Abstract
C1q nephropathy is a rare glomerular disease. Clinical presentation is diverse and ranges from asymptomatic hematuria or proteinuria to symptoms and signs of nephrotic/nephritic syndrome. On light microscopy, it can be classified into two subtypes: minimal change disease (MCD)/focal segmental glomerulosclerosis (FSGS) group and immune complex mediated proliferative glomerulonephritis group. A case of a 19-year-old male patient presenting nausea and decreased appetite will be reported. The labs showed severe nephrotic syndrome and a progressive kidney injury over a few months that were never diagnosed. The immune workup came back negative. The patient mentioned that he was taking protein shakes a few months earlier for bettering his physical fitness. A renal biopsy was done and showed a major reduction in renal mass and C1q nephropathy. He received steroids without any improvement. He was started on hemodialysis afterward then got transplanted 8 months later. In front of this rapid deterioration, FSGS might be the underlying etiology rather than MCD. Further studies are warranted to establish a connection between protein supplements, and progression of kidney disease.
Keywords
C1q nephropathy, kidney failure, kidney biopsyIntroduction
First detailed by Jennette and Hipp [1] in 1985, C1q nephropathy is a rare glomerular disease that may cause steroid-resistant nephritic/nephrotic syndrome in older children and younger adults. Its definition is histological. On light microscopy, it can be classified into two subtypes: minimal change disease (MCD)/focal segmental glomerulosclerosis (FSGS) group and immune complex mediated proliferative glomerulonephritis (GN) group [2]. Note that electron microscopy and immunofluorescence studies have more specificity [1, 2]; they can detect the presence of extensive mesangial deposition of C1q and associated immune complexes [3]. Exclusion criteria include the absence of clinical or immunological features of systemic lupus erythematosus (SLE) and type 1 membranoproliferative GN (MPGN) [2, 3]. The patient may present with asymptomatic hematuria or sub-nephrotic proteinuria, hypertension (35%) and renal insufficiency (5–46%) at time of diagnosis [2]. In addition to that, some cases of end stage renal disease requiring renal replacement therapy have also been reported [4]. Treatment consists of steroids as first line or immunosuppressive therapy as a second option [5].
Case report
The patient was a 19-year-old man, non-smoker, non-alcoholic, known to have hypothyroidism (diagnosed one year prior to presentation) on levothyroxine who presented with recurrent nausea and decreased appetite. Six months prior to presentation, he was admitted to the hospital for gastroenteritis, when he was found to have mildly elevated creatinine (1.5 mg/dL) and a trace of proteins in urine which were attributed to dehydration. No further investigations nor follow-ups were done. The patient also mentioned that he was taking protein shakes as supplements for bettering his physical fitness few months before his gastroenteritis. No other drugs were mentioned. Since then, the patient had a decreased appetite leading to gradual weight loss, which lead him to visit our clinic. Upon presentation, he was normotensive, not tachycardic and afebrile. No headache, eye problems, dysphagia, vomiting, chest pain or dyspnea was noted. Furthermore, there was no history of arthralgia, jaundice, rashes, oral ulcers, or edema. There was no family history of any illness. On physical examination, a pale skin, clear lungs, soft abdomen with no organomegaly no ascites and no lower limb edema were found. Laboratory tests done showed (Tables 1 and 2):
Laboratory tests
| Labs | Values | Labs | Values |
|---|---|---|---|
| Hemoglobin | 10.3 g/dL | Bicarbonates | 23.8 mEq/L |
| Hematocrit | 32% | Calcium | 7.9 mg/dL |
| RBC | 3.51 × 106 per mcL | Magnesium | 1.8 mg/dL |
| WBC | 5 × 103 per mcL | Uric acid | 7.1 mg/dL |
| Platelets | 226 × 103 per mcL | Cholesterol | 229 mg/dL |
| Urea | 107 mg/dL | Triglycerides | 472 mg/dL |
| Creatinine | 3.7 mg/dL | Albumin | 1.7 g/dL |
| Na | 140 mEq/L | CRP | 0.2 mg/L |
| K | 6.7 mmol/L | Glucose | 99 mg/dL |
| Cl | 111 mEq/L | Liver enzymes | Normal |
RBC: red blood cell; WBC: white blood cell; CRP: C-reactive protein
Anemia workup
| Labs | Values | Labs | Values |
|---|---|---|---|
| Iron | 103 mcg/dL | Vitamin B12 | 52 ng/L (low) |
| TIBC | 180 mcg/dL | Folic acid | 2.5 ng/mL |
| Transferrin iron saturation | 57% (high) | Haptoglobin | 2.02 g/L |
| Transferrin | 77 g/L | Fibrinogen | 471 mg/dL (high) |
| Ferritin | 129 ng/mL | LDH | 158 U/L |
TIBC: total iron binding capacity; LDH: lactate dehydrogenase
The autoimmune workup was normal: anti-streptolysin O normal; no hypocomplementemia, C3: 92 mg/dL normal; C4: 28 mg/dL normal, anti-nuclear antibody negative, anti-neutrophil cytoplasmic antibody negative; perinuclear anti-neutrophil cytoplasmic antibody negative; anti-double-stranded DNA immunoglobulin G (IgG) negative, polymyositis and scleroderma-100 (Pm/Scl-100) negative, centromere B normal and cryoglobulins normal. Anti-thyroid peroxidase antibody (anti-TPO Ab) negative.
Wright and Widal tests negative; Toxoplasma serology [IgG, immunoglobulin M (IgM)] negative; cytomegalovirus negative; total IgM, IgG, immunoglobulin A (IgA) normal. Tests for human immunodeficiency virus, hepatitis B virus, hepatitis C virus were negative. Parathormone (PTH) level was 152 pg/mL (high); thyroid stimulating hormone (TSH): 15.5 mlU/L; T3: 0.87 pmol/L, T4: 11.58 pmol/L; thyroglobulin: 14.24 ng/mL; hemoglobinA1c (HbA1c): 5%.
Urinalysis showed proteinuria without hematuria or leukocyturia. There were no lung abnormalities on chest x-ray.
An abdominal and pelvic ultrasound showed a right kidney measuring 14 cm and a left kidney of 13 cm with echogenic parenchyma and cortico-medullary dedifferentiation in favor of a chronic nephropathy without dilation nor lithiasis. His 24-h urine collection showed 18g of proteinuria and a glomerular filtration rate (GFR) of 22 mL/mn. Consequently, the patient was found to have nephrotic syndrome.
A kidney biopsy was done. It showed under light microscopy a major reduction in renal mass (> 80%), one crescent in one residual viable glomerulus, signs of acute interstitial nephritis with tubular necrosis and marked thickening of the vascular walls with fibro-proliferative endarteritis (Figures 1 and 2). Immunofluorescence studies revealed mesangial deposits, of same intensity, with IgM, C1q and C3. IgA and IgG were negative. The immunofluorescence data suggest the diagnosis of C1q glomerulopathy.
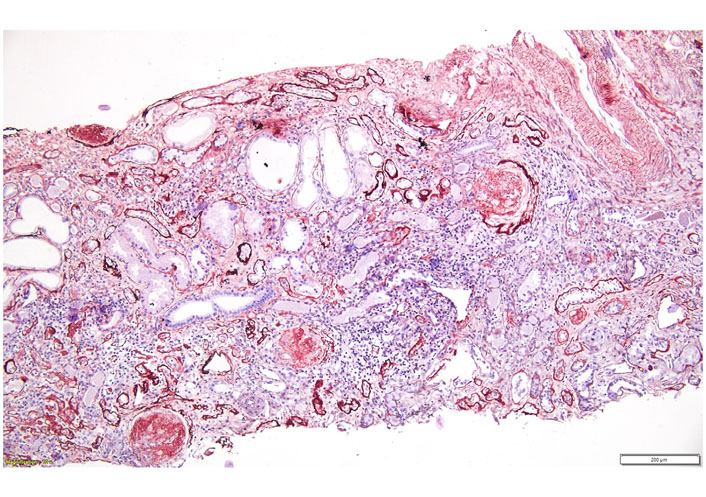
Light microscopy: foci of lymphocytic interstitial infiltrates associated with sclerotic glomeruli and hypertrophic tubules (periodic acid-Schiff staining)
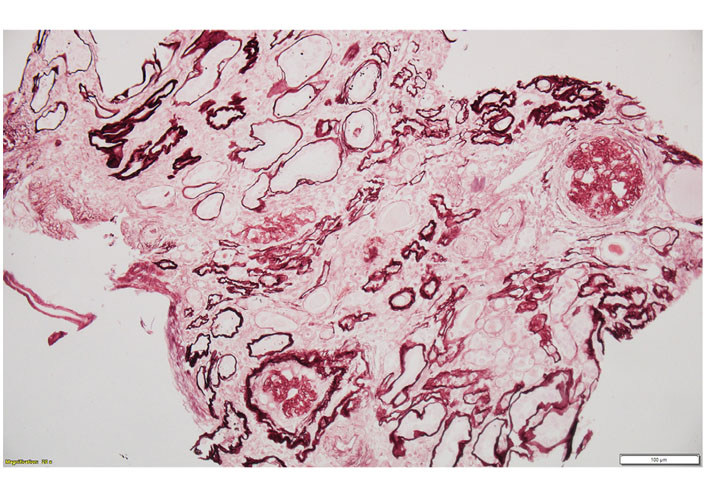
Light microscopy with periodic acid-silver methenamine staining: interstitial enlargement with tubular atrophy and sclerotic glomeruli
Based on these findings, the patient was hospitalized, and a high dose of intravenous steroids (methyl prednisolone) was given: 500 mg daily, for 3 consecutive days, followed by oral prednisone (1 mg/kg) and then slowly tapered till cessation. This treatment targeted the crescent lesion mainly, with the aim of slowing the progression of kidney failure and of delaying hemodialysis. No immunosuppressive treatment was added due to his advanced kidney fibrosis. Angiotensin-converting enzyme (ACE) inhibitors and statins were prescribed to decrease his level of proteinuria. The patient never had hypertension. No improvement in kidney function was noted nor in proteinuria or albuminemia and the patient was started on hemodialysis then got transplanted 8 months later. His creatinine went down to 1.5 mg/dL with disappearance of proteinuria and he is doing well.
Discussion
C1q nephropathy is a kidney disease in which a large amount of proteins are lost in the urine [6]. It is one of the many diseases that can cause the nephrotic syndrome [6]. C1q is a normal protein of the immune system. In C1q nephropathy, this protein can be found deposited throughout the kidneys [6]. Since these deposits can only be seen under a microscope, a kidney biopsy is required to diagnose C1q nephropathy [6]. C1q nephropathy is one of the most recently discovered kidney diseases, and it is not yet well described in the literature. It is thought that the deposited C1q activates the immune system within the kidney itself, and the resulting immune response and inflammation are what cause the kidney damage [6]. As a disease, it is very similar to two other diseases on this site, MCD and FSGS [6]. In C1q nephropathy, the kidney filters can look absolutely normal under light microscopy though they can also have visibly “scarred” areas as well, such in FSGS [6]. It is not until special “stains” specific for the C1q protein are added to the sample that the differences can be seen [6]. These stains cause the areas of the biopsy where C1q has deposited to glow bright green under certain types of light [6]. Also, if the biopsy is evaluated under an “electron microscope”, the C1q deposits themselves can be seen [6]. C1q nephropathy is more common in childhood, but can be detected in early adulthood [6]. Symptoms of C1q nephropathy are more likely to be related to nephrotic syndrome (edema, hypertension hypercholesterolemia, nephrotic range proteinuria, etc.) but the diagnosis needs kidney biopsy. Treatment of C1q nephropathy is not considered easy, and the patient should be monitored closely by a nephrologist [6]. It is the same as MCD or FSGS [6]. Proteinuria is treated in general with ACE inhibitors or angiotensin receptor blockers. The complications of the nephrotic syndrome must be taken into consideration. If the kidney function declines, other measures should be taken as steroids and immunosuppressive treatment, keeping in mind their large spectrum of side effects. If the patient is considered to have MCD, the immunosuppressive drugs that shall be taken into consideration, are cyclophosphamide, rituximab, calcineurin inhibitors (CNIs), or mycophenolic acid analogs [7]. Concerning FSGS, CNIs are the only drugs that are considered efficient nowadays as an alternative to steroids [7]. Because it is both a relatively new and rare disease, it is difficult to predict the progression of C1q nephropathy [6]. While some people have been known to go into complete remission, others have developed end stage renal disease requiring dialysis or a kidney transplant. C1q nephropathy can present with a steroid resistant kidney damage that may lead to an irreversible renal failure. Fortunately, complete renal failure so far seems to be the exception rather than the rule [5]. The kidney biopsy can sometimes help predict the progression of the disease as well [6].
In this case, a rapid deterioration (within a few months) of the renal function without receiving any treatment was noted. This makes the cause of C1q nephropathy more likely to be FSGS than MCD. If this is the case, this might affect kidney transplantation process due to the high likelihood of recurrence afterwards. The patient received a kidney transplant from a living donor (his mom) and did not develop complications afterwards. His creatinine is stable and is doing well after 6 months of transplantation.
In front of having risks of recurrence such as rapid initial deterioration and young age, the risk of recurrence is still high and should be followed more closely mainly the first year after receiving the kidney [8, 9]. This case was compared to three previously reported cases [4, 10, 11] (Table 3):
Comparison between this case report and previously reported cases
| Diagnostic tools and treatment | Case 1 (our patient) | Case 2 [4] | Case 3 [10] | Case 4 [11] |
|---|---|---|---|---|
| Age/Gender | 19-year-old man | 42-year-old man | 17-year-old man | 77-year-old woman |
| Clinical presentation | Recurrent nausea, decreased appetite, weight loss | High grade fever, chills, nausea, vomiting, decreased urine output, lower limbs edema, high blood pressure | Isolated selective proteinuria, in routine study, normal renal function | Facial and lower limbs edema, high blood pressure, oliguria |
| Lab tests | Elevated creatinineAutoimmune workup: negativeSerologies (HBV, HCV, etc.): negativeNormal C3 C4 | Elevated creatinineAutoimmune workup: negativeSerologies: negativeNormal C3 C4 | Normal creatinineAutoimmune workup: negativeSerologies: negativeNormal C3 C4 | Elevated creatinineAutoimmune workup: negativeSerologies: negativeNormal C3 |
| Urine test | ProteinuriaNo hematuria | ProteinuriaHematuria | ProteinuriaNo hematuria | ProteinuriaHematuria |
| Imaging (abdominal and kidney ultrasound) | Chronic nephropathy | Bilateral bulky kidneys with normal echotexture | Normal | Normal |
| Biopsy | Major reduction in renal mass, one crescent, acute interstitial nephritis with tubular necrosis, marked thickening of the vascular wallsIF: mesangial deposits of IgM, C1q and C3. IgA and IgG negative | Suggestive of focal proliferative GNIF: dominant mesangial deposition of C1q with C3 | Segmental glomerular sclerosis, moderate increase of mesangial matrixIF: + C1q (dominant), IgA, IgG, IgM, C3, with a granular mesangial distribution | 2% tubular atrophy with interstitial fibrosis and mononuclear interstitial infiltrateIF: + IgG, IgA, IgM, C3, C4, C1q (dominant)With strong mesangial and some peripheral capillary staining |
| Treatment | No response to pulse steroidsImmunosuppressive treatment not addedACE inhibitors were prescribedHemodialysis doneRemission after kidney transplant | Some sessions of hemodialysis for the acute renal failureComplete remission after pulse steroids and prednisolone per os | Complete remission after 18 months of treatment with enalapril and losartan | Complete remission after 3 months of treatment with steroids, 2 sessions of cyclophosphamide and some sessions of hemodialysis |
HBV: hepatitis B virus; HCV: hepatitis C virus; IF: immunofluorescence
C1q nephropathy can, consequently, occur at any age regardless of the gender of the patient.
The clinical presentation is variable from patient to another, thus, not all patients have kidney failure or decreased renal function upon presentation, as well as for high blood pressure or decreased urine output which were not necessarily found in all patients [4, 10, 11]. Proteinuria is an important finding, all reported patients had proteinuria but hematuria was not found in all patients. The kidney ultrasound was not very helpful, as it did not report major findings or abnormalities in most cases. The autoimmune workup was negative in all reported cases, which helped to rule out lupus nephritis.
The biopsy was the most important and helpful investigation to be done in all reported cases; it is the cornerstone to confirm the diagnosis, by identifying C1q deposits [4, 10, 11]. However, the treatment was very different between all cases, and each patient responded to a certain type of therapy. Some cases were very sensitive to steroids, whereas others were resistant, which necessitate immunosuppressive therapy or hemodialysis or kidney transplantation [4, 10, 11].
No previous study could highlight a direct relationship between the protein supplement taken months prior to the presentation and the patient’s de novo kidney disease. However, some studies showed that high protein diets may induce kidney injury or aggravate a chronic kidney disease [12].
Interestingly, cases of secondary C1q nephropathy due to viral infection or rheumatoid arthritis have also been reported, with patients exhibiting symptoms of the underlying conditions (not found in our case) [2].
In summary, this is the case of a 19-year-old patient, previously on protein supplements, not known to have hypertension or other health problems who presented with severe kidney injury due to C1q nephropathy that did not respond to steroids and lead to end stage kidney disease. Mainly, diagnosis relies on a kidney biopsy with light microscope, immunofixation and electron microscopy, after the exclusion of other etiologies mainly SLE. Further studies are warranted to establish a connection between protein supplements, and progression of kidney disease. A better comprehension of the pathophysiology mechanism is necessary in order to define the treatment and the prognosis of this disease.
Abbreviations
| ACE: | angiotensin-converting enzyme |
| FSGS: | focal segmental glomerulosclerosis |
| GN: | glomerulonephritis |
| IgA: | immunoglobulin A |
| IgG: | immunoglobulin G |
| IgM: | immunoglobulin M |
| MCD: | minimal change disease |
Declarations
Author contributions
VN, RC and JF wrote the first draft of the manuscript. JAN, SB and BBA helped with collection of data. CG was the pathologist who interpreted biopsy results. All authors contributed to revision of manuscript, read and approved the submitted version.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Written informed consent was obtained from the patient.
Consent to publication
Not applicable.
Availability of data and materials
All relevant data are contained within the manuscript.
Funding
Not applicable.
Copyright
© The Author(s) 2022.