Abstract
Aim:
This study investigates the collaborative efforts between speech language therapists and dentists to address the challenges faced by patients with concurrent dental and speech issues. It underscores the importance of understanding the complex interactions within the craniofacial system and its implications for both oral health and communication abilities.
Methods:
A questionnaire-based research was conducted involving speech language therapists and dentists, using Google Forms as the medium of data collection. This study was disseminated through professional networks, where practitioners provided information on their demographics, practices of collaboration, and the perceived advantages of such interdisciplinary work. All ethical standards were adhered to, ensuring the confidentiality and informed consent of the participants.
Results:
The findings indicate that dentists, often see first patient visits beyond recommended ages primarily for existing conditions, deviating from preventive norms. About half communicate monthly with speech language therapists, revealing gaps in early care and collaboration. Speech language therapists focus on language disorders and orofacial myofunctional disorders (SMOF), with 37% collaborating frequently with dentists. This interaction highlights the potential for enhanced patient outcomes through interdisciplinary cooperation. Despite these challenges, both groups acknowledged the benefits of their collaborative efforts.
Conclusions:
The partnership between speech language therapists and dentists represents a vital area of healthcare, aimed at tackling the complex issues of oral health and communication through a multidisciplinary approach. Although obstacles in collaboration were identified, the positive outcomes observed from such partnerships emphasize the importance of developing a unified framework to improve integrated healthcare delivery in the future.
Keywords
Interdisciplinary communication, pediatric dentistry, speech therapy, patient outcome assessment, collaborative healthcareIntroduction
The craniofacial complex, comprising bones, teeth, muscles, and nerves, demonstrates significant adaptability, influenced by both genetic and environmental factors [1, 2]. This system supports vital functions such as sensory perception, feeding, and communication. The head, especially the face, is a complex anatomo-functional system, intricately linked with sensory and motor functions, including olfaction, vision, hearing, taste, and proprioception [3, 4].
The collaborative synergy between speech-language pathologists (speech language therapists) and dentists assumes pivotal significance when addressing patients grappling with concomitant or dependent dental and linguistic, masticatory, or swallowing issues [3]. Operating within disparate yet inherently complementary domains, these specialized professionals can achieve outcomes that go beyond individual expertise through their collaborative efforts, providing a real multidisciplinary approach [5].
Dentists play a vital role in the diagnosis, prevention, and treatment of diseases affecting the oral cavity and its adjacent structures. Their expertise is not limited to maintaining oral health but extends to influencing the overall well-being of individuals. This includes managing congenital and acquired conditions that affect the teeth, mouth, jawbones, and associated joints and tissues [6]. Additionally, dentists, especially orthodontists, are instrumental in correcting dental and skeletal malalignments. They employ various devices to correct malocclusion, move teeth, and stimulate growth centers, which are essential for the harmonious development of the craniofacial region [7, 8].
Orthodontists focus specifically on the alignment of teeth and jaw structures, aiming to enhance skeletal relationships during the active growth phases of the craniofacial complex. Their interventions can significantly impact oral functions and prevent the development of occlusion pathologies and growth disorders [9].
Equally important in this interdisciplinary landscape is the role of pedodontists, who specialize in pediatric dentistry. They possess unique skills tailored to address the specific dental and communicative needs of children. Pedodontists play a critical role in the early stages of a child’s life, providing care that goes beyond conventional dental treatments. Their expertise enables them to detect and intervene early in potential developmental issues, thus ensuring holistic oral health and communication development from a young age [10, 11]. This collaborative model between speech-language pathologists, dentists, and pedodontists illustrates a comprehensive approach to healthcare that integrates the intricate interplay between oral health and human communication, ensuring that all aspects of craniofacial development are addressed effectively.
Conversely, speech-language pathologists specialize in the assessment, diagnosis, and treatment of communication disorders, language issues, and oral function abnormalities [12]. Operating across diverse age groups, their mission extends beyond conventional boundaries, aiming to enhance communication skills, facilitate verbal expression, and promote comprehension [13]. Notably, the speech-language pathologists’ role encompasses a broader intervention context, particularly in preventing oral function disorders and addressing oral movements throughout various life stages, spanning infancy, developmental phases, adulthood, and geriatric stages [14, 15].
The collaboration among speech language therapists and dentists is essential and indispensable in patients affected by orofacial myofunctional disorders (SMOF). SMOF is defined as any alteration of the oral, facial, and cervical musculature that interferes with growth, development, or the functioning of orofacial structures and functions [16].
The prevalence of SMOF in different life stages, according to the International Association of Orofacial Myology, ranges from 38% in the general population to 81% in children with language problems [17].
In cases where patients present with both dental problems and communication or oral function disorders, the collaboration between dentists and speech-language pathologists proves exceptionally advantageous [18].
The speech language therapist, in agreement with the dentist, will establish the timing and implementation of myofunctional treatments aimed at the education and reeducation of oral functions (resting position, swallowing, breathing, chewing, and articulation of phonemes). Whether mitigating a child’s pronunciation issues attributable to malocclusion or assisting an adult undergoing oral surgery that impacts speech, this collaborative alliance optimizes outcomes [19].
This collaborative synergy extends beyond the individual expertise of dentists and speech language therapists, fostering an integrative approach that comprehensively addresses the intricate interplay between oral health and communication.
This interdisciplinary approach emerges as indispensable in addressing the multifaceted challenges associated with oral health and human communication [20]. In this collaborative paradigm, the role of the speech-language pathologists extends beyond conventional expectations. Their involvement spans from addressing speech and language disorders to actively participating in the assessment and rehabilitation of oral functions, recognizing the intricate interdependencies between these domains. Similarly, dentists acknowledge the integral role of communication in overall well-being, understanding that successful treatment outcomes involve not only the restoration of dental health but also the optimization of oral functions that contribute to effective communication. This perspective is not only rooted in theoretical considerations but also finds robust support in existing literature, which underscores the necessity of precise guidelines delineating the parameters of interdisciplinary collaboration between speech therapists and dentists [10–20].
The primary focus of this cohort observational study is to understand the interactions between speech-language pathologists and dentists. Given the identified challenges and the existence of discernible knowledge gaps, we have opted for a comprehensive questionnaire-based study to meticulously evaluate the collaborative dynamics between these two professional groups. This investigation aims not only to contribute to the existing body of knowledge but also to provide practical insights that can inform and enhance interdisciplinary practices in the realms of oral health and communication.
Materials and methods
To systematically extract insights from professionals, our research employed two meticulously designed questionnaires tailored for speech-language pathologists and dentists, respectively. The speech language therapists’ questionnaire focused on investigating the demographics of their patient population, years of professional experience, collaborative practices ranging from ‘daily’ to ‘never’ with other specialists, and the interactions with dentists, including the nature, timing, and modalities involved. Similarly, the dentists’ questionnaire investigated workplace specifics, years of practice, patient demographics, collaboration experiences with speech language therapists, the nature of cases encountered, frequency of information exchange, and the perceived significance of this interdisciplinary interaction.
The questionnaires, hosted on Google Forms, aimed to streamline the response process for participants, ensuring convenience and accessibility. The survey window spanned from January 10, 2023, to January 22, 2023, during which practitioners in speech-language pathology and dentistry were invited to contribute. Widely disseminated through professional networks, messaging platforms like WhatsApp and Telegram, social media channels, and emails, the questionnaires remained open for approximately two weeks, allowing for possible modifications.
Participants meeting the inclusion criteria, actively practicing professionals in speech-language pathology and dentistry, were recruited with a deliberate focus on achieving diversity in geographical locations and professional experience.
Post-survey closure, the responses underwent a meticulous collection and analysis process. The data, compiled and entered into a Microsoft Excel sheet, underwent scrutiny using SPSS version 19 and descriptive statistical methods. Demographic and categorical data were summarized through descriptive statistics, enabling a comprehensive overview of the survey outcomes. The findings from both professional groups were systematically compared, revealing patterns, disparities, and common themes in their collaborative practices.
In adherence to the meticulous guidelines established for online survey studies, this research has prioritized and implemented robust measures to safeguard data privacy and uphold ethical standards. The study adhered strictly to ethical guidelines in line with the Helsinki declaration and was approved by the ethical committee with approval n.95-23 (14/12/2022, A.O.U. “G. Martino”) ensuring participant confidentiality and anonymity, no personal data, as name and surname, email or any ranging from ‘daily’ to ‘never’ detail that could reveal personal information were gathered.
The participants performed the login in the Google Form using their credentials that were not shared by Google to the authors, in line with the company’s privacy guidelines.
Informed consent was obtained from every participant prior to their engagement in the survey, reinforcing the commitment to ethical research practices and the responsible handling of valuable professional insights.
Results
Analysis of the data
The total number of participants in the survey was 152, comprising 82 dentists and 70 speech language therapists. Angela Alibrandi directly invited 245 participants, obtaining 152 questionnaires, therefore the response rate is calculated at 62%. The data obtained from the questionnaire analysis reveal the following key findings.
Survey of dentists
The majority of respondents practice in the Sicily region (78 participants)
Forty percent of the dentists have between 21 and 30 years of professional experience, with a relatively even distribution between those practicing for less than 5 years (21%) and those with between 11 and 20 years of experience (23%), a smaller distribution (16%) for dentists is practicing between 5 and 10 years. Eighty-four percent provide services in the pediatric and/or orthodontic field, while only 13% focus on ranging from ‘daily’ to ‘never’ areas (Figure 1A).
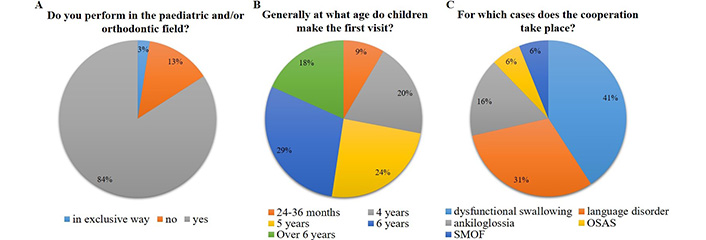
Survey of dentists. (A) Field of expertise. (B) Age of first visit. (C) Collaboration topic. OSAS: obstructive sleep apnea syndrome; SMOF: orofacial myofunctional disorders
Responses regarding the age of the first dental visit show variability, with the majority (29%) indicating 6 years, 24% 5 years, 20% 4 years, and a notable 18% beyond 6 years (Figure 1B).
Regarding the reasons for the first visit, over 70% link it to existing issues, while only 29.3% consider it for preventive purposes. This raises questions about the role of preventive dentistry in pediatric care.
A significant finding is that only 24 dentists are regularly in contact with speech language therapists, with four of them having this professional within their practice.
Collaborations primarily focus on issues such as dysfunctional swallowing (41%), language disorders (31%), ankyloglossia (16%), and, to a lesser extent, obstructive sleep apnea syndrome (OSAS) and orofacial myofunctional disorders (SMOF) (6% each) (Figure 1C).
The majority (46%) report sharing progress information about once a month, while about 30% share information at the beginning and end of treatment, and 24% share information from 1 to 4 times during the whole therapy.
Survey of speech-language pathologists
Responses were collected from speech language therapists practicing in 12 different regions, with a prevalence from Sicilian professionals, mostly in private practice (54.3%).
The majority of the sample has 5 to 10 years of experience (34%), followed by those practicing for less than 5 years (31%), more than 10 years (13%), over 30 years (13%), and less than 5 years (9%).
Sixty percent fall within the developmental age group, while 24% are adults. Five percent of the speech-language pathologists have no age selectivity (Figure 2A).
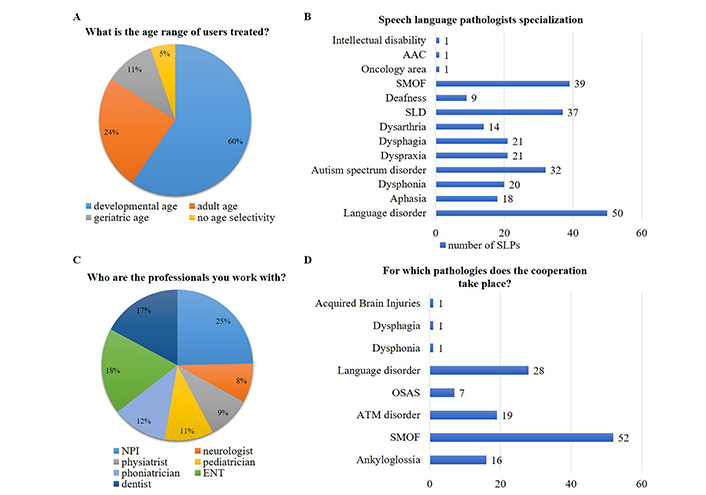
Survey of speech-language pathologists. (A) Patient age distribution. (B) Speech-language pathologists specializations. SMOF: orofacial myofunctional disorders; SLPs: speech-language pathologists. (C) Multidisciplinary team analysis. NPI: neuropsychiatrists; ENT: otolaryngologists. (D) Pathologies treated in cooperation. OSAS: obstructive sleep apnea syndrome; ATM disorders: temporo mandibular articulation disorders
Speech language therapist specializations of particular interest for collaboration include language disorders (50 specialists) and SMOF (39 specialists) (Figure 2B).
Around 31% report interaction at the beginning and end of treatment, 35% approximately once a month, and 15.4% limit interaction to patient referrals.
The majority work in multidisciplinary teams, particularly with child neuropsychiatrists (NPI, 25%), otolaryngologists (ENT, 18%), and dentists (17%) (Figure 2C).
Only 37% of surveyed speech language therapists are regularly in contact with a dentist.
Collaborations mainly involve issues such as SMOF, language disorders, temporo mandibular articulation (ATM) disorders, ankyloglossia, and OSAS, with occasional involvement in dysphonias and feeding/swallowing disorders (Figure 2D).
One hundred percent speech language therapists believe that collaboration with a dentist is beneficial for the patient.
Discussion
The collaboration between speech language therapists and dentists is crucial for addressing the complex interactions of oral health and communication. The stomatognathic system, comprising bones, muscles, joints, nerves, and glands, undergoes dynamic changes and requires a deep understanding of its functions [21, 22]. This partnership leverages dentists’ expertise in oral health and speech language therapists’ skills in managing communication disorders, oral functions, and swallowing issues across all ages.
Alexandre G. Petrovic’s concept of a servo-system highlights the need for neuromuscular homeostasis in facial development, emphasizing the interdependence of hormonal, muscular, and dental factors [23]. In clinical settings, this collaboration is essential, especially for patients facing simultaneous dental and linguistic challenges. It plays a significant role in various scenarios, from pediatric to geriatric cases, ensuring comprehensive care that addresses both speech and dental health, and optimizing patient outcomes [24, 25].
Collaboration landscape: dentists
The emphasis on pedodontic and orthodontic services aligns with the preventive approach, but the ambiguity regarding the age of the first dental visit raises concerns and reveals a lack of shared guidelines among these categories. The majority associating the first visit with existing issues rather than prevention underscores a potential gap in early preventive dental care, conflicting with established guidelines (Figures 1A, B) [26].
For dentists in contact with speech language therapists, collaboration primarily revolves around dysfunctional swallowing, language disorders, and ankyloglossia (Figure 1C). The frequency of information sharing varies, with around 45.8% reporting monthly interactions. This consistent exchange is positive, yet the 16.7% opting for minimal involvement through sending patients raises questions about the depth of collaboration.
Encouragingly, the entire sample perceives collaboration with speech language therapists is beneficial for patients. This unanimity emphasizes the potential for synergy between oral health and communication professionals.
Collaboration landscape: speech language therapists
Examining the data in light of existing literature reveals intriguing patterns, suggesting regional variations and urging a reevaluation of established norms. Challenges include variations in the frequency and modes of information exchange, emphasizing the need for enhanced interdisciplinary communication channels (Figures 2A, B).
Speech language therapists’ responses reveal a majority engaging in collaborative practices, treating pediatric cases for speech and language disorders as well as orofacial dysfunctions. The frequency of information exchange highlights the need for more standardized communication protocols (Figures 2C, D).
Despite challenges, the overwhelming consensus on the mutual benefit of collaboration underscores its potential to enhance patient care.
The collaboration between these two professional groups appears to be important for the resolution of many pathologies of the whole oro-maxillofacial complex, and this data appears evident when evaluating the field of expertise and the outcome of the respective therapies [26]. The literature shows how the correction of some of the more common dental mispositions for example, open bite appears to be directly related to a pathologic tongue position that besides the orthodontic device that dentists usually use should be rehabilitated with a multidisciplinary and myofunctional approach by speech language therapists with specific tongue exercise [27, 28]. Even considering the early orthodontic management and myofunctional treatment in deciduous and mixed dentition children appears to be a promising approach, the quality of the existing evidence is questionable [26, 27]. This kind of evidence should be considered with the scarcity of papers that evaluate this kind of multidisciplinary approach and the possible collaboration between these two specialists [29–31]. The lack of scientific papers evaluating the important relationship between therapies and outcomes with such multidisciplinary approach should be further analyzed and studied including besides this epidemiological evaluation of clinical studies with long-term follow-up [32, 33].
The strengths of this research lie in the comprehensive multidisciplinary approach, the questionnaire-based methodology, the clinical scenario illustration, and the integration with existing literature. However, limitations include regional bias, a relatively small sample size, potential questionnaire design impact, reliance on self-reported data, and a limited exploration of collaboration variances.
It is important to stress that this kind of observational study is important to evaluate the habits of these two professional groups and further develop some shared guidelines based on a precise understanding of the strong and weak points of this collaboration, moreover, evaluating and delimitating a shared field of work.
Future research could further evaluate this kind of collaboration nationally and internationally. Moreover, the clinical result of this kind of multidisciplinary approach should be evaluated by considering specific applications [34, 35].
While the study reveals encouraging collaborative trends, it also highlights areas for refinement, emphasizing the need for a more nuanced understanding of factors influencing successful interdisciplinary partnerships. Future research could delve deeper into specific challenges and facilitators, fostering more effective collaborative models.
The professional collaboration between speech-language pathologists and dentists appears to be a vibrant and progressive frontier within the realm of healthcare, propelling the evolution of an integrated approach to address the intricate intersection of oral health, communication, and myofunctional equilibrium. This collaboration not only acknowledges the complexity of these interconnected aspects but also aims to provide patients with a comprehensive healthcare strategy that optimizes outcomes.
As this collaboration matures, the potential for transformative impacts on patient outcomes becomes increasingly evident. The promise of a future where the synergy between speech-language pathologists and dentists stands as a cornerstone in effective healthcare delivery holds great significance. This partnership extends beyond traditional boundaries, fostering an environment where the exchange of knowledge and expertise is seamless, contributing to a holistic patient care experience.
This paper is aimed to perform a detailed analysis of the therapeutic approaches currently employed. It aspires to be a valuable tool, offering practical insights to enhance collaboration and ensuring that both professions work in tandem to achieve the common goal of providing the best possible treatment for the patient.
Recognizing the significance of collaboration between specialists, this paper underscores the importance of respecting and leveraging their respective expertise. It emphasizes viewing pathological conditions as manifestations of “imbalance” within a unified and integrated system. The data retrieved are aimed to advocate a holistic, synthetic, and coordinated strategy, asserting that the evaluation of any condition cannot be comprehensive without considering the interconnected aspects of oral health and communication. In embracing this unified perspective, healthcare practitioners can offer a level of care that transcends conventional boundaries, fostering an environment where patients receive truly comprehensive and patient-centered treatment.
Abbreviations
| SMOF: | orofacial myofunctional disorders |
Declarations
Author contributions
MC: Investigation, Data curation. FP and AA: Writing—review & editing. RLG: Methodology, Writing—original draft. IC: Conceptualization, Investigation. All authors have read and agreed to the published version of the manuscript.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical approval
The study was conducted following the Declaration of Helsinki and was approved by the Ethical Committee with approval n.95-23 (14/12/2022, A.O.U. “G. Martino”).
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Consent to publication
Not applicable.
Availability of data and materials
Raw data can be requested from the corresponding author.
Funding
Not applicable.
Copyright
© The Author(s) 2024.