Abstract
Coronavirus disease 2019 (COVID-19) pandemic was a great challenge for healthcare professionals globally and also for allergists/immunologists. The Pegaso low-care COVID center's experience in managing a low-care center for COVID-19 patients was reported, trying to bring out the relevance of this type of structure in reducing the length of stay of patients in high-care settings with the consequent effect of avoiding the collapse of major hospitals. The experience of managing a low-care setting with a day hospital service inside emphasizes, even more, the role of the allergists/immunologists during the COVID-19 pandemic contributing to keeping the medical staff's specialty in a strategic role in the battle against this common enemy. Sharing all the information on public health organizations is crucial to cope in the best possible way with the present and future challenges.
Keywords
Coronavirus disease 2019, low-care, allergist/immunologistThe rapid global spread of the coronavirus disease 2019 (COVID-19) pandemic has posed a significant challenge to various countries in terms of the capacity of hospitals to admit and care for patients during the crisis. Following the World Health Organization's declaration of public health international emergency due to COVID-19 [1] and the National Declaration of a health emergency, the Tuscany region (Italy) started to organize strategies to counteract severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic outbreak, creating COVID-19 units in internal medicine, intensive and sub-intensive care departments, managed by multi-specialist medical staff redeployed to these units.
Despite this major reorganization, the hospital's capacity was rapidly overwhelmed. At this time, the strategy adopted to reduce the pressure on high-care settings was based on the creation of “ad hoc” low-care structures outside of main hospitals for the management of COVID-19 cases who no longer needed high-intensity care.
In October 2020, in Prato (Tuscany), during the second wave of the COVID-19 pandemic in Italy, started the redevelopment of a decommissioned complex of buildings named Research Center and Education and was located near the main city hospital. The redevelopment project with the creation of a low-care COVID center, named Pegaso, with a mean capacity of 100 beds (expandable to a maximum of 390), was strongly wanted by the President of the Tuscan regional council. At the beginning of December 2020, the renovation work was completed and the clinical management of this low-care center was entrusted to the local unit of Allergy and Clinical Immunology, joined by specialists in other medical disciplines. On December 16th, the first two patients with COVID-19 were admitted at the Pegaso COVID center.
The presence of 24/7 multi-specialist medical staff and nursing care, and the technological equipment of Pegaso allowed to receive patients with high-flow oxygen therapy that have stopped non-invasive ventilation in the previous 48–72 h significantly reducing the average length of stay in high-care settings. From December 16th, 2020 to April 19th, 2022, 1,263 patients were hospitalized in Pegaso coming from different settings (including emergency departments, but only during “crash situations”) of all hospitals present in central Tuscany local health authority (Figure 1).
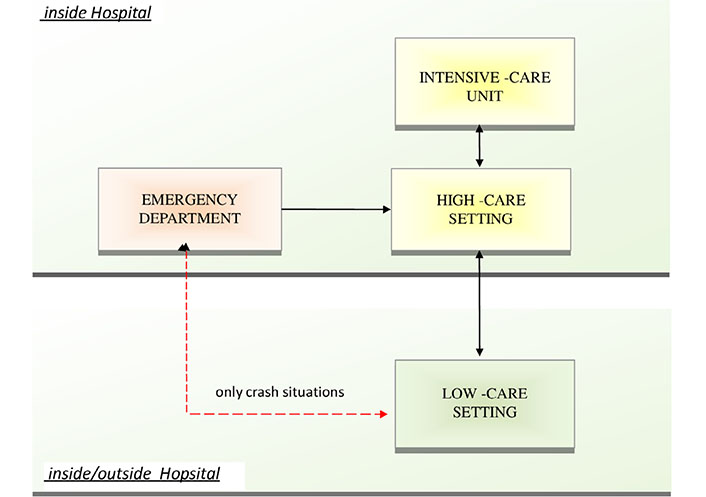
The role of low-care settings located inside or outside the main hospital (depending on the low or high incidence of COVID-19 cases, respectively), according to the concept of progressive patient care. The low-care setting should receive patients from high-care patients units in the early phase of remission. The admission of patients directly from the Emergency Department should be considered only in crash situations, to avoid returning patients to high-care settings due to worsening of clinical conditions
Moreover, the creation of a day hospital service inside Pegaso and the presence of allergists/immunologists experts in recognizing signs or symptoms of hypersensitivity reactions made possible the treatment of non-hospitalized patients with monoclonal antibodies directed against the spike protein of SARS-Cov2, a therapy that has been suggested as an option in preventing progression to severe COVID-19 infection in high-risk individuals and reducing hospitalizations. From May 2021 to April 2022, 281 outpatients with mild or moderate COVID-19 that did not require oxygen therapy or an increase in baseline oxygen flow rate, in those patients on chronic oxygen therapy, but were at high risk of progression to severe COVID-19, were treated at Pegaso day hospital service and the impact of this activity on main hospitals was completely eliminated. Finally, five outpatients with primary immunodeficiency and SARS-CoV-2 infection received their monthly dose of intravenous immunoglobulin inside the Pegaso day hospital service.
In conclusion, the role of the Pegaso low-care COVID center has been crucial in reducing the impact of the COVID-19 pandemic on the regional health system. There are certain lessons we can draw from our 16 months of experience at Pegaso. First, the strategic role of low-care settings in managing patients with COVID-19 disease in an early stage of remission, according to the concept of progressive patient care [2]. Second, the epidemiological suitability of low-care location: outside hospitals is a successful choice to preserve health system resistance during the high-pressure phases, whereas the creation of a low-care setting inside hospitals could be a better solution during low-pressure phases to optimize human and economic resources. It should be stressed that a strength of this experience has been the presence of a multi-specialist medical staff, with the opportunity for a continuous sharing and multidisciplinary discussion of each individual case. The experience of managing low-care settings with the day hospital service inside emphasizes, even more, the role of the allergists/immunologists during the COVID-19 pandemic contributing to keeping our specialty in a strategic role in the battle against this common enemy.
Abbreviations
| COVID-19: | coronavirus disease 2019 |
Declarations
Author contributions
LF: Conceptualization, Data Curation, Writing—original draft, Writing—review & editing. GL: Conceptualization, Writing—original draft, Validation. AF: Conceptualization, Writing—original draft, Writing—review & editing, Supervision, Validation. All authors contributed to manuscript revision, read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2023.