Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
Email: ggilligan@unc.edu.ar
ORCID: https://orcid.org/0000-0002-5201-1444
Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
ORCID: https://orcid.org/0000-0001-6427-1254
Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
ORCID: https://orcid.org/0009-0007-5768-9557
Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
ORCID: https://orcid.org/0000-0002-0881-9614
Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
ORCID: https://orcid.org/0009-0001-7263-1886
Affiliation:
Department of Oral Medicine, School of Dentistry, Universidad Nacional de Córdoba, Córdoba 5000, Argentina
ORCID: https://orcid.org/0000-0001-5955-1139
Explor Digit Health Technol. 2025;3:101136 DOI: https://doi.org/10.37349/edht.2025.101136
Received: June 29, 2024 Accepted: October 31, 2024 Published: January 10, 2025
Academic Editor: Gaurav Pandey, Icahn School of Medicine at Mount Sinai, United States
The article belongs to the special issue Digital Health Technologies for the Early Detection of Oral Cancer
Aim: The primary aim was to develop and test a telemedicine program for oral cancer screening by dentists in primary care. The secondary aim was to analyze the sensitivity of the provisional diagnosis compared to the definitive diagnosis.
Methods: A retrospective observational study that used telemedicine for oral cancer case detection was conducted in Cordoba, Argentina from 2018 to 2023, oral medicine specialists provided in-person training for dentists on the clinical recognition and early diagnosis of oral squamous cell carcinoma (OSCC) and oral potentially malignant disorders (OPMD), and telemedicine use for the early detection of oral cancer. The trained professionals conducted opportunistic screenings in their workplaces. When encountering a suspicious lesion on the oral mucosa, they collected relevant patient data and clinical photographs of the lesion, sharing these with the reference center. The specialized center was based at the Oral Medicine unit at the Facultad de Odontología, Universidad Nacional de Córdoba, Argentina. The specialists suggested radiographic examinations and/or pre-surgical laboratory tests and, if necessary, expedited referral to the specialized center for in-person assessment and definitive diagnosis.
Results: Cases with clinical suspicion of OSCC and OPMD were referred to the reference center. In all cases, the definitive diagnosis was obtained within less than 1 month. Eleven out of 12 cases of OSCC were diagnosed within 2 weeks, with only 1 case diagnosed at 1 month due to some patient delay. The concordance between the clinical suspicion at the time of teleconsultation and the definitive diagnosis of OSCC by the specialists was absolute (Kappa test, coefficient 1), with a sensitivity and specificity of 100%.
Conclusions: Integrating telemedicine with other preventive strategies and timely referral to oral medicine specialists could potentially decrease diagnostic delays in OSCC and OPMD.
Several studies indicate that the early diagnosis of oral squamous cell carcinoma (OSCC) is the most important prognostic factor for overall survival, and when these tumors are diagnosed and treated at earlier stages, survival rates are close to 80% [1, 2]. There are different causes of delay in the diagnosis of OSCC. One of them is professional delay, which refers to the period between the first consultation with a healthcare professional and the consultation with the specialist who performs the biopsy. Morelatto et al. [2] showed in their studies that professional delay fluctuated in two periods of evaluation between 2.9 months to 1.34 months [3].
There are different strategies to reduce the time associated with professional delay. These include continuous training of professionals, the creation of diagnostic networks linking general dentists with specialized oral medicine centers, and the use of telemedicine (TM) [4–7].
The term “TM” is used to refer to the use of information-based technology and communication systems. It enables access to healthcare in hard-to-reach areas or regions far from specialized pathology health centers [8]. TM is a resource that could reduce the delay in referrals to specialists, as direct communication with specialized professionals speeds up the referral process and, therefore, the initial presumptive diagnosis. This approach even allows for the request of specific analyses based on the disease (imaging, laboratory tests, etc.). Remote areas often have limited healthcare personnel trained to diagnose OSCC, and are geographically difficult to access, due to adverse climatic conditions and rough terrain. In this context, there are recent reports that TM for oral lesions (TMO) has been introduced in academic medical centers, community hospitals, rural hospitals, and even between hospitals in different countries [9, 10].
The risk of OSCC is influenced by multiple factors that can vary according to socioeconomic and geographical conditions [11, 12]. In the province of Córdoba, Argentina, there are regions with a high incidence of cancer, including OSCC [13]. These towns are 150 km to 300 km away from the specialized oral cancer diagnosis center. These groups, considered at high risk for the development of OSCC (e.g., in areas with increased arsenic levels in drinking water), require active and specific preventive strategies to achieve early diagnoses. The aim of this study was to develop and test a TM program for oral cancer screening by dentists in primary care. The secondary aim was to analyze the sensitivity of the provisional diagnosis compared to the definitive diagnosis of OSCC and oral potentially malignant disorders (OPMD) among the cases consulted via TMO (through an opportunistic screening and professional training strategy).
A retrospective observational study was conducted from 2018 to 2023, which included cases consulted via TMO at the specialized Oral Medicine Reference Center (RC), located in the Oral Medicine Service of the Facultad de Odontología, Universidad Nacional de Córdoba, Argentina. The study was approved by the Health Ethics Committee of the Facultad de Odontología, Universidad Nacional de Córdoba (protocol number T11/16).
During 2018, 2019, 2021, and 2022, oral medicine specialists from the RC traveled to six geographical zones in the province of Córdoba, Argentina, to provide in-person training for the local dentists on the clinical recognition and early diagnosis of OSCC and OPMD. Additionally, they trained them on teleconsultation modalities, the scope of digital diagnostic tools, and photographic documentation using smartphones. This specific 4-hour training pack included one hour of advice on programming smartphone cameras to obtain clinical photos and consultation protocol modalities for cases of suspected OSCC and OPMD via TMO. The specific training on these topics was conducted by professionals with postgraduate degrees in Oral Medicine, university professors from our diagnostic center, and those involved in research tasks in the field of oral cancer. The training consisted of 45-minute classes, completing a total of 4 h of theoretical activity, where the main concepts of the aforementioned topics were covered. Regarding the training on how to take photographs with the available smartphones, a hands-on session was conducted, allowing participants to practice at the same time. The other two hours provided detailed information on oral manifestations of OSCC and OPMD, relevant risk factors to be recorded through the anamnesis, and the diagnosis and referral sequence of these lesions if found. Likewise, one hour was allocated to training in clinical recognition of other prevalent benign oral conditions in our setting: medication-related osteonecrosis and sexually transmitted infections. Additionally, special training was provided on how to record the most important oral cancer risk factors in our population during patient anamnesis. In each case consulted by TMO, clinical concepts previously trained were reinforced, in the form of virtual tutoring.
Subsequently, six TM networks were established using the free WhatsApp application, consisting of trained and qualified professionals from each region and two specialists in Oral Medicine at the RC (Oral Medicine Department, Facultad de Odontologia UNC). The details of the TMO groups formed are shown in Table 1.
Characteristics of oral telemedicine groups
| Location | Distance to RC | Number of trained dentists | Year of training | Cases consulted by TMO |
|---|---|---|---|---|
| Traslasierra | 200 km | 27 | 2022 | 36 |
| Northern Cordoba | 150 km | 20 | 2022 | 5 |
| Bell Ville | 225 km | 45 | 2018, 2022, 2023 | 118 |
| Villa Maria | 165 km | 12 | 2022 | 12 |
| Las Varillas | 185 km | 30 | 2019 | 54 |
| Marcos JuárezCorral de Bustos | 310 km | 46 | 2018, 2023 | 72 |
| Total/Mean | 205.83 km | 180 | - | 297 |
RC: reference center; TMO: telemedicine for oral lesions
All data for this study were extracted from the digital records of the teleconsultation groups on the free messaging application (WhatsApp). The trained dentists conducted opportunistic screenings in their workplaces (private practices or public health centers). When encountering a lesion on the oral mucosa, they collected relevant patient data and clinical photographs of the lesion, following the photographic documentation protocol (available from the authors on request) proposed during the training sessions. This information was shared in the teleconsultation groups for each geographic area. Upon receiving a teleconsultation for any of these lesions, the specialists suggested additional investigations (radiographic examinations and/or pre-surgical laboratory tests) and, if necessary, expedited referral to the specialized RC for in-person assessment to reach a definitive diagnosis.
The variables analyzed in the teleconsulted cases were presumptive and definitive diagnosis; and for OSCC cases, the delay time from the teleconsultation to the definitive diagnosis.
The prevalence of OSCC and OPMD was expressed in absolute and relative frequencies. The statistical analysis to assess the concordance between the suspected diagnosis of malignant or premalignant lesion and the histopathological diagnosis was performed using the Kappa test, as well as by the sensitivity and specificity of the diagnosis made by dentists in primary care facilities. Kappa coefficient was categorized with a numerical range representing the degree of consistency into < 0.4: fair; 0.4–0.6: moderate; 0.6–0.8: substantial; and > 0.8: almost perfect. P-values below 0.05 were regarded as statistically significant. Statistical analysis was performed using Epidat 4.2 software.
Table 1 lists the demographic features of the networks established for the study. During the period covered by the records, teleconsultations were received for 297 cases (402 clinical images), distributed among six groups of trained professionals. All cases included the sending of at least one clinical photograph. Of this total, 12 were referred with the clinical suspicion of OSCC and 11 of OPMD. The remaining 274 cases were those with presumptive diagnoses other than OSCC and OPMD, including syphilis, reactive lesions, oral histoplasmosis, aphthous ulcers, fibrous hyperplasias, and chronic traumatic ulcers. Each diagnosis was subsequently confirmed through appropriate procedures such as biopsy or serological tests.
Cases with clinical suspicion of OSCC and OPMD were referred to the RC with all pre-surgical data for biopsy procedures. Eleven out of the twelve cases suspected of OSCC attended the referral center within one week, with histopathological confirmation of OSCC achieved within two weeks. The remaining case experienced a delay attributable to the patient, who attended three weeks after referral, with one month after the initial consultation. Among the suspected malignancies, 10 out of 12 cases were conventional OSCC, 1 case was carcinoma in situ, and 1 case was verrucous carcinoma. Among the 11 cases diagnosed as OPMD, 3 cases were proliferative verrucous leukoplakia, 1 case of erythroplakia, 1 case of oral lichen planus, 4 lichenoid lesions, and 2 actinic cheilitis cases were diagnosed (Figure 1). The breakdown of OSCC and OPMD cases diagnosed within each trained professional group is shown in Table 2.
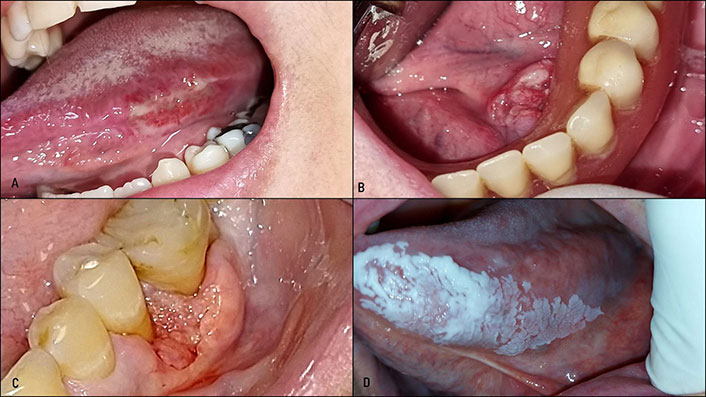
Example of cases consulted by telemedicine. Photographs were taken by dentists previously trained and certified for clinical photography with smartphones. A: ulcerated lesion on the lateral tongue border where the referring professional noted an indurated ulcer. The patient was promptly referred to the referral center where a well-differentiated OSCC was diagnosed. B: female patient without risk factors, promptly referred to the specialized center over 300 km away from the referral center. Biopsy revealed T2N0M0 OSCC. Following surgery, after 3 years of follow-up, remains alive. C: male patient with a non-healing gingival lesion. The consulting dentist was a periodontist with training in Oral Medicine. The patient was promptly treated for a moderately-differentiated OSCC. D: patient of low socioeconomic status who presented at a primary care center. The dentist, previously trained, took the photograph. The patient was promptly referred to the specialized center where a diagnosis and treatment for proliferative verrucous leukoplakia was performed. In all cases, presumptive diagnoses were made by referring professionals and matched the definitive diagnosis
Detail of OSCC, OPMD, and other diagnosis according to groups of trained dentists
| Group | Patients (n) | OSCC | OPMD | Other oral conditions (not referred to under OSCC or OPMD category) |
|---|---|---|---|---|
| Traslasierra | 36 | 1 tongue SCC1 lip SCC | 1 actinic cheilitis | 33 cases: oral histoplasmosis, oral syphilis, pyogenic granuloma, pemphigus vulgaris, cutaneous keratin horn, condyloma acuminate, fibrous hyperplasias |
| Northern Cordoba | 5 | None | 1 lichenoid | 4 cases: fibrous hyperplasias, medication-related osteonecrosis, benign migratory glossitis |
| Bell Ville | 118 | 2 floor of mouth SCC1 gum SCC1 lip SCC1 buccal mucosa VC1 buccal mucosa CIS | 1 PVL1 erythroplakia1 OLP1 actinic cheilitis | 108 cases: melanotic macule, irritative hyperplasia, pyogenic granuloma, lipoma, syphilis, hemorrhagic bullous angina, juvenile spongiotic gingival hyperplasia, condyloma acuminata, squamous papilloma, chronic traumatic ulcer |
| Villa Maria | 12 | 1 lip SCC | None | 11 cases: fibrous hyperplasia, condyloma acuminata, candidasis, medication-related osteonecrosis. osteopetrosis (Albers Schömberg disease) |
| Las Varillas | 54 | None | 2 lichenoid1 PVL | 51 cases: mucoid-cysts, benign migratory glossitis, pyogenic granuloma, herpes labialis, oral syphilis, aphthous ulcers, chronic traumatic ulcer, gingival fibrous hyperplasias. |
| Marcos JuárezCorral de Bustos | 72 | 2 tongue SCC1 gum SCC | 1 PVL1 lichenoid | 67 cases: chronic traumatic ulcer, ranula, torus, medication-related osteonecrosis, gingival fibrous hyperplasias, ulcerative necrotic gingivitis, benign migratory glossitis, oral syphilis, crest syndrome, thrombocytopenic purpura, mucoid cyst |
| Total (%) | 297 | 12 (4%) | 11 (3.7%) | 274 (92.3%) |
OSCC: oral squamous cell carcinoma; OPMD: oral potentially malignant disorders; VC: verrucous carcinoma; CIS: in situ carcinoma; PVL: proliferative verrucous leukoplakia; OLP: oral lichen planus
Of the 12 OSCC cases, 11 were diagnosed at early stages (TIS, T1, and T2), while only one was a gingival OSCC measuring less than 4 cm but with bone involvement (diagnosed as OSCC T4a).
The concordance between the clinical suspicion at the time of teleconsultation and the definitive diagnosis was absolute (the Kappa test yielded a value of 1, which corresponds to the “almost perfect” criterion. The P-value of the Kappa test was P < 0.001), with a sensitivity and specificity of 100%.
TMO in the context of oral cancer control has proven to be effective and widely accepted for delivering cancer education through phone messaging and medical data transfer [14, 15]. The tool has been well-received due to its immediate access, reduced waiting times for specialist communication, cost savings (e.g., saving travel expenses for hospital visits), and prompt accessibility to specialized referrals and multidisciplinary treatment planning. During the COVID-19 pandemic use of TM enhanced communication between primary and specialist care for the diagnosis of malignancies [16]. Specific training in telehealth is essential to ensure optimal oral cancer care through TMO. While established virtual referral centers for OSCC and OPMD exist in some countries, disparities in usage across nations have hindered widespread implementation [17]. The combination of TM and specialized training for local dentists in hard-to-reach areas in topics related to OPMD and OSCC offered multiple advantages. The most important is the rapid referral of suspected cases, which reduces delays. TM enabled access to specialists in real-time, regardless of geographic location, improving coverage and reducing barriers to early diagnosis. On the other hand, prior training ensured that dental professionals are equipped with the necessary skills and competencies to identify early or suspicious signs of oral cancer, increasing the accuracy of initial diagnoses and empowering dentists who lack postgraduate training in Oral Medicine. This synergy optimized health resources, shortened referral times, and promoted earlier and more effective interventions, potentially improving patient outcomes. Although there are studies that address these topics, none have reflected the combination and joint implementation of both tools. In our case, this integrative approach to strategies for the early referral of patients with suspected oral cancer resulted in a highly advantageous experience.
Warnakulasuriya and Kerr [7] have highlighted several conditions that need to be satisfied in planning opportunistic screening for oral cancer prevention. These include the need for specific training of screening personnel having access to specialists to confirm and manage positive detections and improving compliance to screening and referral. To address these requirements, the authors have adopted the provision of appropriate training, particularly in OSCC detection, the development of toolkits and e-learning modules for screener training, the establishment of national practice-based networks for data collection, and we propose the creation of risk prediction models for the use in primary care to assess risk profiles. Building on the advantages of TMO, we have developed a model for early diagnosis of OSCC and OPMD that integrates opportunistic screening strategies with TMO in real-world settings. This study has considered the limitations and recommendations related to opportunistic screening. Our research was not solely based on examinations conducted in private dental offices but also included dental clinics in primary health care centers, thereby enhancing access for low-income patients. Most participating dentists were recent graduates who completed a one-year Oral Medicine course during their undergraduate studies, with weekly theoretical and clinical training. The workforce employed was appropriately trained through postgraduate courses supported financially by governmental and professional institutions. Specific training included instruction on capturing clinical photographs using smartphones as an adjunct tool for screening activities. Furthermore, our approach acknowledges that the primary risk factor for OSCC is not singular but rather the accumulation of various factors [18].
Classically, the feasibility of different screening methods for OSCC and OPMD is evaluated, yet the impact of these preventive models on diagnostic accuracy and delays remains unexplored in the literature [19]. Based on the training given to dentists for the detection of OSCC and OPMD involving a combination of opportunistic screening and TMO, we have achieved not only complete agreement between presumptive and definitive diagnoses of OSCC but also timely final diagnoses without delay. To the best of our knowledge, we have not found prevention models combining the aforementioned strategies. Some studies have assessed the agreement of presumptive diagnoses made by referring professionals with those issued by specialists at the referral center [20]. The inter-observer agreement was consistently above 0.6 in all cases. Regarding histopathological diagnosis, they achieved an average sensitivity exceeding 80% and specificity of 71% [14, 21]. However, none of them achieved absolute agreement of 100% sensitivity and specificity as found in our results.
The absolute agreement between presumptive and definitive diagnoses in this study, as well as the prompt issuance of definitive diagnoses, could be attributed to several factors. These include the prior training of referring professionals (screeners) in both recognizing the clinical manifestations of OSCC and OPMD and capturing appropriate photographs by dentists for remote consultation with the RC. Additionally, the interaction between screeners and specialists facilitates the formulation of presumptive diagnoses, which justifies rapid referral. Moreover, this referral process is optimized by the recommendations provided by the RC to the referring professionals.
The strategy described in this study is not the only alternative for detecting oral lesions through TMO, that require referral to a specialized center. Digital applications like the MEMOSA app developed by Cancer Research Malaysia facilitate the collection of clinical data and images for the referring dentist, enabling professionals with less training in oral medicine to detect suspicious lesions for malignancy [22]. However, its availability is limited to a few countries in the region and not accessible worldwide.
Our study had a major limitation. The records sustained by the referring dental professionals did not encompass all reviewed patients, thus the frequency of lesions diagnosed through opportunistic monitoring remains unknown. Consequently, it precludes comparison of TMO effectiveness with the detection and exclusion of benign mucosal lesions. Furthermore, another important limitation to highlight is the lack of available data on patient survival, which made it impossible to evaluate the impact of this integrative strategy on oral cancer mortality in our population.
Our findings, along with the integrative approach combining TMO and opportunistic screening for early diagnosis of OSCC and OPMD, should be further investigated and replicated in other geographic regions with similar demographic characteristics (risk factors for oral cancer, access to qualified specialists in Oral Medicine, etc.). Future studies should also focus on digitizing databases to optimize the recording of TMO variables and systematically evaluate the impact of this dual approach on patient outcomes, rigorous follow-up protocols performed by TM, treatment modalities, final malignancy staging, and 5-year morbidity and mortality rates. Additionally, a multicenter study involving Latin American institutions could significantly contribute to expanding the evidence base for this innovative strategy. The methodology of this project could also be extended to the prevention and early diagnosis of other rising oral conditions, such as sexually transmitted infections [23].
In conclusion, TMO demonstrates benefits in early diagnosis of OSCC. Integrating TMO with other strategies, such as training for referring professionals, and rapid referral of cases showing agreement with specialist opinion based on the transferred clinical images could potentially decrease diagnostic delays in OSCC and OPMD. This reduction in delay times may result in improving the prognosis of patients diagnosed with oral cancer.
OPMD: oral potentially malignant disorders
OSCC: oral squamous cell carcinoma
RC: Reference Center
TM: telemedicine
TMO: telemedicine for oral lesions
GG: Conceptualization, Investigation, Validation, Funding acquisition, Writing—original draft, Writing—review & editing. RP: Funding acquisition, Writing—original draft, Writing—review & editing. MFGC and JCRP: Investigation, Writing—original draft. JL: Investigation. EP: Investigation, Validation, Writing—original draft, Writing—review & editing, Supervision. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study was conducted within the framework of a doctoral thesis approved by the Health Ethics Committee of the Facultad de Odontología, Universidad Nacional de Córdoba (protocol number T11/16).
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
The datasets analyzed for this study can be found in the Oral Medicine Department archive (Facultad de Odontología, Universidad Nacional de Córdoba, Argentina).
The free training courses (regarding Oral Cancer and Oral Potentially Malignant Disorders as well as Telemedicine for the early detection of Oral Cancer) for referring professionals from several geographical areas of the Province of Córdoba, Argentina, were funded by the Colegio Odontológico de Córdoba, Argentina, Continuing professional training program [337/1997]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Xin-Jia Cai
Eduardo D. Piemonte ... Jerónimo P. Lazos
Kehinde Kazeem Kanmodi ... Jacob Njideka Nwafor
Romina Andrian ... Gerardo Gilligan
Caique Mariano Pedroso ... Alan Roger Santos-Silva
Márcio Diniz-Freitas ... Pedro Diz-Dios
Simon A. Fox, Camile S. Farah
Constanza B. Morales-Gómez ... Víctor Beltrán
Anna Luíza Damaceno Araújo ... Alan Roger Santos-Silva
