Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
1Department of Medicine, Dow University of Health Sciences, Karachi 74000, Pakistan
†These authors contributed equally to this work.
Affiliation:
2Research Institute for Collaborative Development, Kathmandu 44600, Nepal
†These authors contributed equally to this work.
Email: iambibekgiri@gmail.com
ORCID: https://orcid.org/0009-0003-0100-9111
Explor Drug Sci. 2024;2:867–874 DOI: https://doi.org/10.37349/eds.2024.00078
Received: August 02, 2024 Accepted: October 31, 2024 Published: December 03, 2024
Academic Editor: Fernando Albericio, University of KwaZulu-Natal, South Africa; Universidad de Barcelona, Spain
The FDA’s approval of resmetirom (Rezdiffra) marks a significant breakthrough in treating metabolic dysfunction-associated steatohepatitis (MASH) and fibrosis, conditions linked to non-alcoholic fatty liver disease (NAFLD). MASH is a growing global health concern, and resmetirom offers a novel therapeutic option by targeting liver pathophysiology through thyroid hormone receptor-beta activation. This mechanism effectively reduces fibrosis markers, improves liver enzyme levels, and minimizes liver fat buildup. Clinical trials have shown that resmetirom has a favorable safety profile, with manageable side effects like diarrhea and nausea. Additionally, it may lower cardiovascular risks associated with MASH, enhancing patient outcomes and quality of life. As the first FDA-approved drug for MASH, resmetirom’s introduction fills a crucial treatment gap, providing new hope for millions of patients and representing a pivotal moment in hepatology.
On March 14, 2024, the United States Food and Drug Administration (FDA) approved resmetirom (marketed as Rezdiffra) for the treatment of adults with a noncirrhotic liver condition called “metabolic dysfunction-associated steatohepatitis (MASH)” [1]. It is used along with diet and exercise in treating MASH with moderate to advanced liver fibrosis (Figure 1) [1].
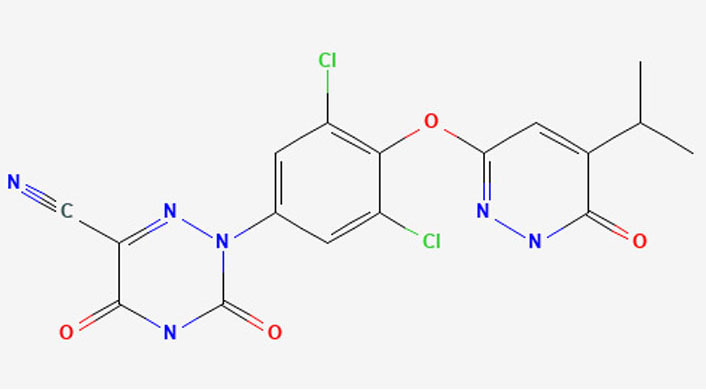
Chemical structure of resmetirom. 2D structure image of resmetirom (SID 163642907) reprinted from https://pubchem.ncbi.nlm.nih.gov/substance/163642907#section=2D-Structure
MASH falls within the spectrum of metabolic dysfunction-associated steatotic liver disease (MASLD), also known as “non-alcoholic fatty liver disease (NAFLD)”. MASH represents a severe subset of NAFLD, characterized by inflammation and hepatocyte injury, often accompanied by hepatic fibrosis [2]. The heterogeneity of MASH underscores its multifactorial nature, where genetic predispositions, environmental factors, and concurrent health conditions collectively contribute to the advancement of fibrosis in specific individuals. Fibrosis ultimately serves to be an important predictor for clinical outcomes [3].
Globally, the prevalence of MASH stands at approximately 5%, however, in individuals with type 2 diabetes mellitus (T2DM), the prevalence rises to about 37.3%, while among those who are overweight or obese, it is estimated to be about 33.5% [4]. According to Markov modeling, it is projected that by 2030, roughly 100.9 million individuals will be affected by NAFLD, and about 27.0 million people will have progressed to MASH, exhibiting different degrees of fibrosis [5]. It was also found that the prevalence of MASH increases with obesity [6]. When MASH progresses further, it can lead to cardiovascular disease (CVD). CVD is proposed to be the leading cause of death in patients with MASH [7]. Thus, it is important to know the disease mechanism as it causes great hazards to human health. This will also help us to understand why resmetirom has been approved as the first drug for treating MASH and associated fibrosis.
The pathophysiology underlying the development of MASH is multifaceted. It primarily stems from the excessive load of free fatty acids delivered to the liver, alongside increased lipogenesis [8, 9]. The liver employs a vital pathway to either store or process these fatty acids, primarily through beta-oxidation, facilitated by mitochondria. Additionally, it re-esterifies them into triglycerides for storage [9]. When these mechanisms become overwhelmed, they can lead to the generation of lipotoxic molecules, which exacerbate stress within the endoplasmic reticulum. This stress triggers the production of oxidants and activates inflammasomes [10]. As the liver becomes increasingly burdened by these stressors, its cells undergo apoptosis, triggering the recruitment of inflammatory cells. Simultaneously, hepatic stellate cells are activated, promoting fibrosis and exacerbating the transition from NAFLD to the more severe stage of MASH [11]. As fibrosis plays a crucial role in predicting clinical outcomes [12, 13], improvement in fibrosis has emerged as a significant surrogate endpoint in MASH clinical trials.
Thyroid hormone (TH) is considered to have a pivotal role in hepatic triglyceride and cholesterol metabolism [14]. Hypothyroidism is regarded as being one of the causes of fatty liver and thus treating TH metabolism results in the betterment of steatohepatitis [15, 16]. These effects of TH are exerted through thyroid hormone receptor-beta (THR-β) activation which is the isoform of thyroid hormone receptors that is found predominantly [14]. TH influences hepatic lipid metabolism by regulating the transcription of target genes involved in lipid balance pathways, such as lipogenesis, beta-oxidation, autophagy, and cholesterol metabolism [14]. Within the liver, deiodinase type 1 (DIO1) plays a crucial role in converting the prohormone thyroxine (T4) into the biologically active hormone triiodothyronine (T3). Interestingly, in an early model of MASH, there is an observed increase in both the levels and activity of DIO1. This suggests a compensatory mechanism aimed at handling the excess lipid accumulation associated with MASH [17]. In a recent systematic review with meta-analysis conducted by Mantovani et al. [15], a notable association was observed between hypothyroidism and both the presence and severity of NAFLD. During chronic liver injury, it is believed that intrahepatic thyroid hormone signaling may become compromised [18]. This impairment could decrease the conversion of T4 to active T3 by DIO1 while increasing the conversion of T4 to inactive reverse triiodothyronine (rT3) by deiodinase type 3 (DIO3). Consequently, this could lead to the buildup of lipotoxic substances, initiating a cycle of recurrent liver injury [19].
Regarding treatment options, following a hypocaloric diet and achieving weight loss have been found to decrease overall body fat, visceral fat, and fat stored in the liver [19]. Prior to the approval of resmetirom, there were no FDA-approved pharmacological treatments available [20].
A recent observational study involving 32 obese patients with diabetes mellitus who underwent Duodenal-Jejunal Bypass Liner (DJBL) demonstrated improvements in non-invasive markers of steatosis and MASH, though not in fibrosis. However, the precise impact of DJBL on NAFLD warrants further investigation [21].
Selonsertib was also tested, but it did not demonstrate any enhancement or resolution of MASH [22]. Glucagon-like peptide 1 (GLP-1) agonists have been experimented with as well. MASH resolution was observed in 39% of patients treated with liraglutide for 48 weeks and in 59% of those receiving semaglutide for 72 weeks [23, 24]. However, there was no significant improvement in fibrosis in either study. In the Phase IIb aramchol for the resolution of steatohepatitis (ARREST) trial, aramchol [a liver-targeted stearoyl coenzyme A desaturase-1 (SCD-1) inhibitor] at 600 mg did not significantly reduce liver fat content. However, improvements in liver histology and biochemical markers suggest its potential for treating MASH and fibrosis [25].
Sobetirome (GC-1) and eprotirome (KB2115) were the first THR-β agonists shown in preclinical models to decrease intrahepatic lipid levels [26, 27]. However, their trials were halted because of their side effects like cartilage damage in eprotirome and hyperglycemia in sobetirome.
Resmetirom (MGL-3196) is a liver-targeted oral agonist of THR, with about 28-fold greater selectivity for THR-β over THR-α than triiodothyronine [28]. It causes reduction in hepatic fat accumulation by activating THR-β [1]. Additionally, it decreases the level of liver enzyme, enhances non-invasive indicators of liver fibrosis, and reduces stiffness of the liver. Simultaneously, it demonstrates a positive cardio-metabolic effect by decreasing low-density lipoprotein (LDL) cholesterol levels [29, 30].
The investigators highlighted that resmetirom’s safety and tolerability were favorable, indicating that treatment-emergent adverse events (TEAEs) were noted in 86.5–86.1% of individuals administered 100 mg of resmetirom and in 88.4% of those allocated to 80 mg of resmetirom, contrasted with 81.8% of those given the placebo [30]. Secondly, in a Phase 3 randomized controlled trial [31], MASH resolved with no worsening of fibrosis in 25.9% of the patients in the 80 mg resmetirom and 29.9% in the 100 mg groups. Fibrosis improved by at least one stage with no worsening of the NAFLD activity score among 24.2% of the patients in the 80 mg resmetirom groups and 25.9% in the 100 mg group.
After daily dosing, it takes 3 days to 4 days to reach a steady state concentration [32]. The median time to achieve maximum plasma concentration is around 4 hours which happens with multiple daily doses of 80 mg or 100 mg [32]. Resmetirom pharmacokinetics remained consistent with a high-fat meal, showing a 33% decrease in maximum concentration (Cmax), an 11% decrease in area under the concentration-time curve (AUC), and a delay in the median time it takes for a drug to reach its maximum concentration (Tmax) by about 2 hours compared to fasting [32]. Resmetirom has a plasma half-life (t½) of 4.5 hours and a steady-state clearance (CL/F) of 17.5 L/h (56.3%) [32]. After oral administration, about 67% of the dose is recovered in feces and 24% in urine. Unchanged resmetirom is not detected in feces and accounts for 1% of urine [32].
Resmetirom is a liver-directed drug and its effects are mediated through THR-β variety [28]. Its liver targeting is attributed to its absorption facilitated by liver-specific organic anion transporting polypeptides 1B1 [33]. In individuals with MASH, there is a reduction in liver THR-β signaling, which impacts lipid metabolism, fatty acid oxidation, and energy production, potentially exacerbating MASH and fibrosis [14]. In MASH, lipotoxicity induces intrahepatic hypothyroidism, reducing T4 to active T3 conversion and favoring rT3 production [2, 33]. Resmetirom aims to address this fundamental pathophysiology in MASH patients [30]. Resmetirom significantly reduced rT3 levels by week 52 compared to placebo, enhancing the FT3/rT3 ratio, indicating normalized liver thyroid hormone function in both thyroxine-treated and euthyroid patients [30]. Resmetirom does not affect the more widely distributed THR-α receptor [30].
The recommended resmetirom dose depends on the patient’s weight: for those under 100 kg (220 lbs.), it’s 80 mg daily, and for those at or above 100 kg (220 lbs.), it’s 100 mg daily [34].
Resmetirom, administered at 80 mg and 100 mg once-daily doses over 52 years, was well tolerated [30]. There were no significant increases in serious TEAEs, nor were there notable imbalances in specific serious TEAEs observed in the resmetirom groups compared to the placebo [30]. Resmetirom demonstrated improvements in liver enzymes, fibrosis biomarkers, and imaging tests compared to the placebo [30].
When administered alongside moderate cytochrome P450 2C8 (CYP2C8) inhibitors like clopidogrel, resmetirom showed increased Cmax by 1.3-fold and AUC by 1.7-fold. Pioglitazone’s AUC rose by 1.5-fold when combined with resmetirom. Simvastatin’s Cmax and AUC increased by 1.4-fold and 1.7-fold, respectively, with resmetirom. Pravastatin’s Cmax and AUC increased by 1.3-fold and 1.4-fold, respectively. Atorvastatin’s AUC rose by 1.4-fold; atorvastatin lactone’s Cmax and AUC increased by 2.0-fold and 1.8-fold, respectively. No clinically significant changes were observed in the pharmacokinetics of R-warfarin or S-warfarin when co-administered with resmetirom.
The primary side effects commonly observed with resmetirom are diarrhea and nausea [1]. Serious side effects include hepatotoxicity and gallbladder problems [35]. Apart from these effects, it can also cause dizziness, itching, pain in the stomach, and constipation [35].
Endocrine conditions such as polycystic ovary syndrome (PCOS), hypothyroidism, hypogonadism, and deficiency of growth hormone may also cause NAFLD [36, 37], putting additional emphasis on the need for more research in understanding the use of resmetirom in the treatment of secondary NAFLD or MASH, particularly in conjunction with treatment regimens for the primary endocrine diseases as well as lifestyle modifications. In turn, resmetirom could help open up an entirely new class of drugs that potentially targets the intricate linkage between NAFLD and common endocrine diseases.
The approval of resmetirom marks a significant milestone in the treatment of MASH, offering a new pharmacological option for patients with moderate to advanced fibrosis [1]. Its ability to reduce hepatic fat accumulation, improve liver function, and mitigate life-threatening cardiovascular risks associated with MASH marks a substantial breakthrough, promising a brighter future for those afflicted by this debilitating condition [7]. However, with an annual wholesale acquisition cost of $47,400 [38], the treatment will not be accessible for the majority of those with socioeconomic difficulties. For this purpose, it would be prudent to explore tiered pricing as well as collaborations and patient assistance programs in order to increase access and ensure equitable treatment outcomes for all patients.
AUC: area under the concentration-time curve
Cmax: maximum concentration
CVD: cardiovascular disease
DIO1: deiodinase type 1
DJBL: duodenal-jejunal bypass liner
FDA: Food and Drug Administration
MASH: metabolic dysfunction-associated steatohepatitis
NAFLD: non-alcoholic fatty liver disease
rT3: reverse triiodothyronine
T3: triiodothyronine
T4: thyroxine
TEAEs: treatment-emergent adverse events
TH: thyroid hormone
THR-β: thyroid hormone receptor-beta
MMA, SM, MM, MH, FL, and SA: Data curation, Investigation, Conceptualization, Methodology, Writing—original draft. BG: Investigation, Project administration, Resources, Supervision, Visualization, Writing—review & editing. All authors have equal contributions to this study, and they have approved the final version of this manuscript.
The authors declare that they have no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
