Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
ORCID: https://orcid.org/0000-0002-9513-193X
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
Affiliation:
2Department of Public Health, University “Federico II” of Naples, 80131 Naples, Italy
ORCID: https://orcid.org/0000-0002-5227-6012
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
Email: klainangela95@gmail.com
ORCID: https://orcid.org/0000-0001-7823-2125
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
ORCID: https://orcid.org/0000-0002-9952-1206
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
Affiliation:
1Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, 80138 Naples, Italy
ORCID: https://orcid.org/0000-0002-8369-5957
Explor Asthma Allergy. 2024;2:340–349 DOI: https://doi.org/10.37349/eaa.2024.00049
Received: March 27, 2024 Accepted: May 10, 2024 Published: July 24, 2024
Academic Editor: Mário Morais-Almeida, CUF Descobertas Hospital, Portuguese Association of Asthmatic Patients, Portugal
The article belongs to the special issue Asthma, Allergies, and Respiratory Infections in Pediatric Age
Aim: This study investigated changes in pediatric respiratory health resulting from the easing of COVID-19-related social restrictions, following a noted decrease in respiratory infections during the lockdown. The COVID-19 restrictions have inadvertently influenced the epidemiology of other viruses and contributed to changes in patterns of recurrent respiratory infections (RRIs) in children.
Methods: This cross-sectional study analyzed the records of children who underwent at “Respiratory Diseases of Pediatric Interest Unit” at the University Hospital “Luigi Vanvitelli” in Naples, Italy, between October 2022 and June 2023. The study aimed to assess associations with RRIs, the occurrence of febrile episodes, and antibiotic usage.
Results: Out of 262 patients (38.2% females, median age 6 years), 81.7% experienced at least one respiratory infection over six months, and 23.7% suffered from RRIs [RRIs in the last six months (RRIS)]. Notably, being underweight was significantly associated with RRIs in the last six months (P-value 0.043), resulting in a 47% increased incidence of respiratory infections (P-value 0.012). No significant associations were observed with sex or age. With increasing age, there was a decreasing incidence rate of 3% for the number of RRIs (P-value 0.019), 4% for febrile episodes (P-value 0.031), and 7% for the number of antibiotic courses (P-value < 0.001).
Conclusions: The study emphasizes age and weight’s role in children’s post-COVID-19 RRI prevalence. It signifies the need for proactive preparedness, targeting younger underweight populations and tailored interventions for recurrent cases.
Respiratory diseases frequently encountered in pediatric practice encompass a range from upper to lower respiratory tract infections. These conditions are predominantly caused by various agents including bacteria (such as Haemophilus influenzae and Streptococcus pneumoniae), viruses [for instance, respiratory syncytial virus (RSV) and adenovirus], and other pathogens (like Chlamydia). These diseases are associated with considerable morbidity and mortality [1]. Approximately 10–15% of children suffer from recurrent respiratory tract infections. However, there is no universal consensus on the definition of recurrent respiratory infections (RRIs) in children [2]. Experiencing multiple respiratory infections during early childhood is a typical phenomenon, playing a pivotal role in the maturation of the immune system. The determination of whether these infections are problematic depends on their severity and frequency. In numerous patients, RRIs are primarily attributed to viral agents, with their occurrence influenced by factors such as age, the developmental stage of the immune system, and environmental elements. However, in certain cases, these infections may be associated with atopy or may signal the presence of an underlying medical condition. It is noteworthy that the manifestation of immune deficiencies characterized solely by respiratory infections, without concurrent infections at other bodily sites, is relatively uncommon [3].
The responsibility of the pediatrician involves discerning whether RRIs in children stem from intrinsic host factors or are a result of heightened environmental exposure, with the latter playing a crucial role. The socioeconomic repercussions of these recurring infections are considerable, necessitating the adoption of preventive strategies. Contemporary approaches in this regard include advocating for breastfeeding, implementing vaccination programs against RSV in pregnancy, and the application of treatments aimed at enhancing immune function. The COVID-19 pandemic has led to a notable decrease in the incidence of major pediatric diseases typically caused by seasonal viruses. The adoption of non-pharmaceutical interventions (NPIs), such as social distancing, wearing masks, rigorous hand hygiene, and restrictions on travel, has played a key role in this temporary epidemiological shift. However, the exact influence of each measure remains to be fully understood. Pediatric conditions, including bronchiolitis, asthma, and gastroenteritis, which are usually prevalent, seemed to have diminished temporarily. The collective impact of these NPIs has effectively hindered human-to-human virus transmission, thereby preventing the formation of local reservoirs for various respiratory viruses [4].
Surveillance studies [5–9] from various countries have demonstrated that the NPIs employed during the COVID-19 pandemic were instrumental in reducing respiratory infections in children. Data collated from South Korea and Japan [5], France [6], Finland [7], rural Alaska [8], and Istanbul [9] uniformly point towards a decline in a range of respiratory illnesses. These outcomes imply that strategies like social distancing, mask-wearing, and travel limitations were pivotal in curtailing respiratory pathogen transmission, thereby enhancing pediatric health. Contrasting this, recent observations from New Zealand and Italy [4]. Additionally, a post-pandemic upswing in conditions such as acute otitis media, adenoiditis, and tonsillitis has been documented [10]. This revival of seasonal viruses extends beyond the relaxation of public health protocols. A likely factor is the diminished protective immunity due to reduced exposure to these pathogens, heightening vulnerability. Moreover, the pandemic’s heightened focus on COVID-19 may have inadvertently weakened immune defenses against other viruses, particularly in children [11–17].
We conducted a cross-sectional study from October 2022 to June 2023 at the University Hospital “Luigi Vanvitelli” in Naples, focusing on children attending the “Respiratory Diseases of Pediatric Interest Unit”. The study’s primary objective was to assess the status of patient access following the easing of COVID-19-related social restrictions [18, 19].
We conducted a cross-sectional study involving children who attended the “Respiratory Diseases of Pediatric Interest Unit”, a tertiary care specialist center, at University Hospital “Luigi Vanvitelli” in Naples, from October 2022 to June 2023. This single-center analysis was chosen as the University Hospital “Luigi Vanvitelli” is centrally located in the largest city of Southern Italy. The study adhered to good clinical practices and the principles of the Declaration of Helsinki. Informed consent was obtained from all patients, permitting the use of anonymized, routinely collected healthcare data, in accordance with the General Data Protection Regulation (GDPR EU2016/679). Furthermore, the study was ethically approved by the Ethics Committee of “Luigi Vanvitelli University” (protocol number 0029465).
In our study, we evaluated several outcomes over the last six months, including the experience of RRIs [RRIs in the last six months (RRIS)] as per the criteria defined in the 2020 intersocietal consensus “the prevention of RRIs” (Table 1) [20], the total number of respiratory infections (n-RI), occurrences of at least one febrile episode (fever), the number of febrile episodes (n-fever), instances of receiving at least one course of antibiotics (antibiotic), and the total number of antibiotic courses prescribed (n-antibiotic).
Definition of RRIs (RRIS) as defined by the 2020 intersocietal consensus “the prevention of RRIs”
| Age group | Definition |
|---|---|
| 1–3 years |
|
| 3–6 years |
|
| 6–12 years |
|
RRIs: recurrent respiratory infections. RRIS: RRIs in the last six months
As for the main variables of interest, we concentrated on the sex, age, and weight of the participants. Weight was further categorized into three classifications: underweight, healthy weight, and overweight [21].
We performed the Shapiro-Wilk test to assess the normality of the distribution of variables. Subsequently, we conducted the Wilcoxon rank-sum test, chi-squared test, and Fisher’s exact test, as appropriate, to identify differences in subgroups. A multivariable logistic model, adjusted for sex, age, and weight, was employed to assess correlates of RRIS. Similarly, a multivariable Poisson regression model, also adjusted for sex, age, and weight, was used to assess the correlates of the number of respiratory infections, febrile episodes, and antibiotic courses in the last six months.
Estimates were presented as odds ratios (ORs), incidence rate ratios (IRRs), and 95% confidence intervals (CIs), as appropriate. P-values lower than 0.05 were considered significant. Statistical analyses were performed using Stata MP 15.0.
We collected data, with reference to the clinical conditions, from October 2022 to June 2023, from 262 outpatient visits between March 2023 and June 2023. 262 patients were visited in the period, 38.2% (100) were females. The median age was 6 years old [interquartile range (IQR) 4 to 9] and the median BMI (body mass index) was 17.8 (IQR 15.67 to 20.93), the majority of the sample was overweight (47.7%) and healthy weight (45.8%). We found no differences between sexes in demographic characteristics. In our pediatric population, 81.7% had experienced at least one respiratory infection (80.0% of females and 82.7% of males) in the last six months, and 23.7% suffered from RRIS (25.0% of females and 22.8% of males) in the last six months. There were no significant differences in RRIs between females and males in the last six months. The majority of patients (67.9%) reported experiencing fever, and a significant portion (65.3%) had used antibiotics in the last six months, with no differences observed between sexes (Table 2).
Descriptive characteristics of the study population
| Item | Female | Male | Whole population | P-value |
|---|---|---|---|---|
| Simple size (% on total) | 100 (38.17) | 162 (61.83) | 262 | |
| Age (median IQR) | 5 (3.5 to 8.5) | 6 (4 to 10) | 6 (4 to 9) | 0.466 |
| BMI (median IQR) | 17.58 (15.70 to 20.32) | 18.04 (15.57 to 21.52) | 17.80 (15.67 to 20.93) | 0.818 |
| Weight | ||||
| Underweight (column %) | 4 (4.00) | 13 (8.02) | 17 (6.49) | 0.424 |
| Healthy weight (column %) | 48 (48.00) | 72 (44.44) | 120 (45.80) | |
| Overweight (column %) | 48 (48.00) | 77 (47.53) | 125 (47.71) | |
| RRIS (column %) | 25 (25.00) | 37 (22.84) | 62 (23.66) | 0.399 |
| At least one respiratory infection (column %) | 80 (80.00) | 134 (82.72) | 214 (81.68) | 0.347 |
| n-RI (median IQR)* | 2 (2 to 4) | 2 (1 to 4) | 2 (1 to 4) | 0.306 |
| Fever (column %) | 66 (66.00) | 112 (69.14) | 178 (67.94) | 0.346 |
| n-fever (median IQR)* | 1 (1 to 2) | 2 (1 to 3) | 1.75 (1 to 2.5) | 0.324 |
| Antibiotic (column %) | 66 (66.00) | 105 (64.81) | 171 (65.27) | 0.477 |
| n-antibiotic (median IQR)* | 2 (1 to 2.75) | 1 (1 to 2) | 2 (1 to 2) | 0.247 |
In the descriptive statistics, the Shapiro-Wilk test, Fisher’s exact test, chi-squared test, and Wilcoxon rank-sum test were utilized, each applied as relevant to the data. *: In these analyses, patients who had not experienced any episodes were excluded from the descriptive evaluation; RRIS: recurrent respiratory infections in the last six months; antibiotic: at least one use of antibiotics in last six months; fever: presence of fever in last six months; n-RI: number of respiratory infections in last six months; n-fever: number of febrile episodes per patient in last six months; n-antibiotic: at least one number of antibiotic courses in last six months. IQR: interquartile range; BMI: body mass index
In the multivariable logistic regression analysis for RRIS, an association was found between being underweight and experiencing RRIS (OR: 3.13, 95% CI 1.04–9.48, P-value 0.043). However, no significant associations were observed with sex or age (Figure 1). Performing Poisson regression analysis, we observed a trend of decreasing incidence rates with increasing age: a 3% decrease in the number of respiratory infections (IRR: 0.97, 95% CI 0.94–0.99, P-value 0.019), a 4% decrease for febrile episodes (IRR: 0.96, 95% CI 0.93–1.00, P-value 0.031), and a 7% decrease in the number of antibiotic courses (IRR: 0.93, 95% CI 0.90–0.97, P-value < 0.001). Underweight patients exhibited a 47% increase in the incidence rate of respiratory infections (IRR: 1.47, 95% CI 1.09–1.98, P-value 0.012). However, no significant correlations were found related to sex or weight categories other than underweight (Figure 2).
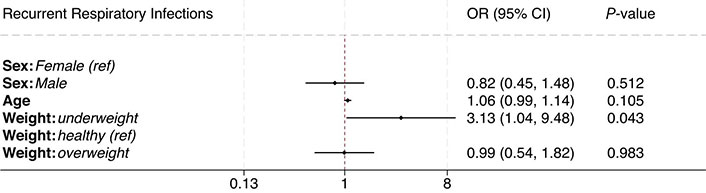
Association between recurrent respiratory infections (RRIs) and demographic characteristics. Outcomes were analyzed employing multivariable logistic regression models, adjusted for sex, age, and weight. Analyses were presented as odds ratio (OR) and 95% confidence intervals (CIs). Ref: reference group
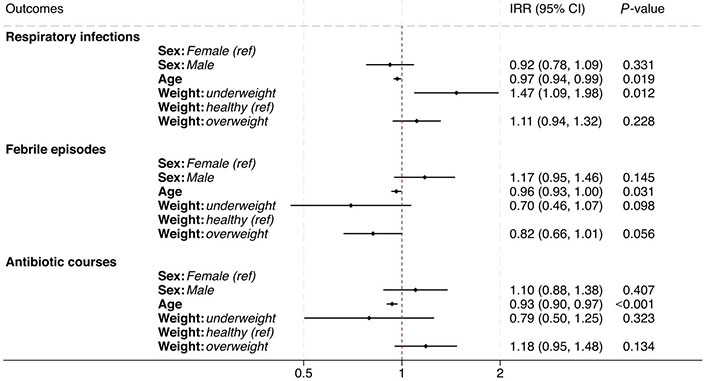
Association between respiratory infections, febrile episodes, and antibiotic courses in the last six months with demographic characteristics. The outcomes were analyzed using multivariable Poisson regression models, which were adjusted for sex, age, and weight. The analyses are presented as incidence rate ratios (IRRs) along with their 95% confidence intervals (CIs). Ref: reference group
In further multivariable Poisson regression models, we also adjusted for the number of respiratory infections, febrile episodes, and antibiotic courses, if they were not the primary outcomes. The analysis found positive correlations between an increasing number of infections, an increasing number of febrile episodes, and an increasing number of antibiotic courses. The collinearity of the number of respiratory infections, febrile episodes, and antibiotic courses was also investigated.
RRIs exhibit extreme heterogeneity concerning their anatomical sites and the pathogens responsible for the infections [1–3]. The incidence is higher in pediatric ages [14], sometimes diminishing or resolving as patients age.
During the study period, our patient cohort was primarily male (61.8%), with a median age of 6 years. Approximately half of these patients were overweight (47.7%), whereas a smaller fraction was underweight (6.5%). Our analysis revealed no substantial gender differences in the population composition.
Within this cohort, a vast majority reported at least one respiratory infection in the past six months, encompassing 80.0% of females and 82.7% of males. Around a quarter of our sample, 23.7%, suffered from RRIs (25.0% females and 22.8% males). Over half had experienced at least one febrile episode in this timeframe (66.0% females and 69.1% males), with a similar proportion completing at least one antibiotic treatment course (66.0% females and 64.8% males). The observed high prevalence of RRIs is reflective of the specialized nature of the tertiary care setting at the University Hospital “Luigi Vanvitelli” in Naples. However, this elevated prevalence might also be attributable to the reduced COVID-19 social restrictions, potentially increasing exposure to respiratory pathogens among children. This supposition aligns with recent findings from New Zealand and Italy, which have indicated a significant post-pandemic increase in bronchiolitis, RSV cases [4], as well as other respiratory conditions such as acute otitis media, adenoiditis, and tonsillitis post-pandemic [10].
Our study did not find any significant difference in the incidence of RRIs or the frequency of respiratory infections over the last six months between male and female patients. While some scientific literature reports a higher incidence and severity of respiratory infections in males, these differences vary depending on the pathogen and the type of infection. Additionally, gender differences in respiratory infection rates are more pronounced in adult populations [22–28]. Our results are not in contrast with the previous scientific literature.
By considering weight categories, we found a higher occurrence of RRIs (OR: 3.13) and episodes of respiratory infections (IRR: 1.47) among underweight patients, consistent with existing literature. Underweight status and malnutrition are known to weaken the immune system, thereby increasing the vulnerability of young patients to respiratory infections [29, 30]. Obesity may be associated with an increased risk of developing atopy, allergies, and asthma, which can elevate the risk of RRIs and respiratory infections, albeit to a lesser extent than being underweight [22, 27, 30–36]. We found no differences between healthy weight and overweight individuals in our population.
In examining age-related trends through our models, we observed a decline in the frequency of respiratory infections (IRR: 0.97), febrile episodes (IRR: 0.96), and the need for antibiotic treatments (IRR: 0.93) with increasing age. The collinearity among these outcomes is noteworthy. This trend, indicative of a decrease in the number of infection episodes with age, aligns with prior research [37, 38], and was evident in our patient cohort. Additionally, this decline in infection episodes was paralleled by a decrease in febrile episodes and antibiotic usage.
The epidemiology of infectious diseases experienced significant changes due to the social restrictions implemented during the COVID-19 pandemic, and with the easing of these restrictions, an increase in the rate of some kinds of infections was observed. This surge could be partly attributed to missed vaccinations and a prolonged period of reduced pathogen exposure spanning nearly two years. The trends we observed in our population are consistent with those reported in other studies investigating post-COVID-19 respiratory infections [39, 40]. Moreover, young age and underweight have already emerged as risk factors of IRRs, along with low socioeconomic level, exposure to cigarette smoke, atopy, and prematurity [41–43].
This study has several limitations. Firstly, it was conducted at a single center in Southern Italy and this factor may limit the generalizability of our findings even though this center is strategically located in the city center of Southern Italy’s most populous city and serves as a tertiary center. Secondly, the cross-sectional retrospective design of our study restricts our possibility of establishing causal relationships between the observed variables. Thirdly, our study faces limitations in sample size. However, it is important to note that our sample was drawn from a tertiary-level referral center, offering a diverse and representative cross-section of the metropolitan and regional population. This aspect does, however, introduce the possibility of selection bias, potentially skewing the sample towards patients with more severe conditions.
Fourthly, our study did not explore factors such as the use of corticosteroids or immunostimulants, nor did it consider the presence of atopy, allergies, asthma, or various environmental exposures. Moreover, we did not account for other potential influencers on the incidence of RRIs like household smoking, vaccination status, pre-existing medical conditions, or the specific pathogens involved in the infections. Addressing these gaps in future studies will be crucial to gaining a more comprehensive understanding of the factors influencing RRIs in children post the COVID-19 pandemic.
Future research should aim to precisely delineate the roles and potential epidemiological shifts of key pathogens in respiratory infections, while also exploring the relative impacts of atopy, allergies, and asthma in comparison to previous COVID-19 infections. It is also important to evaluate the effectiveness of different antibiotic therapies, the usage of corticosteroids or antivirals, the application of immunostimulants or supplements, and the comprehensiveness of vaccination coverage.
In conclusion, our research conducted at the University Hospital “Luigi Vanvitelli” in Naples, a tertiary care center in Southern Italy, offers significant insights into the dynamics of RRIs in children, particularly in the context of the eased COVID-19 social restrictions. Our findings highlight the influence of age and weight on the incidence of RRIs, the frequency of respiratory infections, the number of febrile episodes, and the necessity for antibiotic treatments. Interestingly, our study did not reveal any notable sex-based differences in these aspects. The observed high prevalence of RRIs and increased reliance on antibiotics underscore the continuing challenge these infections pose in pediatric healthcare. This situation accentuates the need for ongoing monitoring, particularly as we adapt to living with COVID-19 and confront the issue of antibiotic resistance.
This study underscores the potential long-term impact of widespread disease prevention strategies, such as those implemented during the COVID-19 pandemic, on the immune response and pathogen exposure in children. It also emphasizes the importance of developing targeted strategies for managing RRIs, especially in vulnerable groups like underweight children. Future research should concentrate on these crucial aspects to enhance the respiratory health of children in the post-COVID-19 era.
CIs: confidence intervals
IRRs: incidence rate ratios
NPIs: non-pharmaceutical interventions
ORs: odds ratios
RRIs: recurrent respiratory infections
RSV: respiratory syncytial virus
CI, LFI, ML, MM, and AK: Conceptualization, Investigation, Writing—original draft, Writing—review & editing. GD, FD, and MMdG: Validation, Writing—review & editing, Supervision. All authors read and approved the submitted version.
Cristiana Indolfi, Angela Klain, Giulio Dinardo, and Michele Miraglia del Giudice who are the Guest Editors of Exploration of Asthma & Allergy had no involvement in the decision-making or the review process of this manuscript. The other authors declare that they have no conflicts of interest.
The present study was approved by the Ethics Committee of “Luigi Vanvitelli University” (protocol number 0029465).
Informed consent to participate in the study was obtained from all participants’ parents.
Not applicable.
The data of this manuscript could be available from the corresponding author upon reasonable request.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2099
Download: 23
Times Cited: 0
Sonila Borici ... Ilir Akshija
Malik Sallam ... Mohammed Sallam
Alberto Vidal, Pedro Cortez
