify which patients may benefit the most from these therapies.
Palma Carlucci ... Danilo Di Bona
View:1508
Download:84
Times Cited: 0
Allergen-specific immunotherapy (AIT) is a proven efficacy treatment for allergic rhinitis (AR), asthma, and Hymenoptera venom allergy, but its use in food allergy (FA) is still under investigation. Because some efficacy and safety concerns still remain, biologic drugs, including omalizumab and dupilumab, have been studied as an adjunctive therapy to AIT for these conditions. In this article, the evidence supporting the use of monoclonal antibodies (mAbs) as an add-on therapy to AIT for FA, AR, asthma, and Hymenoptera venom allergy has been reviewed. The review will delve into the mechanisms of action of different mAbs, their efficacy, and how they can be integrated into personalized medicine approaches to treat allergic diseases. Furthermore, future research areas will be considered. Evidence suggests that omalizumab in combination with AIT may be a beneficial option for respiratory allergies or food desensitisation, especially during the escalation or build-up phase, when adverse events are more frequent. Currently, there is a small number of well-structured clinical trials in Hymenoptera venom allergy, and the available data consist mainly of single-case reports that provide information of limited value. Dupilumab has been studied as adjunctive therapy in patients with respiratory and FAs. Clinical trials are ongoing to evaluate the efficacy of dupilumab as monotherapy or as an adjunct to oral immunotherapy (OIT) in peanut allergy. Other studies are investigating the use of dupilumab in patients with multiple FAs and as an adjunct to milk OIT. Overall, mAbs have the potential to improve outcomes in various allergic conditions when used as an add-on to AIT, especially during the build-up phase. Further research is needed to fully understand their optimal dosing and duration of treatment, as well as to identify which patients may benefit the most from these therapies.
 Small airway dysfunction and impulse oscillometry in adult patients with asthma: recent findingsOpen AccessMini ReviewAsthma is a respiratory disease affecting more than 300 million people around the world. Airflow obstruction and inflammation due to asthma usually involve large airways, but recently small airway i [...] Read more.Marcello Cottini ... Alvise BertiPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:163–173
Small airway dysfunction and impulse oscillometry in adult patients with asthma: recent findingsOpen AccessMini ReviewAsthma is a respiratory disease affecting more than 300 million people around the world. Airflow obstruction and inflammation due to asthma usually involve large airways, but recently small airway i [...] Read more.Marcello Cottini ... Alvise BertiPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:163–173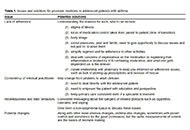 Precision medicine: how to approach the adolescent asthmaticOpen AccessReviewIt is well known that adolescent patients often have less than optimal outcomes. Adolescence is a time of much transition, physically, emotionally, and socially all of which have effects on asthma m [...] Read more.Alan KaplanPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:153–162
Precision medicine: how to approach the adolescent asthmaticOpen AccessReviewIt is well known that adolescent patients often have less than optimal outcomes. Adolescence is a time of much transition, physically, emotionally, and socially all of which have effects on asthma m [...] Read more.Alan KaplanPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:153–162 Safety of 2-day rush induction protocol in sublingual immunotherapy with Pru p 3Open AccessOriginal ArticleAim: Allergy to lipid transfer proteins (LTPs) clinically manifests from oral allergy syndrome (OAS) to anaphylaxis. The risk of systemic symptoms and cross-reactivity make it an important target [...] Read more.Maria Inês T. Silva ... Célia CostaPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:142–152
Safety of 2-day rush induction protocol in sublingual immunotherapy with Pru p 3Open AccessOriginal ArticleAim: Allergy to lipid transfer proteins (LTPs) clinically manifests from oral allergy syndrome (OAS) to anaphylaxis. The risk of systemic symptoms and cross-reactivity make it an important target [...] Read more.Maria Inês T. Silva ... Célia CostaPublished: October 31, 2023 Explor Asthma Allergy. 2023;1:142–152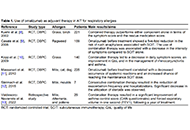 Biologic drugs and allergen immunotherapy: potential alliesOpen AccessReviewAllergen-specific immunotherapy (AIT) is a proven efficacy treatment for allergic rhinitis (AR), asthma, and Hymenoptera venom allergy, but its use in food allergy (FA) is still under investigation. [...] Read more.Palma Carlucci ... Danilo Di BonaPublished: October 20, 2023 Explor Asthma Allergy. 2023;1:126–141
Biologic drugs and allergen immunotherapy: potential alliesOpen AccessReviewAllergen-specific immunotherapy (AIT) is a proven efficacy treatment for allergic rhinitis (AR), asthma, and Hymenoptera venom allergy, but its use in food allergy (FA) is still under investigation. [...] Read more.Palma Carlucci ... Danilo Di BonaPublished: October 20, 2023 Explor Asthma Allergy. 2023;1:126–141 Impact of the GINA asthma guidelines 2019 revolution on local asthma guidelines and challenges: special attention to the GCC countriesOpen AccessReviewThe Global Initiative for Asthma (GINA) provides the most comprehensive and frequently updated guidelines for the management of asthma. The primary aim of guidelines is to bridge the gap between res [...] Read more.Riyad Allehebi, Hamdan AL-JahdaliPublished: October 10, 2023 Explor Asthma Allergy. 2023;1:115–125
Impact of the GINA asthma guidelines 2019 revolution on local asthma guidelines and challenges: special attention to the GCC countriesOpen AccessReviewThe Global Initiative for Asthma (GINA) provides the most comprehensive and frequently updated guidelines for the management of asthma. The primary aim of guidelines is to bridge the gap between res [...] Read more.Riyad Allehebi, Hamdan AL-JahdaliPublished: October 10, 2023 Explor Asthma Allergy. 2023;1:115–125