Affiliation:
1Allergy Unit, Angers University Hospital, 49933 Angers, France
Email: louise_guyot@chu-angers.fr
ORCID: https://orcid.org/0000-0003-0038-7607
Affiliation:
2Angers University, Nantes University, Angers University Hospital, Inserm, CRCINA, SFR ICAT, F-49000 Angers, France
ORCID: https://orcid.org/0000-0002-6987-3120
Affiliation:
4Regional Pharmacovigilance Center, Angers University Hospital, 49933 Angers, France
ORCID: https://orcid.org/0000-0003-4103-7558
Affiliation:
1Allergy Unit, Angers University Hospital, 49933 Angers, France
ORCID: https://orcid.org/0000-0002-4028-703X
Explor Asthma Allergy. 2025;3:100970 DOI: https://doi.org/10.37349/eaa.2025.100970
Received: October 11, 2024 Accepted: December 25, 2024 Published: January 23, 2025
Academic Editor: Umit Murat Sahiner, Hacettepe University Faculty of Medicine, Turkey
Gelatin is extracted from beef, pork, and fish tissues. An increasing number of cases of gelatin-induced anaphylaxis are associated with α-Gal syndrome (AGS). Only a few cases of anaphylaxis to bovine gelatin (BG) without AGS (BG-woAG) have been described. We report two new cases of anaphylaxis to BG-woAG, highlight the characteristics of this entity, and propose a procedure in cases of suspected anaphylaxis to BG. We selected articles on gelatin allergy between 1987 and 2024. Results: we report two new cases of severe anaphylaxis BG-woAG. Diagnosis was established using skin tests (ST), IgE, and basophil activation tests (BAT). We confirm the existence of allergies to BG-woAG. The main characteristic of these allergies seems to be the presence of BG IgE which differentiates them from AGS-related allergies. These initial data need to be confirmed by larger case series. We propose a diagnostic algorithm for better patient management. To confirm the diagnosis, ST and IgE to BG and α-Gal should be performed. The role of BAT to Gelofusine® in the diagnostic strategy remains to be defined.
Gelatin is extracted from the connective tissues of cows, pigs, and fish for uses based on its adhesive and gelling properties [1]. Mammalian gelatin is used as a substitute for colloidal plasma, a stabilizer in vaccines, a component of hemostatic and erythropoietin-based products, in glues, and in the food industry [2].
Galactose-alpha-1,3-galactose (α-Gal) is a glycosylated determinant expressed on non-primate mammalian proteins and lipids. A condition known as α-Gal syndrome (AGS) was initially described in patients suffering anaphylaxis after the ingestion of mammalian meat or the injection of cetuximab [3]. In 2012, Mullins et al. [2] demonstrated a link between gelatin allergy and α-Gal IgE antibodies and estimated the amount of α-Gal in Gelofusine® (0.52 µg/g).
However, it remains unclear whether patients with gelatin allergy systematically display AGS. Only a handful of cases of anaphylaxis in response to bovine gelatin (BG) without AGS (BG-woAG) have been described to date. We report two new cases of BG-woAG here. We highlight the characteristics of this entity and propose a procedure to be followed in cases of suspected anaphylaxis following intravenous (IV) exposure to BG.
Clinical severity was assessed and skin tests (ST) were performed in accordance with EAACI recommendations. Patients underwent prick tests (PT) and intradermal tests (IDT) with modified BG (Gelofusine®) at doses of up to 40 mg/mL, as described in previous studies [2, 3]. Tryptase levels were determined and a basophil activation test (BAT) was performed when possible. Specific IgE measurements were performed with ImmunoCAP® (see the Supplementary material for details).
First case: a 66-year-old man with no history of allergy was referred for grade 3 anaphylaxis during aortic valve replacement. A few minutes after the Gelofusine® infusion, the patient presented sudden hypotension, which resolved following the IV injection of epinephrine. There were no other signs of anaphylaxis. Tryptase determination revealed mast cell degranulation.
Allergological investigations were performed and a positive IDT result was obtained for Gelofusine® (Table 1). PT and IDT were negative for all other drugs administered before the allergic reaction, cetuximab and fish gelatin (FG). Weakly positive results were obtained for specific IgEs against pork and beef and negative results were obtained for specific IgEs against α-Gal thyroglobulin. A BAT was positive for Gelofusine® and negative for α-Gal (Figure S1).
Allergological investigations in patients 1 and 2
| Studied parameters | Patient 1 | Patient 2 |
|---|---|---|
| Tryptase (µg·L–1) | ||
| Tryptase during the crisis (time) | 10.3 (0.5 h)10.9 (2 h) | 152 (12 h) |
| Tryptase basal | 2.27 (24 h) | 20.5 (24 h)15.1 (several weeks later) |
| Prick test | ||
| Gelofusine® | Negative up to 40 mg·mL–1 | Positive at 4 mg·mL–1 |
| Porcine gelatin (undiluted) | ND | Positive |
| Fish gelatin (undiluted) | Negative | ND |
| Intradermal test (IDT) | ||
| Gelofusine® | Positive at 40 mg·mL–1 (4–9/10)* | Positive at 0.04 mg·mL–1 (4–8/20)* |
| Cetuximab | Negative up to 0.5 mg·mL–1 | ND |
| IgE (ImmunoCap® Phadia) kUA/L | ||
| Bovine gelatin | < 0.10 | > 100 |
| Bovine α-Gal thyroglobulin | < 0.10 | 0.39 |
| Pork | 0.20 | < 0.10 |
| Beef | 0.59 | 0.23 |
| BAT (Flow Cast, Bühlmann) | ||
| Gelofusine® | Positive | Positive |
| α-Gal | Negative | Negative |
| Cetuximab | ND | Negative |
| Beef meat | ND | Negative |
ND: not done; BAT: basophil activation tests; α-Gal: galactose-alpha-1,3-galactose *: a–b/c (a: initial diameter of the IDT papule; b: diameter of the IDT papule after 20 min; c: diameter of the IDT erythema after 20 min)
Second case: a 64-year-old man was referred for grade 4 anaphylaxis during coronary angiography. Five minutes after the Gelofusine® injection, he presented a cutaneous rash and four episodes of cardiorespiratory arrests with a favorable outcome. Tryptase determination revealed mast cell degranulation.
A PT with native pig gelatin (PG) and an IDT with Gelofusine® yielded positive results. PT for mammalian meats and pig kidney were negative. ImmunoCap® confirmed strong IgE reactivity to BG. No IgEs specific to pork were detected and a weakly positive result was obtained for the detection of IgEs specific to beef and bovine thyroglobulin. The BAT was positive for BG and negative for cetuximab, beef, and α-Gal (Table 1 and Figure S1).
We reviewed all the articles studied with the keywords gelatin, collagen, colloid, allergy, anaphylaxis, α-Gal, and/or AGS. We selected cases of BG-woAG occurring from 2009 (AGS discovery) to 2024 for which diagnostic data were available.
Both the cases described here presented IgE-mediated allergy to Gelofusine® without AGS. Both patients were used to eating all meats and offal from mammalian sources with no reaction and an absence of IgE reactivity to α-Gal determinants was demonstrated by the negative BAT result for α-Gal and/or negative IDT or BAT result for cetuximab. No IgEs specific for α-Gal were detected in the first case and a weakly positive result was obtained in the second. This weak IgE reactivity to α-Gal may be related to an IgE binding to other bovine thyroglobulin components. We did not perform an oral challenge in either of these patients for ethical reasons, due to the severity of the anaphylaxis observed and comorbid conditions. Both patients were treated with gelatin-containing capsules and both were meat-eaters. They may therefore have been sensitized through food or medication, but it was not possible to demonstrate this conclusively.
Positive BAT results for Gelofusine® have already been reported based on CD63 expression. Apostolou evaluated the performance of BAT in six cases of Gelofusine® anaphylaxis and reported a sensitivity of 100% and a specificity of 87.5% [3, 4]. Our results suggest that BAT is a safe and reliable tool for diagnosing BG anaphylaxis, particularly when Gelofusine® ST is unreliable.
According to the 11th GERAP epidemiological survey, gelatin allergy accounted for 0.15% of anaphylaxis events occurring under anesthesia in France between 2017 and 2018 [5].
Anaphylaxis in response to gelatin may be linked to denatured collagen peptides, mediated by an IgE binding to the α2 chain of type I collagen [6]. However, anaphylaxis in response to IV BG has recently most frequently been linked to the IgE-mediated recognition of a glycosylated component, such as α-Gal [3].
An analysis of the French National Pharmacovigilance database revealed 3,000 cases of anaphylaxis in response to gelatin (data as of July 2022). BG was the only suspected product in approximately 100 cases and allergies to BG-woAG were suspected in fewer than 10 patients.
Eight cases of allergy to BG-woAG have been reported to date. Molina-Molina et al. [7] described a case of fatal anaphylaxis in response to IV BG with positive results for IgE specific for BG and no IgE reactivity to α-Gal. In a series of patients with allergies to meat and/or mammalian gelatin, Ebo et al. [1] described an allergic reaction following the ingestion of a marshmallow containing gelatin in one patient. This patient tested negative for IgE against α-Gal and positive for IgE against BG, whereas the other patients positive for IgE against α-Gal tested negative for IgE against BG [1]. Retterer et al. [8] described a case of anaphylactic reaction following anti-shingles vaccination due to gelatin allergy in a patient allergic to mean. This patient tested negative for IgE against α-Gal but positive for IgE against pork and BG [8]. Grade IV anaphylaxis was reported in another patient following the administration of Gelafundin®, with a positive PT for Gelafundine® and the detection of IgE against BG, but negative results for IgE against α-Gal [9]. The other four cases were reported by Bradfisch et al. [10]. They occurred after rabies vaccination and were attributed to gelatin allergy. All these patients tested positive for IgE against BG but all tested negative for IgE against α-Gal. Three patients underwent ST with gelatin and positive results were obtained for all three. One patient developed generalized urticaria after IDT [10].
Two of these cases had previously received modified IV BG with no reaction (6 months and 10 days previously), which may have triggered primary sensitization. The diagnosis was based on negative results for IgE against α-Gal and positive results for IgE against BG (no BAT was reported). All STs performed with IV BG were positive.
Mullins et al. [2] studied the link between red meat allergy and sensitization to gelatin and AGS. They found that 75% of patients allergic to red meat had positive IDT results for BG and that 83–88% of their series of patients with AGS and positive oral challenge results with pork kidney, IDT with Gelafundin® yielded positive results [11].
A literature review identified 37 cases of AGS in which anti-BG IgE levels were reported. In all but one case, positive results were obtained for IgE against α-Gal whereas negative results were obtained for IgE against BG. In the remaining case, a weakly positive result for IgE against BG (0.42 kIU/L) was obtained in the Mullins et al. [2] series. Conversely, all patients allergic to IV BG with no detectable IgE against α-Gal had positive results for IgE against BG, with the exception of one of our patients. Negative results for IgE against BG appear to be a feature of AGS, whereas most patients displaying BG-woAG have positive IgE ImmunoCAP® results for BG. This anti-BG IgE assay cannot, therefore, be used to rule out BG allergy.
Oral challenge should be considered in cases of anaphylaxis in response to IV gelatin, as anaphylactic reactions have been reported following the ingestion of mammalian gelatin [1]. Gelatin is not a food allergen for which labeling in foods is mandatory. It is therefore difficult to ensure that the diet is gelatin-free. In a series of cases of anaphylaxis due to gelatin-containing vaccines, 27% of the cases experienced grade I or II anaphylaxis after the ingestion of gelatin [12].
Cross-reactivity between different sources of gelatin and collagen has not yet been studied. According to Bogdanovic et al. [13], IgE against BG displays strong cross-reactivity with PG and limited cross-reactivity with FG.
Fujimoto et al. [6] reported grade II anaphylaxis following the consumption of a dietary supplement and jelly sweets containing fish collagen. Positive PT results were obtained for both these products and FG. IgE reactivity to FG and BG has also been demonstrated, together with the possible binding of IgE to the α chain of type I collagen [6]. Patients allergic to BG should be systematically tested for allergy to FG. There is currently no commercial kit for the detection of IgE against FG.
This study, based on case reports and a literature review, confirms the existence of allergies to BG in the absence of AGS. These allergies have a specific profile, with detectable anti-BG IgE antibodies (detected in the ImmunoCAP® assay), differentiating them from AGS-related allergies. These initial data require confirmation in a larger case series.
Our case reports are the first to combine ST, IgE, and positive BAT results. We propose a diagnostic algorithm for improving patient management (Figure 1). For confirmation of the diagnosis, ST should be performed, with determinations of IgE against BG and α-Gal. In cases of proven allergy to BG, an oral challenge should be proposed, together with a PT for FG. The contribution of BAT with Gelofusine® to the diagnostic strategy remains to be defined.
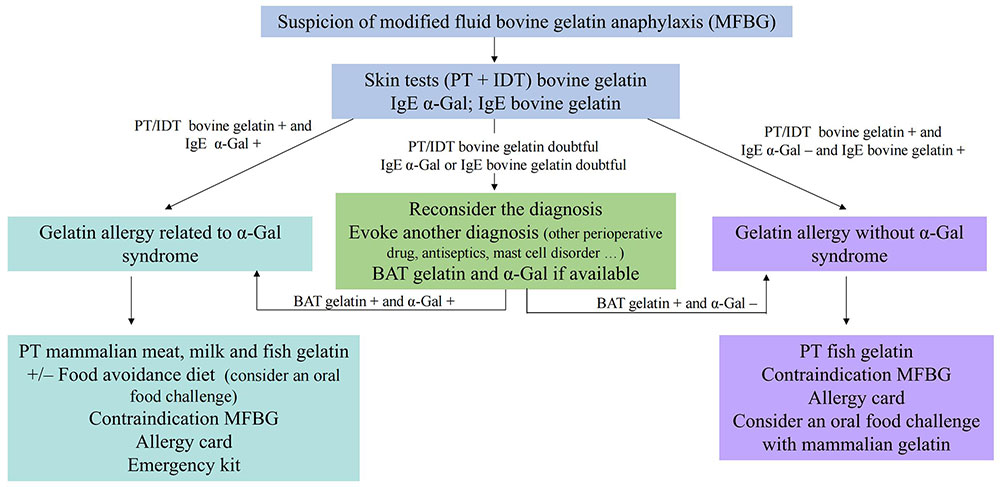
Diagnostic algorithm for suspected allergy to bovine gelatin. +: positive; –: negative; α-Gal: galactose-alpha-1,3-galactose; PT: prick tests; IDT: intradermal tests; BAT: basophil activation tests
AGS: galactose-alpha-1,3-galactose syndrome
BAT: basophil activation tests
BG: bovine gelatin
BG-woAG: bovine gelatin without galactose-alpha-1,3-galactose
FG: fish gelatin
IDT: intradermal tests
IV: intravenous
PG: pig gelatin
PT: prick tests
ST: skin tests
α-Gal: galactose-alpha-1,3-galactose
The supplementary figures for this article are available at: https://www.explorationpub.com/uploads/Article/file/100970_sup_1.pdf.
LG and MM: Conceptualization, Methodology, Resources, Data curation, Writing—review & editing, Writing —original draft. CB, VL, DBM: Conceptualization, Methodology, Resources, Data curation, Writing—review & editing. All the authors have read and approved the final manuscript.
The authors declare that there are no conflicts of interest.
Ethics approval from our institution (Angers University Hospital) was not required for a study of this type.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
Datasets are available from the corresponding authors upon reasonable request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 4766
Download: 31
Times Cited: 0
