-
Exploration of Cardiology
eISSN: 2994-5526EiC: Eugenio Picano, ItalyFrequency: Continuous PublicationAPC: No Article Processing Charge before Jul 31, 2028Publishing Model: Open AccessPeer Review Model: Single BlindPermanent Archive: PorticoIndexing & Archiving: Google Scholar, Dimensions, MyScienceWork, Portico, etc.Articles Age-related atrial fibrillation: is there a role for the gut microbiome?Open AccessReviewAge-related atrial fibrillation (AF) is a common condition that has yet to be fully understood, with mechanisms to explain its development under investigation. Notably, cellular senescence, cardiac [...] Read more.
Age-related atrial fibrillation: is there a role for the gut microbiome?Open AccessReviewAge-related atrial fibrillation (AF) is a common condition that has yet to be fully understood, with mechanisms to explain its development under investigation. Notably, cellular senescence, cardiac [...] Read more.Age-related atrial fibrillation (AF) is a common condition that has yet to be fully understood, with mechanisms to explain its development under investigation. Notably, cellular senescence, cardiac fibrosis, coronary ischemia, cardiac valvular disease, autonomic dysfunction, channelopathies, and immune system remodeling are processes that have been seen to occur with aging and ample evidence has shown their association with the development of AF. Despite robust therapeutic approaches, the incidence of AF continues to rise, suggesting that the dynamic, multi-faceted interactions leading to AF are incompletely understood. One of the newer mechanisms currently being investigated is the gut microbiome. Although more research is needed to understand its impact on the development of age-related AF and targets for therapies, the gut microbiome is a promising new avenue of research that may provide future benefits in AF prophylaxis or enhanced management. As the field works towards developing this knowledge, there are important questions to answer as to the optimal role of potential gut microbiome targeting therapies and their potential risks versus the benefits they provide. This commentary first summarizes the currently understood mechanisms contributing to age-related AF, which is then followed by an analysis of the current work investigating the role of the gut microbiome in the development of age-related AF, and concludes by highlighting notable questions to consider in future work on the role of the gut microbiome and its relationship to age-related AF.
Michael Li ... Robert M. LustPublished: March 24, 2025 Explor Cardiol. 2025;3:101251
DOI: https://doi.org/10.37349/ec.2025.101251
This article belongs to the special issue Molecular Mechanisms of Cardiovascular AgingAge-related atrial fibrillation (AF) is a common condition that has yet to be fully understood, with mechanisms to explain its development under investigation. Notably, cellular senescence, cardiac fibrosis, coronary ischemia, cardiac valvular disease, autonomic dysfunction, channelopathies, and immune system remodeling are processes that have been seen to occur with aging and ample evidence has shown their association with the development of AF. Despite robust therapeutic approaches, the incidence of AF continues to rise, suggesting that the dynamic, multi-faceted interactions leading to AF are incompletely understood. One of the newer mechanisms currently being investigated is the gut microbiome. Although more research is needed to understand its impact on the development of age-related AF and targets for therapies, the gut microbiome is a promising new avenue of research that may provide future benefits in AF prophylaxis or enhanced management. As the field works towards developing this knowledge, there are important questions to answer as to the optimal role of potential gut microbiome targeting therapies and their potential risks versus the benefits they provide. This commentary first summarizes the currently understood mechanisms contributing to age-related AF, which is then followed by an analysis of the current work investigating the role of the gut microbiome in the development of age-related AF, and concludes by highlighting notable questions to consider in future work on the role of the gut microbiome and its relationship to age-related AF.
 Comparison of short-term and long-term effects of peroral L-carnitine intake: clinical implications of elevated TMAO levels in cardiovascular complicationsOpen AccessReviewL-Carnitine (LC) is integral to energy production and fatty acid metabolism, facilitating the transport of long-chain fatty acids into mitochondria for β-oxidation. It modulates metabolic pathway [...] Read more.
Comparison of short-term and long-term effects of peroral L-carnitine intake: clinical implications of elevated TMAO levels in cardiovascular complicationsOpen AccessReviewL-Carnitine (LC) is integral to energy production and fatty acid metabolism, facilitating the transport of long-chain fatty acids into mitochondria for β-oxidation. It modulates metabolic pathway [...] Read more.L-Carnitine (LC) is integral to energy production and fatty acid metabolism, facilitating the transport of long-chain fatty acids into mitochondria for β-oxidation. It modulates metabolic pathways, including pyruvate dehydrogenase activity, proteolysis, and protein synthesis, while also having anti-inflammatory and antioxidant characteristics. LC can be commonly applied to win the battle against HIV and cancer cachexia. Also, it can be recruited with the aim of improving physical and cognitive functions in athletes and the elderly. Despite these benefits, long-term LC administration has been associated to cardiovascular risks due its conversion to trimethylamine-N-oxide (TMAO) by the gut microbiota. Elevated TMAO levels are linked to atherosclerosis, oxidative stress, and an increased risk of cardiovascular disease, diabetes, and chronic kidney disease. Managing TMAO levels using dietary treatments and gut microbiota-targeting techniques, such as probiotics, may reduce these risks. This comprehensive review presents the state-of-the-art information on LC’s dual role, emphasizing the balance between its therapeutic potential and the risks of prolonged supplementation. It aims to guide clinicians and researchers in optimizing LC’s benefits while addressing its long term cardiovascular safety concerns.
Harsahaj Singh Wilkhoo ... Adnan Akhtar ShaikhPublished: February 10, 2025 Explor Cardiol. 2025;3:101250
DOI: https://doi.org/10.37349/ec.2025.101250L-Carnitine (LC) is integral to energy production and fatty acid metabolism, facilitating the transport of long-chain fatty acids into mitochondria for β-oxidation. It modulates metabolic pathways, including pyruvate dehydrogenase activity, proteolysis, and protein synthesis, while also having anti-inflammatory and antioxidant characteristics. LC can be commonly applied to win the battle against HIV and cancer cachexia. Also, it can be recruited with the aim of improving physical and cognitive functions in athletes and the elderly. Despite these benefits, long-term LC administration has been associated to cardiovascular risks due its conversion to trimethylamine-N-oxide (TMAO) by the gut microbiota. Elevated TMAO levels are linked to atherosclerosis, oxidative stress, and an increased risk of cardiovascular disease, diabetes, and chronic kidney disease. Managing TMAO levels using dietary treatments and gut microbiota-targeting techniques, such as probiotics, may reduce these risks. This comprehensive review presents the state-of-the-art information on LC’s dual role, emphasizing the balance between its therapeutic potential and the risks of prolonged supplementation. It aims to guide clinicians and researchers in optimizing LC’s benefits while addressing its long term cardiovascular safety concerns.
 Extubation of patients with COVID-19 acute respiratory failure during extracorporeal membrane oxygenation support is associated with improved survivalOpen AccessOriginal ArticleAim: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, infection resulting in acute respiratory distress syndrome (ARDS) requiring veno-venous or veno-arterial extracorpo [...] Read more.
Extubation of patients with COVID-19 acute respiratory failure during extracorporeal membrane oxygenation support is associated with improved survivalOpen AccessOriginal ArticleAim: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, infection resulting in acute respiratory distress syndrome (ARDS) requiring veno-venous or veno-arterial extracorpo [...] Read more.Aim:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, infection resulting in acute respiratory distress syndrome (ARDS) requiring veno-venous or veno-arterial extracorporeal membrane oxygenation (VV or VA-ECMO) support is a life-threatening disease process that requires prolonged intubation and has a high risk of mortality.
Methods:
In this retrospective, observational, single-center cohort study, we attempt to better understand the role of extubation in the course of treatment by dichotomizing groups into those extubated early while remaining on ECMO treatment (group A), compared to patients who remained intubated for the entirety of their ECMO treatment (group B).
Results:
The data indicate that early extubation of patients with COVID-19-associated ARDS requiring ECMO support leads to improved survival rates for group A (93%) compared to prolonged intubation (group B) throughout the course of ECMO therapy (64%) (p = 0.13). Additionally, patients extubated earlier (19 days vs. 59 days; p = 0.012) required significantly fewer vasoactive drugs (norepinephrine dosing: 0.03 mcg/kg/min vs. 0.093 mcg/kg/min; p = 0.04), and were less likely to require a tracheostomy (0 vs. 4, p = 0.026).
Conclusions:
Although the utility of ECMO in severe ARDS patients remains a contentious topic, early extubation seems to increase survival rates and overall patient outcomes in patients with COVID-19-associated ARDS requiring ECMO support.
Sean Kelleher ... Amit PrasadPublished: February 05, 2025 Explor Cardiol. 2025;3:101249
DOI: https://doi.org/10.37349/ec.2025.101249Aim:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, infection resulting in acute respiratory distress syndrome (ARDS) requiring veno-venous or veno-arterial extracorporeal membrane oxygenation (VV or VA-ECMO) support is a life-threatening disease process that requires prolonged intubation and has a high risk of mortality.
Methods:
In this retrospective, observational, single-center cohort study, we attempt to better understand the role of extubation in the course of treatment by dichotomizing groups into those extubated early while remaining on ECMO treatment (group A), compared to patients who remained intubated for the entirety of their ECMO treatment (group B).
Results:
The data indicate that early extubation of patients with COVID-19-associated ARDS requiring ECMO support leads to improved survival rates for group A (93%) compared to prolonged intubation (group B) throughout the course of ECMO therapy (64%) (p = 0.13). Additionally, patients extubated earlier (19 days vs. 59 days; p = 0.012) required significantly fewer vasoactive drugs (norepinephrine dosing: 0.03 mcg/kg/min vs. 0.093 mcg/kg/min; p = 0.04), and were less likely to require a tracheostomy (0 vs. 4, p = 0.026).
Conclusions:
Although the utility of ECMO in severe ARDS patients remains a contentious topic, early extubation seems to increase survival rates and overall patient outcomes in patients with COVID-19-associated ARDS requiring ECMO support.
 Who is a reviewer? The Good, the Bad, and the Ugly phenotypesOpen AccessEditorialBy offering their expertise, reviewers help authors improve their work and also support editors in selecting high-quality studies, thereby reinforcing the integrity of scientific literature. Much li [...] Read more.
Who is a reviewer? The Good, the Bad, and the Ugly phenotypesOpen AccessEditorialBy offering their expertise, reviewers help authors improve their work and also support editors in selecting high-quality studies, thereby reinforcing the integrity of scientific literature. Much li [...] Read more.By offering their expertise, reviewers help authors improve their work and also support editors in selecting high-quality studies, thereby reinforcing the integrity of scientific literature. Much like in a Sergio Leone film, your manuscript encounters three possible types of reviewers on its editorial journey: the Good, the Bad, and the Ugly. The Good Reviewer is, for reasons unknown, favorably disposed toward both you and your manuscript. They find it “well-written, with literary and enjoyable style”, “original and timely”, and addressing a topic that is “scientifically and socially relevant”. Their comments are respectful, constructive, and focused on minor but meaningful improvements. Unfortunately, the Good Reviewer is as rare as a white unicorn; some researchers reach the end of their careers without ever encountering one, leading them to question their very existence. The Bad Reviewer is both bad at reviewing and a bad influence on your work. They reject your manuscript, but their reasons are vague and unconvincing. Their objections are often asinine, and when you respond thoroughly and decisively, they counter with even more nonsensical arguments. They may pressure you to cite irrelevant literature—often their work or that of their colleagues. In the end, your once-solid and cohesive manuscript emerges in a far worse state than the original. None of this would have been possible without the Bad Reviewer, who, unleashed by a negligent editor, exerts their detrimental influence on your article. The Ugly Reviewer appears with unsettling regularity—at least once a month. They believe your article is truly terrible, and often, they are right. The Ugly Reviewer, though harsh, is no fool. Their critiques are brutal and unforgiving, yet accurate. Years later, you may find yourself grateful to them for preventing you from publishing work that, in hindsight, would have irreparably tarnished your already modest scientific reputation.
Eugenio PicanoPublished: January 23, 2025 Explor Cardiol. 2025;3:101248
DOI: https://doi.org/10.37349/ec.2025.101248By offering their expertise, reviewers help authors improve their work and also support editors in selecting high-quality studies, thereby reinforcing the integrity of scientific literature. Much like in a Sergio Leone film, your manuscript encounters three possible types of reviewers on its editorial journey: the Good, the Bad, and the Ugly. The Good Reviewer is, for reasons unknown, favorably disposed toward both you and your manuscript. They find it “well-written, with literary and enjoyable style”, “original and timely”, and addressing a topic that is “scientifically and socially relevant”. Their comments are respectful, constructive, and focused on minor but meaningful improvements. Unfortunately, the Good Reviewer is as rare as a white unicorn; some researchers reach the end of their careers without ever encountering one, leading them to question their very existence. The Bad Reviewer is both bad at reviewing and a bad influence on your work. They reject your manuscript, but their reasons are vague and unconvincing. Their objections are often asinine, and when you respond thoroughly and decisively, they counter with even more nonsensical arguments. They may pressure you to cite irrelevant literature—often their work or that of their colleagues. In the end, your once-solid and cohesive manuscript emerges in a far worse state than the original. None of this would have been possible without the Bad Reviewer, who, unleashed by a negligent editor, exerts their detrimental influence on your article. The Ugly Reviewer appears with unsettling regularity—at least once a month. They believe your article is truly terrible, and often, they are right. The Ugly Reviewer, though harsh, is no fool. Their critiques are brutal and unforgiving, yet accurate. Years later, you may find yourself grateful to them for preventing you from publishing work that, in hindsight, would have irreparably tarnished your already modest scientific reputation.
 Association between a specific monocyte subset and heart failure with preserved ejection fraction in patients with uremiaOpen AccessOriginal ArticleAim: This study aimed to establish a model based on gene expression in peripheral blood mononuclear cells (PBMCs) for predicting the incidence of heart failure with preserved ejection fraction (H [...] Read more.
Association between a specific monocyte subset and heart failure with preserved ejection fraction in patients with uremiaOpen AccessOriginal ArticleAim: This study aimed to establish a model based on gene expression in peripheral blood mononuclear cells (PBMCs) for predicting the incidence of heart failure with preserved ejection fraction (H [...] Read more.Aim:
This study aimed to establish a model based on gene expression in peripheral blood mononuclear cells (PBMCs) for predicting the incidence of heart failure with preserved ejection fraction (HFpEF) in patients with end-stage renal disease (ESRD).
Methods:
PBMCs were isolated from patients with stage 2–3 chronic kidney disease, ESRD, ESRD with HFpEF, and ESRD with heart failure with reduced ejection fraction (HFrEF). Differences in the expression of differentially expressed genes in PBMCs among different groups were compared using microarray.
Results:
In total, 43 differentially expressed genes were specifically identified in patients with ESRD with HFpEF. The expression of four genes encoding MMP7, S100A8, CXCR3, and CD163 was significantly upregulated. Hence, it played a role in the development of HFpEF. Based on these findings, a nomogram was established using data from the database including 343 patients with ESRD. The receiver operating characteristic curve, calibration curve, model consistency index, and decision curve analyses showed that the nomogram had a good predictive performance for predicting HFpEF.
Conclusions:
Specific gene detections can be an important early warning indicator and guide physicians in evaluating the risk of HFpEF in ESRD.
Xinrui Wang ... Yang YangPublished: January 20, 2025 Explor Cardiol. 2025;3:101247
DOI: https://doi.org/10.37349/ec.2025.101247Aim:
This study aimed to establish a model based on gene expression in peripheral blood mononuclear cells (PBMCs) for predicting the incidence of heart failure with preserved ejection fraction (HFpEF) in patients with end-stage renal disease (ESRD).
Methods:
PBMCs were isolated from patients with stage 2–3 chronic kidney disease, ESRD, ESRD with HFpEF, and ESRD with heart failure with reduced ejection fraction (HFrEF). Differences in the expression of differentially expressed genes in PBMCs among different groups were compared using microarray.
Results:
In total, 43 differentially expressed genes were specifically identified in patients with ESRD with HFpEF. The expression of four genes encoding MMP7, S100A8, CXCR3, and CD163 was significantly upregulated. Hence, it played a role in the development of HFpEF. Based on these findings, a nomogram was established using data from the database including 343 patients with ESRD. The receiver operating characteristic curve, calibration curve, model consistency index, and decision curve analyses showed that the nomogram had a good predictive performance for predicting HFpEF.
Conclusions:
Specific gene detections can be an important early warning indicator and guide physicians in evaluating the risk of HFpEF in ESRD.
 Oxidized low-density lipoproteins and their contribution to atherosclerosisOpen AccessReviewThe oxidation of lipoproteins has a key role in the development of atherosclerosis, a condition where plaque builds up in artery walls. Research shows that when low-density lipoprotein (LDL) oxidize [...] Read more.
Oxidized low-density lipoproteins and their contribution to atherosclerosisOpen AccessReviewThe oxidation of lipoproteins has a key role in the development of atherosclerosis, a condition where plaque builds up in artery walls. Research shows that when low-density lipoprotein (LDL) oxidize [...] Read more.The oxidation of lipoproteins has a key role in the development of atherosclerosis, a condition where plaque builds up in artery walls. Research shows that when low-density lipoprotein (LDL) oxidizes, it speeds up atherosclerosis. Oxidized LDL (Ox-LDL) causes many pathologic scenarios that lead to atherosclerosis. It was suggested as a fundamental player in endothelial dysfunction, creating foam cells, and triggering inflammation in artery walls. How Ox-LDL contributes and interacts with specific receptors on endothelial cells is crucial to these effects. This article aims to shed light on LDL oxidation, the stages of the process, and how Ox-LDL promotes atherosclerosis. A comprehensive search was conducted across various databases, including PubMed, Google Scholar, Scopus, and Ovid, to identify literature and studies that discuss Ox-LDL and their involvement in the pathogenesis of atherosclerosis and cardiovascular diseases, thereby establishing a well-defined perspective on the subject. This review will provide a closer look at the Ox-LDL particle, the different forms and stages of oxidation, and the role of various LDL receptors involved in LDL uptake and breakdown focusing on how they contribute to atherosclerosis. Then, it will discuss the role of scavenger receptors and their contribution to the uptake of Ox-LDL and how this contributes to the development of atherosclerosis.
Abdullatif Taha BabakrPublished: January 17, 2025 Explor Cardiol. 2025;3:101246
DOI: https://doi.org/10.37349/ec.2025.101246
This article belongs to the special issue Molecular Mechanisms of Cardiovascular AgingThe oxidation of lipoproteins has a key role in the development of atherosclerosis, a condition where plaque builds up in artery walls. Research shows that when low-density lipoprotein (LDL) oxidizes, it speeds up atherosclerosis. Oxidized LDL (Ox-LDL) causes many pathologic scenarios that lead to atherosclerosis. It was suggested as a fundamental player in endothelial dysfunction, creating foam cells, and triggering inflammation in artery walls. How Ox-LDL contributes and interacts with specific receptors on endothelial cells is crucial to these effects. This article aims to shed light on LDL oxidation, the stages of the process, and how Ox-LDL promotes atherosclerosis. A comprehensive search was conducted across various databases, including PubMed, Google Scholar, Scopus, and Ovid, to identify literature and studies that discuss Ox-LDL and their involvement in the pathogenesis of atherosclerosis and cardiovascular diseases, thereby establishing a well-defined perspective on the subject. This review will provide a closer look at the Ox-LDL particle, the different forms and stages of oxidation, and the role of various LDL receptors involved in LDL uptake and breakdown focusing on how they contribute to atherosclerosis. Then, it will discuss the role of scavenger receptors and their contribution to the uptake of Ox-LDL and how this contributes to the development of atherosclerosis.
 Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.
Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
Eugenio PicanoPublished: May 13, 2024 Explor Cardiol. 2024;2:88–96
DOI: https://doi.org/10.37349/ec.2024.00024While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
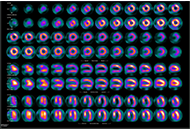
 Coronary external diameter index for assessing coronary artery involvement in Kawasaki diseaseOpen AccessOriginal ArticleAim: Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines [...] Read more.
Coronary external diameter index for assessing coronary artery involvement in Kawasaki diseaseOpen AccessOriginal ArticleAim: Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines [...] Read more.Aim:
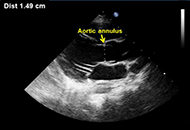
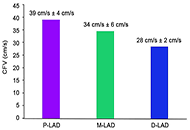
Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines the utility of a new parameter, coronary external diameter index (CEDi), for early diagnosis and monitoring in KD.
Methods:
CEDi of left main (LM) and right coronary artery (RCA), calculated as the ratio of coronary artery external diameter (i.e., the distance between the outer coronary edges measured in the proximal segment of the artery) and the diameter of the aortic annulus, was evaluated in 34 patients (age 23 mouths ± 13 months) with KD at the hospital admission and after 2 weeks and 8 weeks of treatment. The control group consisted of 210 healthy children aged 20 months ± 13.4 months. Z-score charts for LM and RCA coronary external diameter (CED) were obtained.
Results:
Compared with controls, KD patients had a markedly higher mean value of LM CEDi (0.53 ± 0.06 vs. 0.33 ± 0.04; P < 0.0001) and RCA CEDi (0.48 ± 0.05 vs. 0.31 ± 0.04; P < 0.0001) at hospital admission. By ROC analysis, LM CEDi of 0.41, and RCA coronary artery thickness index (CATi) of 0.39 were the best cut-offs to confirm the clinical diagnosis of KD, both exhibiting 100% sensitivity and specificity. Mean LM CEDi and RCA CEDi values decreased significantly (P < 0.0001) after 2 weeks of follow-up and were similar to controls (P = 0.53 and P = 0.12, respectively) 8 weeks after admission.
Conclusions:
In patients with KD, CEDi of LM and RCA is an accurate parameter to evaluate coronary artery involvement in the early phase of the illness and during follow-up.
Andrea Azzarelli ... Francesco VierucciPublished: October 31, 2023 Explor Cardiol. 2023;1:103–113
DOI: https://doi.org/10.37349/ec.2023.00011Aim:
Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines the utility of a new parameter, coronary external diameter index (CEDi), for early diagnosis and monitoring in KD.
Methods:
CEDi of left main (LM) and right coronary artery (RCA), calculated as the ratio of coronary artery external diameter (i.e., the distance between the outer coronary edges measured in the proximal segment of the artery) and the diameter of the aortic annulus, was evaluated in 34 patients (age 23 mouths ± 13 months) with KD at the hospital admission and after 2 weeks and 8 weeks of treatment. The control group consisted of 210 healthy children aged 20 months ± 13.4 months. Z-score charts for LM and RCA coronary external diameter (CED) were obtained.
Results:
Compared with controls, KD patients had a markedly higher mean value of LM CEDi (0.53 ± 0.06 vs. 0.33 ± 0.04; P < 0.0001) and RCA CEDi (0.48 ± 0.05 vs. 0.31 ± 0.04; P < 0.0001) at hospital admission. By ROC analysis, LM CEDi of 0.41, and RCA coronary artery thickness index (CATi) of 0.39 were the best cut-offs to confirm the clinical diagnosis of KD, both exhibiting 100% sensitivity and specificity. Mean LM CEDi and RCA CEDi values decreased significantly (P < 0.0001) after 2 weeks of follow-up and were similar to controls (P = 0.53 and P = 0.12, respectively) 8 weeks after admission.
Conclusions:
In patients with KD, CEDi of LM and RCA is an accurate parameter to evaluate coronary artery involvement in the early phase of the illness and during follow-up.
 Mitral valve prolapse—arrhythmic faces of the valve diseaseOpen AccessReviewMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of t [...] Read more.
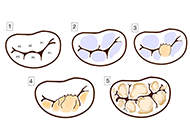
Mitral valve prolapse—arrhythmic faces of the valve diseaseOpen AccessReviewMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of t [...] Read more.Mitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of the general population. Although MVP is viewed as a benign condition, the association between MVP and sudden cardiac death (SCD) has been proven. Patients with MVP have a three times higher risk of SCD than the general population. The underlying mechanisms and predictors of arrhythmias, which occur in patients with MVP, are still poorly understood. However, some echocardiographic features such as mitral annulus disjunction (MAD), bileaflet MVP (biMVP), and papillary muscle (PM) fibrosis were frequently linked with increased number of arrhythmic events and are referred to as “arrhythmogenic” or “malignant”. Arrhythmogenic MVP (AMVP) has also been associated with other factors such as female sex, polymorphic premature ventricular contraction (PVC), abnormalities of T-waves, and Pickelhaube sign on tissue Doppler tracing of the lateral part of the mitral annulus. Cardiac magnetic resonance (CMR) imaging and speckle tracking echocardiography are new tools showing significant potential for detection of malignant features of AMVP. This paper presents various data coming from electrocardiography (ECG) analysis, echocardiography, and other imaging techniques as well as compilation of the recent studies on the subject of MVP.
Maria Możdżan ... Karina Wierzbowska-DrabikPublished: October 31, 2023 Explor Cardiol. 2023;1:72–87
DOI: https://doi.org/10.37349/ec.2023.00009
This article belongs to the special issue Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coinMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of the general population. Although MVP is viewed as a benign condition, the association between MVP and sudden cardiac death (SCD) has been proven. Patients with MVP have a three times higher risk of SCD than the general population. The underlying mechanisms and predictors of arrhythmias, which occur in patients with MVP, are still poorly understood. However, some echocardiographic features such as mitral annulus disjunction (MAD), bileaflet MVP (biMVP), and papillary muscle (PM) fibrosis were frequently linked with increased number of arrhythmic events and are referred to as “arrhythmogenic” or “malignant”. Arrhythmogenic MVP (AMVP) has also been associated with other factors such as female sex, polymorphic premature ventricular contraction (PVC), abnormalities of T-waves, and Pickelhaube sign on tissue Doppler tracing of the lateral part of the mitral annulus. Cardiac magnetic resonance (CMR) imaging and speckle tracking echocardiography are new tools showing significant potential for detection of malignant features of AMVP. This paper presents various data coming from electrocardiography (ECG) analysis, echocardiography, and other imaging techniques as well as compilation of the recent studies on the subject of MVP.
 Laboratory markers of metabolic syndromeOpen AccessReviewMetabolic syndrome (MetS) is known as a non-communicable disease (NCD) that affects more and more individuals. MetS is closely related to type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD [...] Read more.
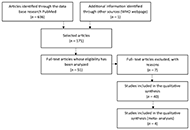
Laboratory markers of metabolic syndromeOpen AccessReviewMetabolic syndrome (MetS) is known as a non-communicable disease (NCD) that affects more and more individuals. MetS is closely related to type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD [...] Read more.Metabolic syndrome (MetS) is known as a non-communicable disease (NCD) that affects more and more individuals. MetS is closely related to type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), obesity and inflammation. It is associated with T2DM due to the disturbance in insulin secretion/effect, eventually leading to insulin resistance (IR). The link between MetS and CVD is due to accelerated atherosclerosis in response to chronic inflammation. This literature review was based on a search in the PubMed database. All selected articles are written in English and cover a period of approximately 10 years (January 2014 to May 2023). The first selection used MeSH terms such as: “metabolic syndrome”, “type 2 diabetes mellitus”, “obesity”, “inflammation”, and “insulin resistance” and different associations between them. Titles and abstracts were analyzed. In the end, 44 articles were selected, 4 of which were meta-analysis studies. Currently, an individual is considered to have MetS if they present 3 of the following changes: increased waist circumference, increased triglycerides (TG), reduced high-density lipoprotein cholesterol (HDL-C), increased fasting blood glucose and hypertension. We believe this can often lead to a false diagnosis. The objective of this paper is to compile what we consider to be an appropriate panel of MetS indicators. The markers that stand out in this review are the lipid profile, anti- and pro-inflammatory function and oxidative stress. Considering the research, we believe that a complete panel, to correlate the most characteristic conditions of MetS, should include the following markers: TG/HDL-C ratio, small dense low-density lipoprotein cholesterol (SdLDL-C), lipid peroxidation markers, leptin/adiponectin ratio, plasminogen activator inhibitor-1 (PAI-1), activin-A and ferritin levels. Finally, it is important to expand research on the pathophysiology of MetS and confirm the most appropriate markers as well as discover new ones to correctly diagnose this condition.
Filipa Morgado ... Leonel PereiraPublished: June 24, 2024 Explor Cardiol. 2024;2:114–133
DOI: https://doi.org/10.37349/ec.2024.00026
This article belongs to the special issue Molecular Mechanisms of Cardiovascular AgingMetabolic syndrome (MetS) is known as a non-communicable disease (NCD) that affects more and more individuals. MetS is closely related to type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), obesity and inflammation. It is associated with T2DM due to the disturbance in insulin secretion/effect, eventually leading to insulin resistance (IR). The link between MetS and CVD is due to accelerated atherosclerosis in response to chronic inflammation. This literature review was based on a search in the PubMed database. All selected articles are written in English and cover a period of approximately 10 years (January 2014 to May 2023). The first selection used MeSH terms such as: “metabolic syndrome”, “type 2 diabetes mellitus”, “obesity”, “inflammation”, and “insulin resistance” and different associations between them. Titles and abstracts were analyzed. In the end, 44 articles were selected, 4 of which were meta-analysis studies. Currently, an individual is considered to have MetS if they present 3 of the following changes: increased waist circumference, increased triglycerides (TG), reduced high-density lipoprotein cholesterol (HDL-C), increased fasting blood glucose and hypertension. We believe this can often lead to a false diagnosis. The objective of this paper is to compile what we consider to be an appropriate panel of MetS indicators. The markers that stand out in this review are the lipid profile, anti- and pro-inflammatory function and oxidative stress. Considering the research, we believe that a complete panel, to correlate the most characteristic conditions of MetS, should include the following markers: TG/HDL-C ratio, small dense low-density lipoprotein cholesterol (SdLDL-C), lipid peroxidation markers, leptin/adiponectin ratio, plasminogen activator inhibitor-1 (PAI-1), activin-A and ferritin levels. Finally, it is important to expand research on the pathophysiology of MetS and confirm the most appropriate markers as well as discover new ones to correctly diagnose this condition.
 Why and when should be lipoprotein(a) level measured?Open AccessReviewLipoprotein(a) [Lp(a)] is composed of a low-density lipoprotein (LDL) and glycoprotein (a)—apo(a). The size and concentration of Lp(a) in serum can vary among individuals and is determined by gene [...] Read more.
Why and when should be lipoprotein(a) level measured?Open AccessReviewLipoprotein(a) [Lp(a)] is composed of a low-density lipoprotein (LDL) and glycoprotein (a)—apo(a). The size and concentration of Lp(a) in serum can vary among individuals and is determined by gene [...] Read more.Lipoprotein(a) [Lp(a)] is composed of a low-density lipoprotein (LDL) and glycoprotein (a)—apolipoprotein(a) [apo(a)]. The size and concentration of Lp(a) in serum can vary among individuals and is determined by genetic factors. The environmental factors, diet, and physical activity have a negligible effect on Lp(a) level. Observational, epidemiological, and genetic studies improved that high levels of Lp(a) > 50 mg/dL (> 125 nmol/L) have been associated with an increased risk of myocardial infarction (MI), stroke, and calcific aortic valve stenosis (CAVS). It is recommended to measure Lp(a) at least once in adults to identify individuals with a high cardiovascular risk. This screening is particularly important in certain populations, including: youth with a history of ischemic stroke or a family history of premature atherosclerotic cardiovascular disease (CVD; ASCVD) or high Lp(a), individuals with recurrent cardiovascular events despite optimal hypolipemic treatment and no other identifiable risk factors or patients with familial hypercholesterolemia (FH). Considering Lp(a) levels in the evaluation of cardiovascular risk can provide valuable information for risk stratification and management decisions. However, it’s important to note that the treatments of elevated level of Lp(a) are limited. In recent years, there has been ongoing research and development of new drugs targeting Lp(a): pelacarsen—antisense oligonucleotide (ASO), and olpasiran—a small interfering RNA (siRNA).
Miłosz Broncel, Marlena BroncelPublished: December 29, 2023 Explor Cardiol. 2023;1:180–192
DOI: https://doi.org/10.37349/ec.2023.00015
This article belongs to the special issue Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coinLipoprotein(a) [Lp(a)] is composed of a low-density lipoprotein (LDL) and glycoprotein (a)—apolipoprotein(a) [apo(a)]. The size and concentration of Lp(a) in serum can vary among individuals and is determined by genetic factors. The environmental factors, diet, and physical activity have a negligible effect on Lp(a) level. Observational, epidemiological, and genetic studies improved that high levels of Lp(a) > 50 mg/dL (> 125 nmol/L) have been associated with an increased risk of myocardial infarction (MI), stroke, and calcific aortic valve stenosis (CAVS). It is recommended to measure Lp(a) at least once in adults to identify individuals with a high cardiovascular risk. This screening is particularly important in certain populations, including: youth with a history of ischemic stroke or a family history of premature atherosclerotic cardiovascular disease (CVD; ASCVD) or high Lp(a), individuals with recurrent cardiovascular events despite optimal hypolipemic treatment and no other identifiable risk factors or patients with familial hypercholesterolemia (FH). Considering Lp(a) levels in the evaluation of cardiovascular risk can provide valuable information for risk stratification and management decisions. However, it’s important to note that the treatments of elevated level of Lp(a) are limited. In recent years, there has been ongoing research and development of new drugs targeting Lp(a): pelacarsen—antisense oligonucleotide (ASO), and olpasiran—a small interfering RNA (siRNA).
 B-lines by lung ultrasound in cardiologyOpen AccessReviewPulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo G [...] Read more.
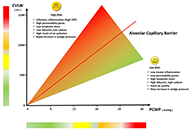
B-lines by lung ultrasound in cardiologyOpen AccessReviewPulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo G [...] Read more.Pulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo Giuntini, a pneumologist who attempted the quantification of lung water in the seventies with too insensitive chest X-ray lung water score, too cumbersome nuclear medicine, and too complex invasive thermodilution techniques. Daniel Lichtenstein, is a French intensivist who first discovered lung ultrasound as a sign of extravascular lung water in 1997. B-lines (also known as ultrasound lung comets) detectable by lung ultrasound arise from the pleural line, extend towards the edge of the screen, and move synchronously with respiration. In cardiology, B-lines were introduced in 2004 and are now the dominant technique for research applications and clinical purposes. B-lines showed a prognostic value in several clinical scenarios, largely independent and additive over echocardiographic predictors such as ejection fraction. The methodology became user-friendly in the last years, with a reduction of the scanning sites from the original 28 to a simplified 4-site scan now extracting information on lung water in < 1 minute. More recently, B-lines were also studied during physical and pharmacological stress. Signs of pulmonary congestion are found during stress in 1 out of 3 all-comers with normal findings at rest. Artificial intelligence applied to ultrasound and clinical data allows for the detection of B lines, their quantification, and the assessment of their nature. The B-lines phenotype can cluster around different endotypes: dry (in systemic sclerosis and lung interstitial fibrosis); wet (water); sterile (as in cardiogenic edema); infective (as in COVID-19 and interstitial pneumonia); right heart-sided (as in pulmonary arterial hypertension); left-heart sided (as in heart failure or valvular heart disease). Artificial intelligence B-lines and pocket-size insonation of the B-lines-driven decongestion therapy are now on the horizon.
Marco Antonio Rodrigues Torres, Natália Moraes de QuevedoPublished: November 14, 2024 Explor Cardiol. 2024;2:265–279
DOI: https://doi.org/10.37349/ec.2024.00039
This article belongs to the special issue Multimodality Imaging in Ischemic Heart DiseasePulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo Giuntini, a pneumologist who attempted the quantification of lung water in the seventies with too insensitive chest X-ray lung water score, too cumbersome nuclear medicine, and too complex invasive thermodilution techniques. Daniel Lichtenstein, is a French intensivist who first discovered lung ultrasound as a sign of extravascular lung water in 1997. B-lines (also known as ultrasound lung comets) detectable by lung ultrasound arise from the pleural line, extend towards the edge of the screen, and move synchronously with respiration. In cardiology, B-lines were introduced in 2004 and are now the dominant technique for research applications and clinical purposes. B-lines showed a prognostic value in several clinical scenarios, largely independent and additive over echocardiographic predictors such as ejection fraction. The methodology became user-friendly in the last years, with a reduction of the scanning sites from the original 28 to a simplified 4-site scan now extracting information on lung water in < 1 minute. More recently, B-lines were also studied during physical and pharmacological stress. Signs of pulmonary congestion are found during stress in 1 out of 3 all-comers with normal findings at rest. Artificial intelligence applied to ultrasound and clinical data allows for the detection of B lines, their quantification, and the assessment of their nature. The B-lines phenotype can cluster around different endotypes: dry (in systemic sclerosis and lung interstitial fibrosis); wet (water); sterile (as in cardiogenic edema); infective (as in COVID-19 and interstitial pneumonia); right heart-sided (as in pulmonary arterial hypertension); left-heart sided (as in heart failure or valvular heart disease). Artificial intelligence B-lines and pocket-size insonation of the B-lines-driven decongestion therapy are now on the horizon.
 Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.
Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
Eugenio PicanoPublished: May 13, 2024 Explor Cardiol. 2024;2:88–96
DOI: https://doi.org/10.37349/ec.2024.00024While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
 Coronary external diameter index for assessing coronary artery involvement in Kawasaki diseaseOpen AccessOriginal ArticleAim: Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines [...] Read more.
Coronary external diameter index for assessing coronary artery involvement in Kawasaki diseaseOpen AccessOriginal ArticleAim: Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines [...] Read more.Aim:
Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines the utility of a new parameter, coronary external diameter index (CEDi), for early diagnosis and monitoring in KD.
Methods:
CEDi of left main (LM) and right coronary artery (RCA), calculated as the ratio of coronary artery external diameter (i.e., the distance between the outer coronary edges measured in the proximal segment of the artery) and the diameter of the aortic annulus, was evaluated in 34 patients (age 23 mouths ± 13 months) with KD at the hospital admission and after 2 weeks and 8 weeks of treatment. The control group consisted of 210 healthy children aged 20 months ± 13.4 months. Z-score charts for LM and RCA coronary external diameter (CED) were obtained.
Results:
Compared with controls, KD patients had a markedly higher mean value of LM CEDi (0.53 ± 0.06 vs. 0.33 ± 0.04; P < 0.0001) and RCA CEDi (0.48 ± 0.05 vs. 0.31 ± 0.04; P < 0.0001) at hospital admission. By ROC analysis, LM CEDi of 0.41, and RCA coronary artery thickness index (CATi) of 0.39 were the best cut-offs to confirm the clinical diagnosis of KD, both exhibiting 100% sensitivity and specificity. Mean LM CEDi and RCA CEDi values decreased significantly (P < 0.0001) after 2 weeks of follow-up and were similar to controls (P = 0.53 and P = 0.12, respectively) 8 weeks after admission.
Conclusions:
In patients with KD, CEDi of LM and RCA is an accurate parameter to evaluate coronary artery involvement in the early phase of the illness and during follow-up.
Andrea Azzarelli ... Francesco VierucciPublished: October 31, 2023 Explor Cardiol. 2023;1:103–113
DOI: https://doi.org/10.37349/ec.2023.00011Aim:
Transthoracic echocardiography is commonly used to assess coronary artery dilatation in Kawasaki disease (KD). However, existing criteria often miss early abnormalities. This study examines the utility of a new parameter, coronary external diameter index (CEDi), for early diagnosis and monitoring in KD.
Methods:
CEDi of left main (LM) and right coronary artery (RCA), calculated as the ratio of coronary artery external diameter (i.e., the distance between the outer coronary edges measured in the proximal segment of the artery) and the diameter of the aortic annulus, was evaluated in 34 patients (age 23 mouths ± 13 months) with KD at the hospital admission and after 2 weeks and 8 weeks of treatment. The control group consisted of 210 healthy children aged 20 months ± 13.4 months. Z-score charts for LM and RCA coronary external diameter (CED) were obtained.
Results:
Compared with controls, KD patients had a markedly higher mean value of LM CEDi (0.53 ± 0.06 vs. 0.33 ± 0.04; P < 0.0001) and RCA CEDi (0.48 ± 0.05 vs. 0.31 ± 0.04; P < 0.0001) at hospital admission. By ROC analysis, LM CEDi of 0.41, and RCA coronary artery thickness index (CATi) of 0.39 were the best cut-offs to confirm the clinical diagnosis of KD, both exhibiting 100% sensitivity and specificity. Mean LM CEDi and RCA CEDi values decreased significantly (P < 0.0001) after 2 weeks of follow-up and were similar to controls (P = 0.53 and P = 0.12, respectively) 8 weeks after admission.
Conclusions:
In patients with KD, CEDi of LM and RCA is an accurate parameter to evaluate coronary artery involvement in the early phase of the illness and during follow-up.
 B-lines by lung ultrasound in cardiologyOpen AccessReviewPulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo G [...] Read more.
B-lines by lung ultrasound in cardiologyOpen AccessReviewPulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo G [...] Read more.Pulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo Giuntini, a pneumologist who attempted the quantification of lung water in the seventies with too insensitive chest X-ray lung water score, too cumbersome nuclear medicine, and too complex invasive thermodilution techniques. Daniel Lichtenstein, is a French intensivist who first discovered lung ultrasound as a sign of extravascular lung water in 1997. B-lines (also known as ultrasound lung comets) detectable by lung ultrasound arise from the pleural line, extend towards the edge of the screen, and move synchronously with respiration. In cardiology, B-lines were introduced in 2004 and are now the dominant technique for research applications and clinical purposes. B-lines showed a prognostic value in several clinical scenarios, largely independent and additive over echocardiographic predictors such as ejection fraction. The methodology became user-friendly in the last years, with a reduction of the scanning sites from the original 28 to a simplified 4-site scan now extracting information on lung water in < 1 minute. More recently, B-lines were also studied during physical and pharmacological stress. Signs of pulmonary congestion are found during stress in 1 out of 3 all-comers with normal findings at rest. Artificial intelligence applied to ultrasound and clinical data allows for the detection of B lines, their quantification, and the assessment of their nature. The B-lines phenotype can cluster around different endotypes: dry (in systemic sclerosis and lung interstitial fibrosis); wet (water); sterile (as in cardiogenic edema); infective (as in COVID-19 and interstitial pneumonia); right heart-sided (as in pulmonary arterial hypertension); left-heart sided (as in heart failure or valvular heart disease). Artificial intelligence B-lines and pocket-size insonation of the B-lines-driven decongestion therapy are now on the horizon.
Marco Antonio Rodrigues Torres, Natália Moraes de QuevedoPublished: November 14, 2024 Explor Cardiol. 2024;2:265–279
DOI: https://doi.org/10.37349/ec.2024.00039
This article belongs to the special issue Multimodality Imaging in Ischemic Heart DiseasePulmonary congestion is a key determinant of heart failure, but for a long time it has been an elusive target for the clinical cardiologist in the pre-B-line era, despite research efforts of Carlo Giuntini, a pneumologist who attempted the quantification of lung water in the seventies with too insensitive chest X-ray lung water score, too cumbersome nuclear medicine, and too complex invasive thermodilution techniques. Daniel Lichtenstein, is a French intensivist who first discovered lung ultrasound as a sign of extravascular lung water in 1997. B-lines (also known as ultrasound lung comets) detectable by lung ultrasound arise from the pleural line, extend towards the edge of the screen, and move synchronously with respiration. In cardiology, B-lines were introduced in 2004 and are now the dominant technique for research applications and clinical purposes. B-lines showed a prognostic value in several clinical scenarios, largely independent and additive over echocardiographic predictors such as ejection fraction. The methodology became user-friendly in the last years, with a reduction of the scanning sites from the original 28 to a simplified 4-site scan now extracting information on lung water in < 1 minute. More recently, B-lines were also studied during physical and pharmacological stress. Signs of pulmonary congestion are found during stress in 1 out of 3 all-comers with normal findings at rest. Artificial intelligence applied to ultrasound and clinical data allows for the detection of B lines, their quantification, and the assessment of their nature. The B-lines phenotype can cluster around different endotypes: dry (in systemic sclerosis and lung interstitial fibrosis); wet (water); sterile (as in cardiogenic edema); infective (as in COVID-19 and interstitial pneumonia); right heart-sided (as in pulmonary arterial hypertension); left-heart sided (as in heart failure or valvular heart disease). Artificial intelligence B-lines and pocket-size insonation of the B-lines-driven decongestion therapy are now on the horizon.
 Diagnostic modalities for ischemic heart disease: evaluating the role of stress echocardiography, cardiac CT, and myocardial perfusion scintigraphy in guiding coronary angiographyOpen AccessReviewCardiovascular diseases, particularly ischemic heart disease (IHD), are the leading cause of mortality globally, accounting for 16% of deaths. Effective management of ischemic cardiomyopathy (ICM) i [...] Read more.
Diagnostic modalities for ischemic heart disease: evaluating the role of stress echocardiography, cardiac CT, and myocardial perfusion scintigraphy in guiding coronary angiographyOpen AccessReviewCardiovascular diseases, particularly ischemic heart disease (IHD), are the leading cause of mortality globally, accounting for 16% of deaths. Effective management of ischemic cardiomyopathy (ICM) i [...] Read more.Cardiovascular diseases, particularly ischemic heart disease (IHD), are the leading cause of mortality globally, accounting for 16% of deaths. Effective management of ischemic cardiomyopathy (ICM) is crucial, as outlined in the latest European Society of Cardiology (ESC) guidelines for chronic coronary syndrome (CCS). The guidelines emphasize a structured approach comprising four key steps: a general clinical evaluation to exclude non-cardiac causes, cardiac examination, and likelihood estimation using echocardiography, diagnostic testing such as stress echocardiography and coronary CT angiography, and treatment involving lifestyle changes and medication, alongside potential revascularization. The review underscores the importance of coronary angiography and functional assessments in diagnosing ischemic heart failure (IHF) and guiding treatment strategies. Non-invasive imaging techniques, including stress echocardiography and myocardial perfusion scintigraphy, are valuable for assessing ischemia and myocardial viability while reducing unnecessary invasive procedures. Coronary CT angiography is also examined for its procedural advantages and risks. A comparative analysis of diagnostic modalities highlights the strengths and limitations of each technique, emphasizing the need for individualized approaches based on patient characteristics. The ESC 2024 guidelines advocate for a patient-centered imaging strategy based on the likelihood of coronary artery disease (CAD) while addressing the economic and environmental impacts of imaging practices. Overall, implementing these guidelines and leveraging diverse imaging modalities can optimize management strategies for IHD, ultimately improving patient outcomes.
Marco Fabio Costantino ... Luisiana StolfiPublished: January 13, 2025 Explor Cardiol. 2025;3:101243
DOI: https://doi.org/10.37349/ec.2025.101243
This article belongs to the special issue Multimodality Imaging in Ischemic Heart DiseaseCardiovascular diseases, particularly ischemic heart disease (IHD), are the leading cause of mortality globally, accounting for 16% of deaths. Effective management of ischemic cardiomyopathy (ICM) is crucial, as outlined in the latest European Society of Cardiology (ESC) guidelines for chronic coronary syndrome (CCS). The guidelines emphasize a structured approach comprising four key steps: a general clinical evaluation to exclude non-cardiac causes, cardiac examination, and likelihood estimation using echocardiography, diagnostic testing such as stress echocardiography and coronary CT angiography, and treatment involving lifestyle changes and medication, alongside potential revascularization. The review underscores the importance of coronary angiography and functional assessments in diagnosing ischemic heart failure (IHF) and guiding treatment strategies. Non-invasive imaging techniques, including stress echocardiography and myocardial perfusion scintigraphy, are valuable for assessing ischemia and myocardial viability while reducing unnecessary invasive procedures. Coronary CT angiography is also examined for its procedural advantages and risks. A comparative analysis of diagnostic modalities highlights the strengths and limitations of each technique, emphasizing the need for individualized approaches based on patient characteristics. The ESC 2024 guidelines advocate for a patient-centered imaging strategy based on the likelihood of coronary artery disease (CAD) while addressing the economic and environmental impacts of imaging practices. Overall, implementing these guidelines and leveraging diverse imaging modalities can optimize management strategies for IHD, ultimately improving patient outcomes.
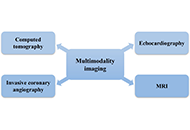
 Emerging technologies and applications in multimodality imaging for ischemic heart disease: current state and future of artificial intelligenceOpen AccessReviewIschemic heart disease (IHD) is a major global health issue, frequently resulting in myocardial infarction and ischemic cardiomyopathy. Prompt and precise diagnosis is essential to avert complicatio [...] Read more.
Emerging technologies and applications in multimodality imaging for ischemic heart disease: current state and future of artificial intelligenceOpen AccessReviewIschemic heart disease (IHD) is a major global health issue, frequently resulting in myocardial infarction and ischemic cardiomyopathy. Prompt and precise diagnosis is essential to avert complicatio [...] Read more.Ischemic heart disease (IHD) is a major global health issue, frequently resulting in myocardial infarction and ischemic cardiomyopathy. Prompt and precise diagnosis is essential to avert complications such as heart failure and sudden cardiac death. Although invasive coronary angiography remains the gold standard for high-risk patients, noninvasive multimodality imaging is becoming more prevalent for those at low-to-intermediate risk. This review evaluated the current state of multimodality imaging in IHD, including echocardiography, nuclear cardiology, cardiac magnetic resonance imaging (MRI), computed tomography (CT) angiography, and invasive coronary angiography. Each modality has distinct strengths and limitations, and their complementary use provides a comprehensive assessment of cardiac health. Integrating artificial intelligence (AI) into imaging workflows holds promise for enhancing diagnostic accuracy and efficiency. AI algorithms can optimize image acquisition, processing, and interpretation of complex imaging data. Emerging technologies like 4D flow MRI, molecular imaging, and hybrid systems [e.g., positron emission tomography (PET)/MRI, PET/CT] integrate anatomical, functional, and molecular data, providing comprehensive insights into cardiac pathology and potentially revolutionizing the management of IHD. This review also explored the clinical applications and impact of multimodality imaging on patient outcomes, emphasizing its role in improving diagnostic precision and guiding therapeutic decisions. Future directions include AI-driven decision support systems and personalized medicine approaches. Addressing regulatory and ethical challenges, such as data privacy and algorithm transparency, is crucial for the broader adoption of these advanced technologies. This review highlighted the transformative potential of AI-enhanced multimodality imaging in improving the diagnosis and management of IHD.
Praveen Kumar Chandra Sekar, Ramakrishnan VeerabathiranPublished: November 11, 2024 Explor Cardiol. 2024;2:253–264
DOI: https://doi.org/10.37349/ec.2024.00038
This article belongs to the special issue Multimodality Imaging in Ischemic Heart DiseaseIschemic heart disease (IHD) is a major global health issue, frequently resulting in myocardial infarction and ischemic cardiomyopathy. Prompt and precise diagnosis is essential to avert complications such as heart failure and sudden cardiac death. Although invasive coronary angiography remains the gold standard for high-risk patients, noninvasive multimodality imaging is becoming more prevalent for those at low-to-intermediate risk. This review evaluated the current state of multimodality imaging in IHD, including echocardiography, nuclear cardiology, cardiac magnetic resonance imaging (MRI), computed tomography (CT) angiography, and invasive coronary angiography. Each modality has distinct strengths and limitations, and their complementary use provides a comprehensive assessment of cardiac health. Integrating artificial intelligence (AI) into imaging workflows holds promise for enhancing diagnostic accuracy and efficiency. AI algorithms can optimize image acquisition, processing, and interpretation of complex imaging data. Emerging technologies like 4D flow MRI, molecular imaging, and hybrid systems [e.g., positron emission tomography (PET)/MRI, PET/CT] integrate anatomical, functional, and molecular data, providing comprehensive insights into cardiac pathology and potentially revolutionizing the management of IHD. This review also explored the clinical applications and impact of multimodality imaging on patient outcomes, emphasizing its role in improving diagnostic precision and guiding therapeutic decisions. Future directions include AI-driven decision support systems and personalized medicine approaches. Addressing regulatory and ethical challenges, such as data privacy and algorithm transparency, is crucial for the broader adoption of these advanced technologies. This review highlighted the transformative potential of AI-enhanced multimodality imaging in improving the diagnosis and management of IHD.
 Mitral valve prolapse—arrhythmic faces of the valve diseaseOpen AccessReviewMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of t [...] Read more.
Mitral valve prolapse—arrhythmic faces of the valve diseaseOpen AccessReviewMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of t [...] Read more.Mitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of the general population. Although MVP is viewed as a benign condition, the association between MVP and sudden cardiac death (SCD) has been proven. Patients with MVP have a three times higher risk of SCD than the general population. The underlying mechanisms and predictors of arrhythmias, which occur in patients with MVP, are still poorly understood. However, some echocardiographic features such as mitral annulus disjunction (MAD), bileaflet MVP (biMVP), and papillary muscle (PM) fibrosis were frequently linked with increased number of arrhythmic events and are referred to as “arrhythmogenic” or “malignant”. Arrhythmogenic MVP (AMVP) has also been associated with other factors such as female sex, polymorphic premature ventricular contraction (PVC), abnormalities of T-waves, and Pickelhaube sign on tissue Doppler tracing of the lateral part of the mitral annulus. Cardiac magnetic resonance (CMR) imaging and speckle tracking echocardiography are new tools showing significant potential for detection of malignant features of AMVP. This paper presents various data coming from electrocardiography (ECG) analysis, echocardiography, and other imaging techniques as well as compilation of the recent studies on the subject of MVP.
Maria Możdżan ... Karina Wierzbowska-DrabikPublished: October 31, 2023 Explor Cardiol. 2023;1:72–87
DOI: https://doi.org/10.37349/ec.2023.00009
This article belongs to the special issue Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coinMitral valve prolapse (MVP) is a relatively common mitral valvulopathy and the most common cause of isolated primary mitral regurgitation (MR) requiring surgical repair. It affects about 1–3% of the general population. Although MVP is viewed as a benign condition, the association between MVP and sudden cardiac death (SCD) has been proven. Patients with MVP have a three times higher risk of SCD than the general population. The underlying mechanisms and predictors of arrhythmias, which occur in patients with MVP, are still poorly understood. However, some echocardiographic features such as mitral annulus disjunction (MAD), bileaflet MVP (biMVP), and papillary muscle (PM) fibrosis were frequently linked with increased number of arrhythmic events and are referred to as “arrhythmogenic” or “malignant”. Arrhythmogenic MVP (AMVP) has also been associated with other factors such as female sex, polymorphic premature ventricular contraction (PVC), abnormalities of T-waves, and Pickelhaube sign on tissue Doppler tracing of the lateral part of the mitral annulus. Cardiac magnetic resonance (CMR) imaging and speckle tracking echocardiography are new tools showing significant potential for detection of malignant features of AMVP. This paper presents various data coming from electrocardiography (ECG) analysis, echocardiography, and other imaging techniques as well as compilation of the recent studies on the subject of MVP.
 Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.
Who is the author: genuine, honorary, ghost, gold, and fake authors?Open AccessEditorialWhile authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public [...] Read more.While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
Eugenio PicanoPublished: May 13, 2024 Explor Cardiol. 2024;2:88–96
DOI: https://doi.org/10.37349/ec.2024.00024While authorship practices can vary across different disciplines, authorship should reflect the individuals who have made a substantial contribution to the research project, take public responsibility for the paper’s content, and agree to its submission for publication. In real life, the article is usually authored by at least one truly genuine author and some parasitic authors. The first author and the last author are especially important. The middle authors are less important, and their participation is often wrongly seen as an inconsequential decorative favor. The honorary author, a gift or guest author, is added as a bonus to please someone higher in the hierarchy than the submitting author. This practice is believed to enhance the chances of publication, but usually, the excess of honorary authors will make reviewers more critical. A ghost author contributed substantially but it does not appear in the list of authors to avoid declaring an overt conflict of interest. The gold author is someone paid by a third party in direct or indirect forms, and capable of writing and signing everything asked by the payer, including overstating the merits of a new drug or ignoring its drawbacks. A fake author does not exist, and while it may seem humorous it is a breach of scientific integrity and can lead to serious consequences for the individuals involved. With Chat-generative pre-trained transformer (Chat-GPT), artificial intelligence may contribute decisively to the article content and presentation. Overall, it is important to maintain high standards of integrity and transparency in authorship practices to ensure that research findings are trustworthy and reliable. The reputation of your work is in the hands of your coauthors, so choose them carefully and make sure they share your commitment to scientific integrity.
 Low-doses ionizing radiation exposure: an emerging causal risk factor for cardiovascular diseaseOpen AccessCommentaryMaria Grazia AndreassiPublished: December 11, 2023 Explor Cardiol. 2023;1:141–147
Low-doses ionizing radiation exposure: an emerging causal risk factor for cardiovascular diseaseOpen AccessCommentaryMaria Grazia AndreassiPublished: December 11, 2023 Explor Cardiol. 2023;1:141–147
DOI: https://doi.org/10.37349/ec.2023.00013
This article belongs to the special issue Environmental Cardiology Noninvasive identification and therapeutic implications of supernormal left ventricular contractile phenotypeOpen AccessReviewLeft ventricular (LV) function is typically evaluated through LV ejection fraction (EF), a robust indicator of risk, showing a nonlinear increase in mortality rates below 40%. Conversely, [...] Read more.
Noninvasive identification and therapeutic implications of supernormal left ventricular contractile phenotypeOpen AccessReviewLeft ventricular (LV) function is typically evaluated through LV ejection fraction (EF), a robust indicator of risk, showing a nonlinear increase in mortality rates below 40%. Conversely, [...] Read more.Left ventricular (LV) function is typically evaluated through LV ejection fraction (EF), a robust indicator of risk, showing a nonlinear increase in mortality rates below 40%. Conversely, excessively high EF values (> 65%) also correlate with elevated mortality, following a U-shaped curve, with its nadir observed between 50% and 65%. This underscores the necessity for improved identification of the hypercontractile phenotype. However, EF is not synonymous with LV contraction function, as it can fluctuate independently of contractility due to variations in afterload, preload, heart rate, and ventricular-arterial coupling. Assessing the contractile status of the LV requires more specific metrics, such as LV elastance (or contractile force) and global longitudinal strain. Current guidelines outline various parameters for a more precise characterization of LV contractility, yet further research is warranted for validation. The true hypercontractile phenotype is evident in cardiac pathologies such as hypertrophic cardiomyopathy, ischemia with angiographically normal coronary arteries, Tako-tsubo syndrome, heart failure with preserved EF, and may also stem from systemic disorders including anemia, hyperthyroidism, liver, kidney, or pulmonary diseases. The hypercontractile phenotype constitutes a distinctive hemodynamic substrate underlying clinical manifestations such as angina, dyspnea, or arrhythmias, presenting a target for intervention through beta-blockers or specific cardiac myosin inhibitors. While EF remains pivotal for clinical classification, risk stratification, and therapeutic decision-making, integrating it with other indices of LV function can enhance the characterization of the hypercontractile phenotype.
Yi Wang, Lixue YinPublished: June 17, 2024 Explor Cardiol. 2024;2:97–113
DOI: https://doi.org/10.37349/ec.2024.00025Left ventricular (LV) function is typically evaluated through LV ejection fraction (EF), a robust indicator of risk, showing a nonlinear increase in mortality rates below 40%. Conversely, excessively high EF values (> 65%) also correlate with elevated mortality, following a U-shaped curve, with its nadir observed between 50% and 65%. This underscores the necessity for improved identification of the hypercontractile phenotype. However, EF is not synonymous with LV contraction function, as it can fluctuate independently of contractility due to variations in afterload, preload, heart rate, and ventricular-arterial coupling. Assessing the contractile status of the LV requires more specific metrics, such as LV elastance (or contractile force) and global longitudinal strain. Current guidelines outline various parameters for a more precise characterization of LV contractility, yet further research is warranted for validation. The true hypercontractile phenotype is evident in cardiac pathologies such as hypertrophic cardiomyopathy, ischemia with angiographically normal coronary arteries, Tako-tsubo syndrome, heart failure with preserved EF, and may also stem from systemic disorders including anemia, hyperthyroidism, liver, kidney, or pulmonary diseases. The hypercontractile phenotype constitutes a distinctive hemodynamic substrate underlying clinical manifestations such as angina, dyspnea, or arrhythmias, presenting a target for intervention through beta-blockers or specific cardiac myosin inhibitors. While EF remains pivotal for clinical classification, risk stratification, and therapeutic decision-making, integrating it with other indices of LV function can enhance the characterization of the hypercontractile phenotype.
 Normal physiologic coronary flow velocity gradient across the left anterior descending artery in healthy asymptomatic subjectsOpen AccessOriginal ArticleAim: Coronary flow velocity (CFV) can be obtained with transthoracic echocardiography (TTE) in the left anterior descending coronary artery (LAD). The physiologic flow velocity gradient across th [...] Read more.
Normal physiologic coronary flow velocity gradient across the left anterior descending artery in healthy asymptomatic subjectsOpen AccessOriginal ArticleAim: Coronary flow velocity (CFV) can be obtained with transthoracic echocardiography (TTE) in the left anterior descending coronary artery (LAD). The physiologic flow velocity gradient across th [...] Read more.Aim:
Coronary flow velocity (CFV) can be obtained with transthoracic echocardiography (TTE) in the left anterior descending coronary artery (LAD). The physiologic flow velocity gradient across the different segments of LAD has not been established. This study aims to assess the normal values of resting CFV in proximal, mid, and distal LAD.
Methods:
In a single center, prospective, observational study design, TTE was attempted on 110 consecutive, asymptomatic middle-aged subjects (age = 55 years, 46% males) with a low likelihood of coronary artery disease (< 5%). Resting CFV in the LAD was assessed with high-end machines, dedicated coronary pre-set, and high-frequency transducers by pulsed-wave Doppler under color-Doppler guidance in the proximal, mid, and distal segments.
Results:
The technical success rate for CFV imaging was lowest for the proximal (101/110, 92%), intermediate for mid (106/110, 96%), and highest for the distal segment (108/110, 98%). All 3 segments were interpretable in 101 subjects. CFV was highest in proximal segments (38.6 cm/s ± 3.9 cm/s), intermediate in mid segments (34.3 cm/s ± 6.04 cm/s, P < 0.01 vs. proximal), and lowest in distal segments (28.1 cm/s ± 1.7 cm/s, P < 0.01 vs. proximal and vs. mid).
Conclusions:
A resting evaluation of CFV-LAD can be obtained by TTE in the large majority of consecutive subjects referred to the echocardiography laboratory. Feasibility is highest for distal and lowest for proximal-LAD segments. There is a clear physiologic gradient of CFV with decreasing values, of about 10% for each step, going from proximal to mid and distal segments of LAD. When resting CFV is considered, the site of the sampling is important to obtain comparable and physiologically meaningful data.
Fausto Rigo ... Maurizio AgnolettoPublished: August 31, 2023 Explor Cardiol. 2023;1:42–48
DOI: https://doi.org/10.37349/ec.2023.00006Aim:
Coronary flow velocity (CFV) can be obtained with transthoracic echocardiography (TTE) in the left anterior descending coronary artery (LAD). The physiologic flow velocity gradient across the different segments of LAD has not been established. This study aims to assess the normal values of resting CFV in proximal, mid, and distal LAD.
Methods:
In a single center, prospective, observational study design, TTE was attempted on 110 consecutive, asymptomatic middle-aged subjects (age = 55 years, 46% males) with a low likelihood of coronary artery disease (< 5%). Resting CFV in the LAD was assessed with high-end machines, dedicated coronary pre-set, and high-frequency transducers by pulsed-wave Doppler under color-Doppler guidance in the proximal, mid, and distal segments.
Results:
The technical success rate for CFV imaging was lowest for the proximal (101/110, 92%), intermediate for mid (106/110, 96%), and highest for the distal segment (108/110, 98%). All 3 segments were interpretable in 101 subjects. CFV was highest in proximal segments (38.6 cm/s ± 3.9 cm/s), intermediate in mid segments (34.3 cm/s ± 6.04 cm/s, P < 0.01 vs. proximal), and lowest in distal segments (28.1 cm/s ± 1.7 cm/s, P < 0.01 vs. proximal and vs. mid).
Conclusions:
A resting evaluation of CFV-LAD can be obtained by TTE in the large majority of consecutive subjects referred to the echocardiography laboratory. Feasibility is highest for distal and lowest for proximal-LAD segments. There is a clear physiologic gradient of CFV with decreasing values, of about 10% for each step, going from proximal to mid and distal segments of LAD. When resting CFV is considered, the site of the sampling is important to obtain comparable and physiologically meaningful data.
 Vascular senescence and atherosclerotic plaque vulnerability: investigating the telomere-mitochondria crosstalk—rationale and design of the VICTORIA StudyOpen AccessProtocolVascular aging is recognized as one of the hallmarks of atherosclerosis. Currently, a growing body of evidence suggests that there exists a mutual crosstalk between telomere dysfunction and mitochon [...] Read more.
Vascular senescence and atherosclerotic plaque vulnerability: investigating the telomere-mitochondria crosstalk—rationale and design of the VICTORIA StudyOpen AccessProtocolVascular aging is recognized as one of the hallmarks of atherosclerosis. Currently, a growing body of evidence suggests that there exists a mutual crosstalk between telomere dysfunction and mitochon [...] Read more.Vascular aging is recognized as one of the hallmarks of atherosclerosis. Currently, a growing body of evidence suggests that there exists a mutual crosstalk between telomere dysfunction and mitochondrial dysmetabolism during the process of vascular senescence. This underscores the importance of comprehensively studying the molecular mediators involved in this complex and intricate connection. In pursuit of this goal, the “VICTORIA” protocol entails a prospective single-center cohort study aimed at recruiting patients undergoing coronary angiography at Niguarda Hospital in Italy. The primary objective is to explore potential associations between peripheral markers of cell aging (telomere length and mtDNA content), dysregulation of non-coding RNA [specifically lncRNA TERRA and mitochondrial microRNA (MitomiR)], and the varied presentations of ischemic heart disease (stable angina, unstable angina, NSTEMI, and STEMI). Furthermore, we aim to investigate whether these markers correlate with vulnerable plaque characteristics, as assessed by optical coherence tomography findings. Additionally, systemic levels of pro-inflammatory biomarkers and novel indicators of senescence will be assessed. Patients will be followed up at 1 year to monitor primary outcomes including mortality, myocardial infarction, stroke, unplanned revascularization, and rehospitalization. The anticipated findings of this study hold promise for advancing our understanding of the telomere-mitochondria crosstalk, potentially paving the way for novel treatment modalities and refined risk stratification approaches for acute coronary syndrome.
Jonica Campolo ... Maria Grazia AndreassiPublished: July 24, 2024 Explor Cardiol. 2024;2:168–177
DOI: https://doi.org/10.37349/ec.2024.00030
This article belongs to the special issue Molecular Mechanisms of Cardiovascular AgingVascular aging is recognized as one of the hallmarks of atherosclerosis. Currently, a growing body of evidence suggests that there exists a mutual crosstalk between telomere dysfunction and mitochondrial dysmetabolism during the process of vascular senescence. This underscores the importance of comprehensively studying the molecular mediators involved in this complex and intricate connection. In pursuit of this goal, the “VICTORIA” protocol entails a prospective single-center cohort study aimed at recruiting patients undergoing coronary angiography at Niguarda Hospital in Italy. The primary objective is to explore potential associations between peripheral markers of cell aging (telomere length and mtDNA content), dysregulation of non-coding RNA [specifically lncRNA TERRA and mitochondrial microRNA (MitomiR)], and the varied presentations of ischemic heart disease (stable angina, unstable angina, NSTEMI, and STEMI). Furthermore, we aim to investigate whether these markers correlate with vulnerable plaque characteristics, as assessed by optical coherence tomography findings. Additionally, systemic levels of pro-inflammatory biomarkers and novel indicators of senescence will be assessed. Patients will be followed up at 1 year to monitor primary outcomes including mortality, myocardial infarction, stroke, unplanned revascularization, and rehospitalization. The anticipated findings of this study hold promise for advancing our understanding of the telomere-mitochondria crosstalk, potentially paving the way for novel treatment modalities and refined risk stratification approaches for acute coronary syndrome.
 Left atrium stress echocardiography: correlation between left atrial volume, function, and B-lines at rest and during stressOpen AccessOriginal ArticleAim: Left atrial volume index (LAVI), left atrial reservoir function through left atrial reservoir strain (LASr), and B-lines in lung ultrasound serve as supplementary indicators of left ventricu [...] Read more.
Left atrium stress echocardiography: correlation between left atrial volume, function, and B-lines at rest and during stressOpen AccessOriginal ArticleAim: Left atrial volume index (LAVI), left atrial reservoir function through left atrial reservoir strain (LASr), and B-lines in lung ultrasound serve as supplementary indicators of left ventricu [...] Read more.Aim:
Left atrial volume index (LAVI), left atrial reservoir function through left atrial reservoir strain (LASr), and B-lines in lung ultrasound serve as supplementary indicators of left ventricular filling pressures. This study analyzes the interrelation between LAVI, LASr, and B-lines in both resting and peak vasodilator stress.
Methods:
Dipyridamole stress echocardiography (SE) was conducted on 252 individuals (180 males, 71%, age 65 years ± 10 years) with chronic coronary syndromes. LAVI was quantified using the biplane disk summation method; LASr was obtained using 2-dimensional speckle tracking echocardiography; B-lines were evaluated through a simplified 4-site scan in the third intercostal space during lung ultrasound.
Results:
During SE, a reduction in LAVI (26 ml/m2 ± 14 ml/m2 vs. 24 ml/m2 ± 12 ml/m2, P < 0.001) and an increase in LASr from rest (33% ± 8% vs. 38% ± 10%, P < 0.001) were respectively observed from rest to stress. B-lines were increased significantly during SE, from 19 (7.5%) to 29 (11.5%), P < 0.001. A substantial, inverse linear correlation was identified between LAVI and LASr both at rest (r = –0.301, P < 0.001) and peak stress (r = –0.279, P < 0.001). At group analysis, peak B-lines showed a direct correlation with peak LAVI (r = 0.151, P = 0.017) and an inverse correlation with peak LASr (r = –0.234, P < 0.001). In individual assessments, 9.7% (20/207) of patients displayed stress B-lines with normal LAVI and preserved LASr, while 20% (9/45) exhibited stress B-lines with abnormalities in both LAVI and LASr.
Conclusions:
Vasodilator SE with combined left atrial and volume assessment, related to pulmonary congestion, is feasible with a high success rate. Pulmonary congestion is more frequent with dilated left atrium with reduced atrial contractile reserve (ClinicalTrials.gov identifier: NCT030.49995; NCT050.81115).
Costantina Prota ... Quirino CiampiPublished: February 26, 2024 Explor Cardiol. 2024;2:19–30
DOI: https://doi.org/10.37349/ec.2024.00018Aim:
Left atrial volume index (LAVI), left atrial reservoir function through left atrial reservoir strain (LASr), and B-lines in lung ultrasound serve as supplementary indicators of left ventricular filling pressures. This study analyzes the interrelation between LAVI, LASr, and B-lines in both resting and peak vasodilator stress.
Methods:
Dipyridamole stress echocardiography (SE) was conducted on 252 individuals (180 males, 71%, age 65 years ± 10 years) with chronic coronary syndromes. LAVI was quantified using the biplane disk summation method; LASr was obtained using 2-dimensional speckle tracking echocardiography; B-lines were evaluated through a simplified 4-site scan in the third intercostal space during lung ultrasound.
Results:
During SE, a reduction in LAVI (26 ml/m2 ± 14 ml/m2 vs. 24 ml/m2 ± 12 ml/m2, P < 0.001) and an increase in LASr from rest (33% ± 8% vs. 38% ± 10%, P < 0.001) were respectively observed from rest to stress. B-lines were increased significantly during SE, from 19 (7.5%) to 29 (11.5%), P < 0.001. A substantial, inverse linear correlation was identified between LAVI and LASr both at rest (r = –0.301, P < 0.001) and peak stress (r = –0.279, P < 0.001). At group analysis, peak B-lines showed a direct correlation with peak LAVI (r = 0.151, P = 0.017) and an inverse correlation with peak LASr (r = –0.234, P < 0.001). In individual assessments, 9.7% (20/207) of patients displayed stress B-lines with normal LAVI and preserved LASr, while 20% (9/45) exhibited stress B-lines with abnormalities in both LAVI and LASr.
Conclusions:
Vasodilator SE with combined left atrial and volume assessment, related to pulmonary congestion, is feasible with a high success rate. Pulmonary congestion is more frequent with dilated left atrium with reduced atrial contractile reserve (ClinicalTrials.gov identifier: NCT030.49995; NCT050.81115).
Special Issues The Effect of Sexual Dysfunctions, Peripheral Artery Disease, and Patient Education on the Cardiovascular Risk in Diabetes
The Effect of Sexual Dysfunctions, Peripheral Artery Disease, and Patient Education on the Cardiovascular Risk in DiabetesCarmine Gazzaruso Adriana Coppola
Submission Deadline: May 15, 2025
Published Articles: 0
 Exploring Exercise Cardiology: from Molecules to Humans
Exploring Exercise Cardiology: from Molecules to HumansPaulo Gentil
Submission Deadline: May 31, 2025
Published Articles: 1
 Cardiovascular Risk for Mothers and Offspring Resulting from Complicated Pregnancy
Cardiovascular Risk for Mothers and Offspring Resulting from Complicated PregnancyIlona Hromadnikova
Submission Deadline: June 30, 2025
Published Articles: 2
 Multimodality Imaging in Ischemic Heart Disease
Multimodality Imaging in Ischemic Heart DiseaseLeonardo Bolognese Maurizio Pieroni
Submission Deadline: June 30, 2025
Published Articles: 4
 Environmental Cardiology
Environmental CardiologyMaria Grazia Andreassi
Submission Deadline: June 07, 2025
Published Articles: 5
 Molecular Mechanisms of Cardiovascular Aging
Molecular Mechanisms of Cardiovascular AgingAndrea Borghini
Submission Deadline: June 07, 2025
Published Articles: 4
 Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coin
Common cardiovascular target for a wide gamut of contemporary health problems – thrombotic and arrhythmic sides of an inflammatory coinKarina Wierzbowska-Drabik
Submission Deadline: January 31, 2025
Published Articles: 6
From the Editor-in-Chief Exploration of Cardiology (EC) is a new open-access journal from Open Exploration publisher. The journal aims to provide, at this moment free of charge, an open forum for scholarly research on a range of topics. There are many good cardiology journals, with excellent editors, and still, one more journal may have a unique role in promoting research and debate in the new era of environmental cardiology and the obligatory quest for economic, legal, and environmental sustainability of cardiology practice. Healthcare money shortage and energy crisis, the pandemic pressure, climate change, and increasing evidence of environmental roots of cardiovascular disease pose new challenges to clinical cardiologists, researchers, and professional societies. Based on these principles, the EC will place a special emphasis on all techniques, methods, and practices promoting the development of ‘green’ (climate-neutral) and ‘blue’ (sustainable) cardiology. EC will publish Original Articles, Reviews, Protocols, Commentaries, Perspectives, and Editorials, and will also regularly publish special exploration issues to highlight advances at the cutting edge of research. I invite you to consider publishing your next paper with us and help us put EC in a prominent place in the cardiovascular editorial domains. As editor-in-Chief, I take a commitment to respecting the Author’s rights to fast and fair review and to do this in the best possible way with an inner team of associate editors who will work to serve our submitting authors, who are the real strength of any journal.Eugenio Picano
Exploration of Cardiology (EC) is a new open-access journal from Open Exploration publisher. The journal aims to provide, at this moment free of charge, an open forum for scholarly research on a range of topics. There are many good cardiology journals, with excellent editors, and still, one more journal may have a unique role in promoting research and debate in the new era of environmental cardiology and the obligatory quest for economic, legal, and environmental sustainability of cardiology practice. Healthcare money shortage and energy crisis, the pandemic pressure, climate change, and increasing evidence of environmental roots of cardiovascular disease pose new challenges to clinical cardiologists, researchers, and professional societies. Based on these principles, the EC will place a special emphasis on all techniques, methods, and practices promoting the development of ‘green’ (climate-neutral) and ‘blue’ (sustainable) cardiology. EC will publish Original Articles, Reviews, Protocols, Commentaries, Perspectives, and Editorials, and will also regularly publish special exploration issues to highlight advances at the cutting edge of research. I invite you to consider publishing your next paper with us and help us put EC in a prominent place in the cardiovascular editorial domains. As editor-in-Chief, I take a commitment to respecting the Author’s rights to fast and fair review and to do this in the best possible way with an inner team of associate editors who will work to serve our submitting authors, who are the real strength of any journal.Eugenio Picano
Editor-in-Chief of Exploration of Cardiology -
-
Selected Special IssuesTopic: The Effect of Sexual Dysfunctions, Peripheral Artery Disease, and Patient Education on the Cardiovascular Risk in Diabetes Topic: Exploring Exercise Cardiology: from Molecules to Humans Topic: Cardiovascular Risk for Mothers and Offspring Resulting from Complicated Pregnancy Topic: Multimodality Imaging in Ischemic Heart Disease Topic: Environmental Cardiology More