Abstract
Atopic dermatitis (AD) is a chronic inflammatory skin disease that primarily affects the barrier function of the skin in patients. The condition has been documented to cause xerosis in patients from birth onwards. In order to protect the skin barrier in AD, it is of the utmost importance to moisturize the skin. Moisturizers and emollients play a pivotal role in the prevention and treatment of AD. Concordantly, the use of moisturizers and emollients can facilitate the reduction in the necessity for the application of topical treatments such as corticosteroids. An understanding of the use of moisturizers and emollients, in conjunction with an appreciation of the pathophysiology of the skin barrier, will prove invaluable in the treatment of AD.
Keywords
Atopic dermatitis, moisturizer, emollient, treatmentIntroduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease presenting as xerosis, recurrent eczema, and severe pruritus [1]. It is one of the most prevalent diseases in pediatric populations, affecting 15–38% of children < 5-year-old globally. In adults, the prevalence ranges from 1.2% to 9.7% [2, 3]. Twenty-five percent of adults with AD have been reported to have an onset of the disease in adulthood, with similar prevalence across different countries. It is a possibility that the presence of AD in adulthood is a consequence of the disease having manifested at an early stage of development and subsequently resolved, and been forgotten [4].
The social burden of AD is evident in both children and adults. It has been documented that parents have observed both adults and children avoiding interaction with children diagnosed with AD. Furthermore, in adults, AD is believed to impair their social life and limit simple everyday activities, such as their choice of clothing, shaving, or wearing makeup [5]. The chronic itch, sleep deprivation, and stigmatization associated with AD can result in significant psychological distress for patients and their families [1]. Besides, the financial burden associated with AD encompasses a multitude of costs. These include prescriptions, physician visits, emergency room and hospital costs for patients and insurers alike, as well as over-the-counter pharmacy costs for patients. Moreover, indirect costs, like decreased work efficiency, absenteeism, and diminished quality of life of patients, contribute to the economic burden [5].
AD is caused by a combination of skin barrier dysfunction and T helper 2 (Th2) cell-mediated immunity [6]. The skin barrier serves to protect the skin against mechanical, chemical, and microbial traumas by reshaping terminally differentiated keratinocytes [7]. In AD, the impairment of the skin barrier is a vital factor in the pathogenesis, precipitating deterioration in the physical and functional shielding of the skin [8]. The dysfunction of the skin barrier results in the unregulated activation of proteases in the epidermis, which in turn leads to the production of Th2-type immune-inducing factors, such as thymic stromal lymphopoietin (TSLP) [6].
The Th2 immune response plays a fundamental role in the pathogenesis of AD. Specifically, the Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway is involved in the signaling of Th2 cytokines (IL-4, IL-13, and IL-31), which are essential for Th2-type immune responses. IL-4 and IL-13 have been demonstrated to down-regulate the levels of filaggrin (FLG), loricrin, and involucrin in keratinocytes, thereby exacerbating epidermal barrier dysfunction. Furthermore, IL-31 is another cytokine produced by Th2 cells whose levels have been found to be increased in both lesional and non-lesional skin of AD patients. As well as its pruritogenic function, IL-31 has been demonstrated to directly inhibit the differentiation of keratinocytes, leading to a disruption of epidermal barrier function. This effect appears to be mediated by the down-regulation of barrier/differentiation-related proteins [6, 9].
In addition to immune dysregulation, there are also defects in terminal epithelial differentiation, including lack of FLG, deficiencies in antimicrobial peptides, alterations in the composition of stratum corneum intercellular lipids, and changes in the skin microbiome [8]. FLG, a natural moisturizing component of the skin has a gene mutation in AD skin that results in barrier dysfunction [6]. Although it is well established that FLG mutation is a significant predisposing factor for AD development, specifically in patients with early-onset AD and those with persistent AD, recent studies have demonstrated that the isolation of FLG mutation is not sufficient to generate AD [8].
Given that the prevalence of eczema is significantly higher in children than in adults, it is of the utmost importance to prioritize this population [10]. Especially, the onset of dysfunction in the skin barrier occurs shortly after birth, presenting a potential avenue for the prevention of AD through the enhancement of the skin barrier, which may reduce inflammation from irritants and sensitization via the skin [11].
Moisturizers and emollients in the management of AD
Moisturizers represent a fundamental component of the therapeutic regimen for AD [12]. There is substantial evidence suggesting that the use of moisturizers can reduce the severity of AD and the need for pharmacologic intervention. Hence, moisturizers should be an integral part of the management of patients with AD [13].
Moisturizers comprise a number of different agents acting on the surface of the skin to prevent moisture loss and maintain the skin’s hydration. The occlusive agents form an airtight layer on the skin’s surface, while the emollients impart a soft and smooth texture. The humectants facilitate the stratum corneum’s ability to retain moisture. Furthermore, lipid components, such as ceramides, and barrier lipids, contribute to the moisturizer’s efficacy [14].
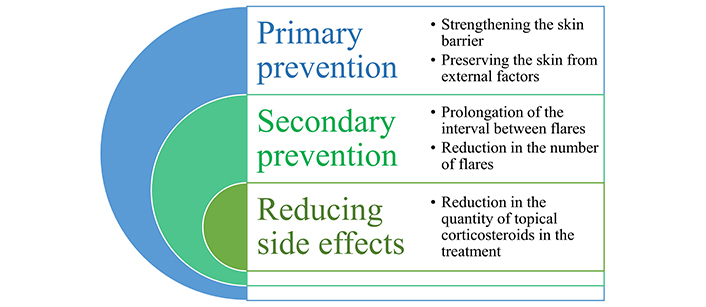
It is recommended that physicians continue to be the primary source of advice regarding the use of moisturizers [15]. The utilization of moisturizers in the treatment of AD is of significant benefit, as they provide relief from the clinical symptoms of the disease and enhance the functionality of the skin barrier. Additionally, they have been shown to reduce the colonization of bacteria [8]. The regular application of moisturizers containing a combination of emollients, humectants, and occlusive ingredients has been demonstrated to enhance barrier function and reduce the necessity for topical corticosteroid therapy in individuals with AD [12]. Moreover, moisturizers may facilitate the prolongation of the interval between flares and the reduction in the number of flares. For instance, in a study, the use of topical anti-inflammatory agents in conjunction with moisturizers has been shown to be more effective than the use of topical anti-inflammatory agents alone over a 6–8-week period (mean difference –9.30 g, 95% CI 15.3 to –3.27; I2 = 68%) [10].
The optimal moisturizer requires the correct emulsifiers in the appropriate quantity to enhance the skin barrier. Additionally, the composition of cholesterol, free fatty acids, and ceramides has been proposed as a means of maintaining an accurate lipid formulation. However, the precise composition and, in particular, the necessity of ceramides or even pseudo-ceramides remains a subject of debate [16].
An emollient is a component of a moisturizer [17]. The term “emollient” is frequently employed in conjunction with “moisturizer”, yet it is also utilized to delineate emulsifying ingredients within moisturizers, facilitating the product’s capacity to be readily applied [12, 18]. The primary function of an emollient is to act as an ingredient that fills the gaps in the stratum corneum, thereby imparting a soft feel to the skin. It should be noted that numerous emollients possess moisturizing properties [14]. They are composed of vehicle-type substances confering a protective physical barrier for the skin [16]. Emollients have been demonstrated to decrease trans epidermal water loss (TEWL), increase stratum corneum hydration, improve comfort, and reduce itch when applied to skin already affected by active eczema. In order to enhance the moisturizing efficacy of the emollients, a number of additional ingredients could be employed, including urea, glycerol, and propylene glycol. Consequently, emollients represent a significant component in the treatment of eczema [19, 20].
The studies have showed that the rate of skin absorption is elevated in both lesional and nonlesional AD skin in comparison to control skin, with a potential increase of more than twofold [21]. Therefore, emollient usage serves to reduce the quantity of topical treatment required, as topical corticosteroid absorption is diminished. On the other hand, the efficacy of emollients across the various stages of the disease, including acute, chronic, and interstitial flare periods, remains uncertain [10, 22]. It is not possible to state that all emollients are effective in alleviating the severity of disease when administered independently, whereas they are an appropriate sole treatment for mild or very mild eczema [10]. A multicenter, pragmatic, randomized controlled trial of high-risk infants has demonstrated that utilizing regular emollients for the first year of life does not result in the suspension, end, or control of eczema at age two years [23]. Another long-term follow-up study sets from an emollient for AD prevention trial documented AD and other atopic outcomes to 5 years. The findings suggest that there is no evidence to support the efficacy of regular daily emollient usage during the first year of life in reducing the risk of developing AD in the longer term [24]. Furthermore, it has been posited that the regular application of emollients during the first year of life does not confer protection against AD, food allergy, asthma, or hay fever [23, 24]. The aforementioned studies indicate that emollients may not be an adequate sole treatment for the first year of life in children with AD. Besides, in a separate study, the number of flares reported with moisturizers alone was greater than when combined with twice-weekly fluticasone propionate [10]. Although the evidence regarding the primary preventive effects of emollients is inconclusive during the first year of life, a daily treatment with emollients has been demonstrated to result in a reduction in the incidence of AD and allergic sensitizations in newborns at high risk of developing these conditions. Moreover, emollients play a crucial role in the prevention of eczema flares (secondary prevention) in AD. Experts continue to recommend the use of emollients in individuals at risk of developing AD during early childhood [20]. The application of moisturizers prior to the onset of eczema may offer a potential avenue for the primary prevention of eczema, as well. In the literature, studies have indicated that the application of moisturizers to infant skin may help to reduce in the prevalence of eczema during the application process [19].
It is recommended that patients with AD engage in regular bathing as a treatment and maintenance strategy. However, there is currently no standardized approach to the frequency or duration of bathing for those with AD. It is advised that non-soap cleansers, which are neutral to low pH, hypoallergenic and fragrance-free, are used with caution. The optimal cleansing product should provide cleansing dry, itchy skin, while also providing immediate and long-lasting hydration effectively [13, 25]. It is also advisable to ensure that the temperature of the water used is not excessively elevated. It is essential to clean the skin thoroughly and gently to remove any crusts, and to mechanically remove any bacterial contamination in the event of a superinfection [20]. Moisturizers and emollients should be applied promptly following bathing in order to enhance skin hydration in patients with AD. The application of moisturizers and emollients at this stage is particularly advantageous as the dermis is still slightly hydrated, thus providing the ideal opportunity to enhance the skin’s moisture retention [13, 20].
Accordingly, the results of studies indicate that the use of moisturizers and emollients is intended for the prevention of eczema, as well as for the treatment of the condition. Also, the use of moisturizers and emollients can facilitate the reduction of AD flares (Figure 1).
Formulations of moisturizers and emollients
The selection of a moisturizer and emollient is of paramount importance, given the variability in the clinical outcomes observed in patients [23]. The majority of parents and patients perceive an ideal moisturizer to be a fragrance-free, non-herbal, white or transparent cream applied two to three times per day [15].
Moisturizers contain varying concentrations of active ingredients such as humectants, occlusives and hydrophilic matrices, along with excipient ingredients like emulsifiers [19, 26]. Humectants, are substances capable of increasing the attraction and retention of water by the stratum corneum, which are frequently found in urea, glycerol, and lactic acid. Occlusives, forming a layer on the skin surface, are another category of moisturizer ingredients [17]. Occlusives encompass a range of hydrocarbons, such as petrolatum, mineral oil, paraffin, and squalene; silicones, such as dimethicone, cyclomethicone, and amodimethicone; and animal and vegetable fats, such as lanolin, shea butter, and grape seed oil. Examples of other oils include avocado oil, hemp oil, jojoba oil, sesame seed oil, and nut oil. Fatty acids like lanolin acid and stearic acid are also present. Additionally, occlusives comprise fatty and polyhydric alcohols such as lanolin alcohol, cetyl alcohol, propylene glycol, and butylene glycol. Furthermore, additional wax esters are present, including lanolin and beeswax, as well as stearyl stearate. Vegetable waxes, such as carnauba and candelilla, and phospholipids, such as lecithin, along with sterols, including cholesterol, serve as the other occlusive moisturizing ingredients [26]. The application of occlusive preparations may result in the formation of a semi-occlusive epidermal barrier, which serves to reinforce a naturally occurring barrier. This process prevents water loss and reduces the penetration of natural, and chemical allergens that pass through the skin [16]. The hydrophilic matrices in colloidal oatmeal form a physical protective coating over the skin, preventing evaporation [26]. In addition, oatmeal contains a number of constituents exhibiting beneficial effects on the skin, including moisturizing, soothing, anti-inflammatory, barrier-protective and antioxidant properties [27] (Table 1).
| Moisturizers and emollients | Components | Active ingredients | Effects |
|---|---|---|---|
| Moisturizers | Humectants | UreaGlycerin/glycerol | Enhancing the capacity of the stratum corneum to retain and attract water |
| Occlusive agents | Hydrocarbons (petrolatum, mineral oil, paraffin, squalene)Silicones (dimethicone, cyclomethicone, amodimethicone)Animal and vegetable fats (lanolin, shea butter, grape seed oil, avocado oil, hemp oil, jojoba oil, sesame seed oil, nut oil)Fatty acids (lanolin acid, stearic acid)Fatty and polyhydric alcohols (lanolin alcohol, cetyl alcohol, propylene glycol, butylene glycol)Wax esters (lanolin, beeswax, stearyl stearate)Vegetable waxes (carnauba, candelilla)Phospholipids (lecithin)Sterols (cholesterol) | Forming a semi-occlusive epidermal barrierInhibiting water lossLimiting the penetration allergens | |
| Hydrophilic matrices | Colloidal oatmeal | Forming a physical protective coating over the skinMoisturizingSoothingAnti-inflammatoryProtecting the skin barrierAntioxidant | |
| Emollients | Protective and fatting substances | Diisopropyl dilinoleateIsopropyl isostearateCastor oilPropylene glycolJojoba oilIsostearyl isostearateOctyl stearate | Forming a strong protective film on the skin surfaceProviding a slightly greasy thin layer with longer-lasting effect on the skinYielding soft and smooth texture of the skin |
Moisturizers can be classified as hydrophilic or lipophilic. Hydrophilic moisturizers are capable of attracting water and are therefore crucial for maintaining the hydration of the skin. In contrast, lipophilic moisturizers tend to remain on the surface of the skin, thereby assisting in the maintenance of the skin barrier [19]. The hydrophilic components of a product are of primary importance for skin hydration, whereas the lipophilic components serve the dual purpose of remaining on the surface of the skin as a barrier layer, preventing the evaporation of water and assisting in the recovery of the barrier function [17].
The role of lipids in the skin, particularly their capacity to regulate inflammation and the immune response, has recently been the subject of increased recognition. The concentration of intracellular lipids is diminished in lesional eczematous skin. It is possible that topically applied lipids may also enter the skin, thereby interfering with the bilayer lipids. For example, petrolatum is absorbed into the outermost layer of the delipidized stratum corneum, whereas more physiological lipids penetrate the skin and modify endogenous epidermal lipids, as well as the rate of barrier recovery [18, 19]. Additionally, petrolatum has been demonstrated to enhance skin barrier functions through the upregulation of antimicrobial peptides, including cathelicidin (LL-37), beta-defensins-2, elafin, and S100 proteins, and to significantly reduce T-cell, and dendritic cell infiltration [8]. A vegetable oil containing linoleic acid has been observed to alter the levels of ceramides present in the normal human stratum corneum. The diminished quantities of a specific ceramide identified in the stratum corneum during the winter months have been found to be replenished to levels comparable to those observed in the summer months. It has been postulated that polyunsaturated fatty acids present in oils containing omega-3 fatty acids may undergo enzymatic transformation by the epidermis into pertinent anti-inflammatory products [18].
Furthermore, moisturizers have been shown to induce the expression of epidermal differentiation markers, such as FLG and loricrin [8]. A moisturizer including urea and glycerol has been demonstrated barrier-strengthening effects, enhanced skin moisturization, and provided protection against irritation [22]. Another study has indicated that creams containing glycyrrhetinic acid, urea, and glycerol were more effective than their respective controls (vehicle, placebo, or no moisturizer) in both the participant, and physician evaluations [10].
Emollients soften the skin and make it smoother [17]. The emollients, including diisopropyl, dilinoleate and isopropyl isostearate, facilitate the formation of a robust protective film on the skin surface. The fatting emollients, comprising castor oil, propylene glycol, jojoba oil, isostearyl isostearate, and octyl stearate, facilitate the formation of a thin layer on the skin surface. This film is slightly greasy and has a longer-lasting effect [26] (Table 1).
The emollients may be enhanced by the incorporation of other ingredients, including moisturizers or tannin, ammonium bituminosulfonate, flavonoids, and unsaturated fatty acids, such as omega-3 or omega-6 compounds. Special ingredients, including ceramides and natural moisturizing factors (urea, pyrrolidone carboxylic acid, glutamic acid, and other amino acids), antimicrobial peptides, and ectoin, can also be used to enhance the emollient properties of a substance. Additionally, plant-derived substances, such as aloe vera, coconut oil, and animal-derived products, including lanolin and horse oil, represent further examples of the range of ingredients employed. These products contain putative active ingredients that do not meet the criteria for classification or licensing as topical drugs. However, they have been designated as “emollients plus” by the European guideline since 2018 [20, 28].
The term “prescription emollient devices” (PED) has recently been introduced in the literature. These are a class of topical agents developed to “target specific defects in skin barrier function” in individuals with eczema. The PEDs are formulated with a combination of a variety of lipid, ceramide, fatty acid, and natural anti-inflammatory agent mixtures, and ratios, including glycyrrhetinic acid, as well as additional ingredients designed to alleviate itching and inflammation [13, 17].
Conclusions
The use of moisturizers and emollients is an effective treatment option for individuals with AD by preventing, alleviating the condition through the maintenance of skin hydration and protection from moisture loss. Considering the potential adverse effects of topical corticosteroids such as skin thinning and atrophy, the application of moisturizers and emollients serves to reinforce the protective barrier function of the skin, thereby offering both prophylactic and therapeutic benefits. Moisturizers and emollients function to mitigate the desiccation of the dermis, diminish the rate of TEWL, enhance comfort, and alleviate pruritus. It is evident that the moisturization of the skin, which constitutes a primary and secondary form of prevention, is an efficient method for controlling AD. Further development of moisturizers and emollients with additional investigation into the optimal ratios of different ingredient combinations, and the long-term effects of their use in future research will help to provide greater efficacy in the treatment of AD.
Abbreviations
| AD: | atopic dermatitis |
| FLG: | filaggrin |
| Th2: | T helper 2 |
Declarations
Author contributions
SM: Conceptualization, Investigation, Writing—original draft, Writing—review & editing, Validation, Supervision. The author read and approved the submitted version.
Conflicts of interest
The author declares that she has no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2024.