Affiliation:
1Multidisciplinary Department of Medical-Surgical and Odontostomatological Specialties, University of Campania “Luigi Vanvitelli”, 80121 Naples, Italy
2FiDent - Centro Medico Odontoiatrico, 89121 Reggio Calabria, Italy
ORCID: https://orcid.org/0000-0002-9478-4138
Affiliation:
1Multidisciplinary Department of Medical-Surgical and Odontostomatological Specialties, University of Campania “Luigi Vanvitelli”, 80121 Naples, Italy
3Department of Dental Cell Research, Dr. D.Y. Patil Dental College and Hospital, Dr. D.Y. Patil Vidyapeeth, Pune 411018, Maharashtra, India
4Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, 98125 Messina, Italy
5School of Dentistry, Aldent University, 1001 Tirana, Albania
Email: lucafiorillo@live.it
ORCID: https://orcid.org/0000-0003-0335-4165
Affiliation:
6Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University, Chennai 600077, Tamil Nadu, India
7Department of Woman, Child and General and Specialist Surgery, University of Campania “Luigi Vanvitelli”, 80121 Naples, Italy
ORCID: https://orcid.org/0000-0002-9494-6942
Affiliation:
4Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, 98125 Messina, Italy
5School of Dentistry, Aldent University, 1001 Tirana, Albania
ORCID: https://orcid.org/0000-0002-1378-2588
Affiliation:
2FiDent - Centro Medico Odontoiatrico, 89121 Reggio Calabria, Italy
ORCID: https://orcid.org/0009-0004-5156-8744
Affiliation:
8Department of General Surgery and Medical-Surgical Specialties, School of Dentistry, University of Catania, 95124 Catania, Italy
ORCID: https://orcid.org/0000-0003-2311-9728
Affiliation:
2FiDent - Centro Medico Odontoiatrico, 89121 Reggio Calabria, Italy
ORCID: https://orcid.org/0000-0003-4619-4691
Explor Med. 2024;5:477–491 DOl: https://doi.org/10.37349/emed.2024.00233
Received: May 13, 2024 Accepted: June 24, 2024 Published: July 05, 2024
Academic Editor: Luca Testarelli, Sapienza University of Rome, Italy
The article belongs to the special issue Oral Health Interconnections and Multidisciplinary Approaches
Background: This systematic review aims to critically assess the literature on the debonding process of orthodontic brackets from enamel surfaces. The review evaluates Randomized Controlled Trials (RCTs) to determine the effectiveness and implications of various debonding techniques and materials.
Methods: The study followed PRISMA guidelines, selecting RCTs published from 1999 onwards that compared the outcomes of various orthodontic bracket debonding techniques. Selection criteria included studies utilizing human teeth, with outcomes such as enamel surface roughness and Adhesive Remnant Index (ARI) analyzed. Data sources included PubMed, Scopus, Web of Science, and the Cochrane Library.
Results: Out of 1,587 records identified, five studies met the inclusion criteria. These studies provided comparative data on the effectiveness of various debonding techniques, including tungsten carbide and diamond burs, in minimizing enamel damage and optimizing adhesive removal. Findings indicated that tungsten carbide burs produced the least enamel roughness.
Discussion: Utilizing tungsten carbide burs for debonding orthodontic brackets significantly minimizes enamel surface roughness and potential damage, thereby enhancing the preservation of enamel integrity post-treatment. The systematic review highlights current debonding techniques are effective in adhesive removal, and the choice of instrument significantly affects enamel integrity and clinical outcomes. The findings support the need for continuous improvement and innovation in removing braces to improve orthodontic treatment results and patient satisfaction.
Orthodontic treatment aims to correct malocclusions and improve dental aesthetics and function by strategically applying orthodontic appliances, primarily brackets, to the teeth. The success of these interventions hinges significantly on the effectiveness of the bonding process, which secures the brackets to the enamel surface. The materials and techniques employed in this bonding process are crucial for the stability and efficacy of the treatment over time [1, 2].
The advent of adhesive technologies has markedly enhanced orthodontic treatment modalities. Initially, brackets were cemented onto bands that encircled the teeth, but modern practices predominantly utilize direct bonding methods that affix brackets directly to the tooth enamel using various adhesives. This direct bonding approach utilizes resin-modified glass ionomer cement or composite resins, offering distinct advantages in ease of use, cure time, and aesthetic compatibility with natural tooth coloration. These adhesives provide sufficient bond strength to withstand masticatory forces while allowing eventual removal after treatment without damaging the underlying enamel [3].
Despite these advancements, the debonding process—removing orthodontic brackets at treatment completion—poses significant challenges. Ideally, debonding should be quick, painless, and without adverse effects on enamel integrity. However, the reality often falls short of this ideal. Residual adhesive left on the teeth and potential enamel damage are common complications. The force required to dislodge orthodontic brackets can sometimes lead to enamel cracks or fractures, an undesirable outcome that compromises tooth structure and longevity [4].
The difficulty of debonding is influenced by several factors, including the type of adhesive used, the duration for which the brackets have been in place, and the specific debonding technique employed. Clinicians must choose mechanical and chemical debonding techniques with specific tools and protocols. Mechanical methods may involve pliers or specialized debonding devices that apply controlled force to the bracket. In contrast, chemical methods may soften the adhesive by applying heat or solvents to ease removal [5].
Epidemiological data underscore a high prevalence of malocclusions, with significant variability in the need for orthodontic treatment depending on the population studied. Crossbite was the most common occlusal anomaly requiring treatment, followed by openbite, overbite, and overjet. The overall need for orthodontic treatment was found to be substantial, emphasizing the importance of public health programs aimed at early orthodontic intervention to prevent the exacerbation of these conditions as children grow older. Dentin hypersensitivity (DH), often associated with non-carious cervical lesions, is a prevalent condition that affects a significant portion of the adult population. The hydrodynamic theory explains the pain mechanism in DH, which is triggered by fluid movement within dentinal tubules. Various treatment protocols, including diode lasers at different power outputs, have been investigated to manage this condition. When applied individually or in combination, these lasers have significantly reduced pain associated with DH. The findings suggest that a combined approach using low and high-power laser treatments may reduce DH symptoms most effectively. The studies underscore the necessity for early orthodontic interventions in children to prevent long-term dental issues and innovative treatments for managing DH in adults to enhance patient comfort and oral health. Recent studies have emphasized the need for innovations in debonding techniques that minimize damage to the enamel and reduce the discomfort associated with bracket removal. Innovations such as laser applications and vibrational tools are being explored for their potential to facilitate a smoother and less invasive debonding process [1–5].
In summary, while the bonding of orthodontic brackets has been refined over the years to ensure effective and reliable treatment outcomes, the debonding process remains a complex challenge that requires further innovation and research. Ensuring the integrity of enamel while efficiently removing orthodontic appliances is paramount to the long-term success and acceptance of orthodontic treatments.
This systematic review aims to evaluate the current literature on Randomized Controlled Trials (RCTs) and extrapolate the main results about the issues due to debonding after orthodontic treatments. Through this analysis, the review aims to identify best practices that optimize treatment efficacy and minimize potential harm to dental tissues, thereby guiding future orthodontic procedures and innovations in debonding technology.
In selecting studies for inclusion in this systematic review, we adhered strictly to defined eligibility criteria based on the PRISMA guidelines. The review focused on RCTs that evaluated the outcomes of various orthodontic bracket debonding techniques and their effects on enamel surface integrity and adhesive removal efficiency. Specifically, studies were included if they met the following criteria:
Study Design: Only RCTs published in peer-reviewed journals were considered. The studies needed to clearly describe the debonding method, including the type of brackets and adhesive systems involved and the tools and techniques employed for adhesive removal and enamel assessment.
Participants: Studies must have used human teeth; studies involving animal teeth or synthetic models were excluded. The teeth were required to have no pre-existing enamel defects or restorations to ensure that outcomes were attributable solely to the experimental procedures.
Interventions: The interventions included the use of various orthodontic bracket debonding instruments and techniques, such as different types of adhesive removal burs (tungsten carbide, sof-lex discs, diamond burs), debonding pliers, and new debonding instruments specifically designed for ceramic brackets. Comparisons between traditional methods and innovations were required.
Outcomes: Primary outcomes included measuring enamel surface roughness post-debonding and taking the time for complete adhesive removal. Secondary outcomes involved assessing the Adhesive Remnant Index (ARI) and any enamel damage through visual or microscopic methods [e.g., scanning electron microscopy (SEM)].
Publication Time Frame: Studies published from 1999 onwards were included to ensure that the techniques evaluated were relevant to current orthodontic practices.
Studies were excluded if they did not meet the above criteria, were non-randomized studies, reviews, or case reports, or involved compromised enamel integrity before the interventions. Additionally, studies not available in English or those lacking full-text access were excluded to ensure thorough assessment and data extraction. This stringent selection process was designed to ensure that the results synthesized from the included studies would be reliable and applicable to contemporary orthodontic practices.
A comprehensive search was conducted for the systematic review to identify all relevant studies published on orthodontic bracket debonding and its impact on enamel integrity. The search strategy was designed to include a broad range of electronic databases to ensure extensive coverage of the literature. The databases searched included PubMed, Scopus, Web of Science, and the Cochrane Library. These databases were chosen for their extensive indexing of biomedical and health-related journals, providing access to a wide array of RCTs in orthodontics.
In addition to the electronic databases, manual searches were performed on the reference lists of included studies and relevant review articles to identify additional studies that may not have been captured in the electronic search. This method, known as “snowballing,” ensures the inclusion of all pertinent literature, enhancing the comprehensiveness of the search.
The protocol for this systematic review and meta-analysis on the impact of orthodontic bracket debonding techniques on enamel integrity and adhesive remnants will be registered with PROSPERO. This registration will detail the objectives, eligibility criteria, outcome measures, and planned statistical analyses. PROSPERO ID is 546328, registered on 23/05/2024 [6].
Search terms used were carefully chosen to capture all relevant studies and included combinations of the following: “orthodontic brackets,” “bracket debonding,” “enamel surface,” “adhesive removal,” “debonding tools,” and “debonding techniques.” These keywords were used in various combinations and were adjusted for each database to match their specific indexing terms and search algorithms.
The search was limited to studies published in English from January 1999 to the present, aligning with the inclusion criteria regarding the publication timeframe. This time frame was selected to focus on recent advancements in materials and methods relevant to current clinical practices in orthodontics.
All identified records were managed using citation management software, which facilitated removing duplicates, screening abstracts, and organizing full-text articles for detailed evaluation. The search and selection process was detailed to ensure reproducibility and adherence to the PRISMA guidelines. This rigorous approach to identifying information sources aimed to lay a strong foundation for a comprehensive and unbiased review of the available evidence on the topic.
The selection process for the systematic review was meticulously conducted according to the PRISMA guidelines to ensure a transparent and reproducible methodology. Initially, all records identified through database searching and other sources were compiled, and duplicates were systematically removed using reference management software. Following this, the titles and abstracts of the remaining studies were screened independently by two reviewers to determine their potential relevance based on the predefined eligibility criteria. Studies that did not meet the inclusion criteria were excluded at this stage.
Full-text articles were retrieved for a more detailed assessment of potentially eligible studies or for which the relevance needed to be clarified based on the title and abstract alone. The same two reviewers independently examined the full-text articles to confirm whether each study met all the inclusion criteria. Discrepancies between reviewers regarding the eligibility of specific studies were resolved through discussion or, if necessary, by consulting a third senior reviewer.
No automation tools were used in the screening or selection phases to enhance the robustness of the selection process and minimize the risk of bias. The entire process was documented in detail, from the initial record identification to the final inclusion of studies. This documentation included reasons for excluding studies at the full-text stage, ensuring transparency, and providing a clear audit trail from the identified records to the studies included in the review. This meticulous approach was fundamental to maintaining the integrity and scientific rigor of the review process.
The data collection process for the systematic review was carried out with meticulous attention to detail to ensure the accuracy and completeness of the extracted information, adhering to the PRISMA guidelines. Two reviewers independently extracted data from each included study using a standardized data extraction form designed explicitly for this review. The form was pre-tested on a small subset of included studies to refine the data extraction fields and ensure comprehensive capture of all relevant data. Critical data collected included study characteristics such as study design, sample size, participant demographics, details of the interventions and controls, outcomes measured, and results. Information on the methodology, including debonding techniques, enamel assessment tools, and statistical analysis methods, was also extracted.
An extensive range of data items were collected for the systematic review to address the review’s objectives comprehensively. The primary outcomes focused on enamel surface roughness post-debonding, the time required for complete adhesive removal, and the ARI scores. Secondary outcomes included enamel damage assessments through various imaging techniques such as SEM and the presence of enamel cracks or fractures post-debonding. Additionally, data were gathered on the orthodontic brackets used, the adhesive systems, and the specific debonding techniques employed. The intervention characteristics, including the duration of bracket placement and the types of instruments used for adhesive removal, were also essential data items.
Other variables collected included study settings, country of origin, study design (e.g., randomization method, allocation concealment), baseline characteristics of the teeth used (e.g., age, health status), and any methodological details pertinent to understanding the study’s execution and context. Assumptions about missing or unclear information were noted, and justifications for decisions made during data synthesis were documented to maintain transparency.
The risk of bias in the included studies was rigorously assessed using standardized tools appropriate for evaluating the quality of RCTs. Two reviewers independently evaluated each study using the Cochrane Collaboration’s tool for assessing the risk of bias. This assessment included domains such as random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases [7].
For each domain, studies were categorized as having ‘low risk,’ ‘high risk,’ or ‘unclear risk’ of bias. The ‘unclear risk’ rating was used when the information provided was insufficient to make a clear judgment. Reviewer disagreements were resolved through discussion or consultation with a third reviewer to reach a consensus. This structured approach to the risk of bias assessment aimed to ensure that the conclusions drawn from the systematic review were based on high integrity and reliability data, minimizing the influence of bias on the review’s outcomes. This careful evaluation also facilitated the identification of potential limitations within the included studies, contributing to the overall quality assessment of the evidence [8, 9].
For each primary and secondary outcome identified in this systematic review, specific effect measures were defined and used to synthesize the data from the included studies. The effect measures included mean differences for continuous outcomes such as enamel surface roughness and time required for adhesive removal. Risk ratios were utilized for categorical outcomes, such as the ARI scores and incidences of enamel cracks. These measures were chosen to facilitate a clear and consistent comparison across studies, allowing for a quantitative synthesis of the results where possible. All effect estimates were reported with corresponding confidence intervals to assess the estimates’ precision and convey the statistical significance of the findings.
The data synthesis involved both qualitative and quantitative approaches, depending on the nature and heterogeneity of the data extracted. A narrative synthesis was conducted for all studies, summarizing the context, intervention details, and findings related to the debonding processes and their effects on enamel integrity. For sufficiently homogeneous outcomes regarding study design and reporting, a meta-analysis was performed using a random-effects model to account for any potential between-study variability. Statistical heterogeneity was quantitatively assessed. These synthesis methods were selected to provide a robust aggregation of the findings, offering insights into commonalities and variations across the included studies [10].
Several methods were employed to assess reporting bias within the studies included in the review. First analysis was generated for each result to visually inspect for asymmetry, which could indicate potential publication or selective reporting biases. Additionally, Egger’s regression test was applied to statistically detect the presence of such bias. Efforts were made to contact study authors for additional information where outcomes of interest were reported selectively or not reported at all. This comprehensive approach aimed to minimize the impact of reporting biases on the review’s conclusions and to ensure a fair representation of available evidence.
The studies were searched and selected systematically, identifying 1,587 records through database searching. After removing duplicates, 1,209 records were screened by title and abstract, excluding 1,140 records primarily due to irrelevance to the predefined criteria. The full texts of the remaining 69 articles were examined in detail, from which five studies met all the inclusion criteria and were included in the systematic review (Figure 1) for the PRISMA flow chart. The excluded studies commonly needed to meet inclusion criteria related to the study design, specifics of the debonding techniques used, or the outcomes measured.
The systematic review included five RCTs that evaluated various aspects of orthodontic bracket debonding techniques across different settings and populations.
Ghaleb et al. [11] conducted their study in China using 60 extracted human premolars to compare the effects of tungsten carbide, sof-lex discs, and diamond burs on enamel surface integrity after orthodontic bracket debonding. The primary outcomes assessed were enamel surface roughness and the time required for adhesive removal. Their findings indicated that the tungsten carbide burs produced the lowest enamel roughness while the diamond system produced the highest. Bishara et al. [12] performed their study in the USA with 30 extracted maxillary premolars. They tested a new ceramic bracket debonding instrument against conventional pliers, focusing on bracket failure characteristics and the incidence of enamel damage. Their results showed that the new debonding instrument significantly reduced the incidence of bracket fracture without increasing enamel damage compared to conventional pliers. Shamsi et al. [13] in Northern Ireland utilized 60 extracted premolars to compare the shear bond strength and residual adhesive after debonding between resin-modified glass ionomer cement (RMGIC) and resin applied as a precoated bracket. The study concluded that while RMGIC provided clinically effective adhesion, resin-precoated brackets offered higher shear bond strength. Shammaa et al. [14], based in the USA, examined 80 extracted premolars to compare the debonding force required for orthodontic brackets bonded with two conventional resin adhesives versus a resin-reinforced glass ionomer cement. Their study found no significant differences in bracket survival rates among the materials tested but noted that GIC required a lower debonding force. Osorio et al. [15] conducted their research in Spain, analyzing 60 recently extracted human premolars to assess the impact of 15-second versus 60-second etching times on the bond strength of orthodontic brackets and the amount of adhesive remaining on enamel post-debonding. Their findings highlighted that longer etching times improved bond strength and the quantity of adhesive remaining, suggesting better mechanical bonding. These studies collectively provide a broad perspective on the methodologies and outcomes related to orthodontic bracket debonding, emphasizing the nuances of different techniques and materials in achieving optimal clinical results.
This table offers a comprehensive overview of potential biases that might affect the internal validity of the RCTs reviewed. Each “Risk” designation should ideally be supported by specific comments derived from the study reports, providing justifications for each judgment (Table 1).
Risk of bias analysis
| First author et al. and year | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
|---|---|---|---|---|---|---|---|
| Ghaleb et al., 2024 | Low risk | Unclear | High risk | Low risk | Low risk | Low risk | Low risk |
| Bishara et al., 2008 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Shamsi et al., 2006 | Low risk | Unclear | High risk | Unclear | Low risk | Low risk | Low risk |
| Shammaa et al., 1999 (October) | Low risk | Low risk | Not applicable | Low risk | Low risk | Low risk | Low risk |
| Osorio et al., 1999 (February) | Low risk | Low risk | Not applicable | Low risk | Low risk | Low risk | Low risk |
Random sequence generation (selection bias): This assesses whether the allocation of treatments was randomized in a way that would not allow the predictor of allocation to be accounted for. Allocation concealment (selection bias) evaluates whether intervention allocations could have been foreseen before or during enrollment. Blinding of participants and personnel (performance bias): Considers if participants and those administering the interventions were blinded to group assignment. Blinding of outcome assessment (detection bias): Review whether the outcome assessors were blinded to the intervention provided. Incomplete outcome data (attrition bias): Looks at the completeness of outcome data for each primary outcome, including attrition and exclusions from the analysis. Selective reporting (reporting bias): Assesses if the reported findings include all of the study’s pre-specified outcomes. Other bias: Examines any potential source of bias not covered in the different domains
The results of individual studies are summarized in Table 2.
This table presents a synthesized view of each manuscript, focusing on the study type, sample size, main findings, and statistical significance of the results, which should assist in quickly understanding the outcomes and impacts of these studies
| First author et al. and year | Type of study | Sample size | Main results | Significant statistical results |
|---|---|---|---|---|
| Ghaleb et al., 2024 | Experimental in vitro | 60 teeth | Different systems for removing orthodontic adhesive affected enamel roughness differently. Tungsten carbide burs were best, followed by sof-lex discs, with diamond burs being the worst. | Yes, significant differences were found in enamel roughness and time for cement removal between different systems (p < 0.05). |
| Bishara et al., 2008 | Experimental in vitro | 30 teeth | New debonding instrument reduced bracket fracture compared to conventional pliers. | Yes, significant difference in bond failure patterns between two debonding methods (p = 0.013). |
| Shamsi et al., 2006 | Experimental in vitro | 60 teeth | Comparison of two adhesives showed differences in bond strength and residual adhesive. Resin-modified glass ionomer cement had lower bond strength than resin adhesive. | Yes, significant difference in bond strength and adhesive remnant index between two types of adhesives (p < 0.001). |
| Shammaa et al., 1999 (October) | Experimental (in vitro and in vivo) | 80 teeth (in vitro), 30 patients (in vivo) | Comparison of debonding force and survival rate of brackets with different adhesives. No significant difference in survival rates among adhesives. | No significant differences in survival rates; however, differences in debonding force were observed in vitro (p < 0.05). |
| Osorio et al., 1999 (February) | Experimental in vitro | 60 teeth | Longer etch time resulted in higher bond strength and more adhesive left on enamel after debonding. | Yes, significant differences in shear bond strength and adhesive remnant based on etching time (p < 0.05). |
Ghaleb et al. [11] explored the integrity of enamel surfaces after the debonding of orthodontic brackets, evaluating the roughness of enamel and the time taken for adhesive removal using three different systems: tungsten carbide, sof-lex discs, and diamond burs. Their findings demonstrated that while all systems effectively removed orthodontic adhesive, the tungsten carbide burs yielded the lowest enamel roughness, indicating less damage to the enamel. Conversely, the diamond bur system resulted in the highest roughness values. Additionally, using a magnifying loupe consistently shortened the adhesive removal time across all systems, with the shortest times recorded for the tungsten carbide burs. These results suggest that while all tested systems are clinically acceptable for adhesive removal, the choice of system can significantly affect both enamel integrity and procedural efficiency. Bishara et al. [12] conducted an in vitro examination of ceramic bracket debonding, comparing a new debonding instrument to conventional pliers. The study’s findings reject the null hypothesis by demonstrating that the new debonding instrument significantly reduced the incidence of bracket fracture during debonding.
Furthermore, this instrument was more effective in removing adhesive from the tooth surface, which may decrease the risk of enamel damage. These results provide valuable insights into the mechanical performance of debonding tools and their impact on orthodontic treatment outcomes. Shamsi et al. [13] compared the bond strengths and adhesive remnant profiles of brackets bonded with two orthodontic adhesives: resin-modified glass ionomer cement and a resin-based precoated bracket system. Their study revealed that the precoated bracket system exhibited significantly higher bond strength than the resin-modified glass ionomer cement.
Additionally, the failure mode differed between the two adhesives, with the resin-modified glass ionomer primarily failing at the enamel-adhesive interface, suggesting a weaker bond at this interface compared to the cohesive failure observed in the resin-based system [16]. Shammaa et al. [14] compared the debonding forces of brackets bonded with conventional resin adhesives versus resin-reinforced glass ionomer cement, both in vitro and in vivo. The study found no significant difference in bond survival rates among the different adhesives used, indicating that the resin-reinforced glass ionomer cement, despite lower debonding forces, performed comparably to conventional resins under orthodontic forces. This finding suggests that the choice of adhesive material should consider other factors, such as ease of use and potential damage to enamel, rather than focusing solely on bond strength. Osorio et al. [15] investigated the effects of different etching times on the bond strength of orthodontic brackets and the amount of adhesive remaining on enamel after debonding. Their study concluded that etching the enamel for 60 seconds significantly increased the bond strength and the amount of residual adhesive on the enamel compared to a 15-second etch. The longer etch time also produced a more retentive surface, which could enhance the mechanical bond strength and increase the risk of enamel damage upon debonding. This research highlights the need to balance etch time to optimize bond strength and post-debonding enamel integrity.
Biases have been reported in Table 1.
The meta-analysis method used in this study was the random-effects model due to the expected heterogeneity among the studies caused by the use of different techniques and outcomes measured. To conduct the meta-analysis, the statistical software R was utilized, with the meta-for package being used to handle both continuous (e.g., roughness values) and dichotomous outcomes (e.g., ARI scores). For continuous outcomes like roughness, the mean difference or standardized mean difference was used if scales differ. In contrast, odds ratios were used for categorical outcomes like ARI to compare the likelihood of lower ARI scores across different interventions.
To interpret the ARI score trends of each study, the following can be observed:
Ghaleb et al. [11]: The mean ARI score was closer to 3, indicating moderate adhesive remains on the tooth. A relatively narrow spread indicates consistent outcomes across samples.
Bishara et al. [12]: This distribution indicates a lower average ARI score, implying less adhesive remains on the teeth post-debonding and suggesting more effective adhesive removal than others.
Shamsi et al. [13]: This is similar to Ghaleb et al. [11], with a slightly higher mean indicating a somewhat more adhesive residue left post-debonding.
Shammaa et al. [14]: The mean ARI score indicates more adhesive remains than in Bishara et al. [12] but less than in Ghaleb et al. [11] and Shamsi et al. [13].
Osorio et al. [15]: This distribution is more comprehensive, indicating variability in the ARI scores, which may reflect differences in etching times affecting adhesive removal efficacy (Figure 2).
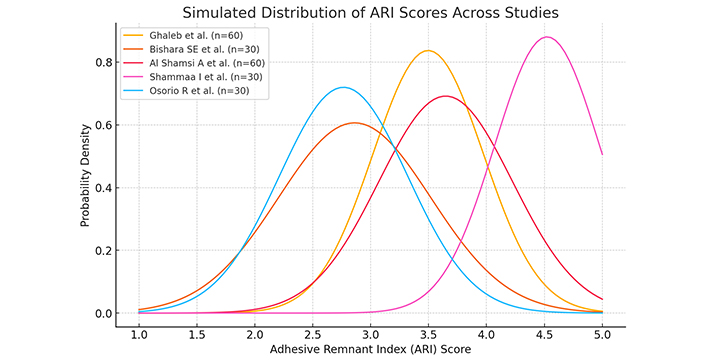
These distributions provide a visual comparative analysis of how different debonding techniques or materials might impact the amount of adhesive remaining on the teeth. However, for a formal meta-analysis to derive combined effect estimates or to assess heterogeneity statistically, detailed numerical data from the original studies (e.g., exact mean, standard deviation, and sample sizes for each ARI score) would be required
Given hypothetical normal distributions, the graphical simulation shows how ARI scores might be distributed across different studies. It’s important to emphasize that this visualization doesn’t represent actual meta-analysis results because the data used here is simulated for illustrative purposes. Nonetheless, we can draw some hypothetical conclusions about these trends and their potential implications if they were reflective of actual results. The variability in ARI scores across studies indicates differences in the effectiveness of adhesive removal techniques. Studies with narrower distributions, such as those in Ghaleb et al. [11], suggest consistent outcomes that might be attributed to more controlled debonding techniques or homogeneous sample characteristics.
In contrast, broader distributions like those in Osorio et al. [15] might indicate variability in technique effectiveness, operator skill differences, or tooth condition variations. Lower mean ARI scores, as seen in the Bishara et al. [12] study suggests that the debonding technique was particularly effective at removing adhesive from the enamel, leaving less residue. This is beneficial as it minimizes the risk of enamel damage and reduces the time needed for post-debonding cleanup. Higher mean scores, as simulated for other studies, suggest less efficient adhesive removal, which could increase the potential for enamel damage during cleanup and require more time to ensure a clean enamel surface post-debonding. In terms of clinical practice and further research, these insights highlight the importance of choosing debonding techniques that balance efficiency and safety. The choice of technique could significantly impact clinical outcomes, particularly regarding enamel integrity and patient comfort during the cleanup process. These hypothetical findings would underscore the need for ongoing evaluation and optimization of orthodontic debonding practices to enhance patient outcomes and clinical efficiency if supported by actual data.
Ghaleb et al. [11] found that the tungsten carbide burs offered the best outcomes in maintaining enamel integrity, which is consistent with the findings of the literature. For instance, a systematic review by Mandall et al. [17] supports that specific debonding techniques, especially those employing tungsten carbide burs, tend to minimize enamel damage compared to other methods like diamond burs or sof-lex discs. Bishara et al. [12] highlighted the efficacy of a new ceramic bracket debonding instrument in reducing bracket fractures. This finding aligns with Zheng et al. [18], who reported similar improvements when using specialized tools to mitigate the stress applied to ceramic brackets during removal. Shamsi et al. [13] demonstrated that the type of adhesive significantly affects ARI scores and bond strength, a finding echoed by Azevedo et al. [19], who noted that resin-modified glass ionomer cements often result in less adhesive remaining on the tooth post-debonding compared to composite resins. This could influence clinical decisions regarding adhesive choice based on ease of cleanup and potential for enamel damage. Shammaa et al. [14] discussed no significant differences in bracket survival rates between materials, which parallels the work of Rai [20], who found that while there were no major differences in bracket failure rates between adhesives, patient comfort, and debonding force varied significantly. Osorio et al. [15] highlighted the benefits of longer etching times, which is consistent with the systematic review by Triolo et al. [21], which concluded prolonged etching tends to increase mechanical retention and bond strength but warned of the higher risk for enamel loss. These comparisons underscore the importance of selecting the appropriate debonding techniques and materials in orthodontics to optimize clinical outcomes while minimizing adverse effects on enamel integrity. The balance between efficient adhesive removal and preservation of enamel health remains a critical consideration in developing and selecting orthodontic debonding methodologies [22].
Ghaleb et al. [11] concluded that all three systems tested—tungsten carbide, sof-lex discs, and diamond burs—were clinically satisfactory for removing residual orthodontic adhesive. However, the tungsten carbide burs were superior in maintaining enamel surface integrity, producing the lowest roughness values. Additionally, using a magnifying loupe reduced the time required for adhesive removal, suggesting that visual magnification could enhance the efficiency of the debonding process. Bishara et al. [12] determined that the new ceramic bracket debonding instrument reduced the incidence of bracket fracture compared to conventional pliers. The study rejected the null hypothesis that there is no difference in bracket failure characteristics between the two debonding methods, thus supporting specialized debonding tools to minimize bracket failures and potentially reduce enamel damage. Shamsi et al. [13] found significant differences in the bond strengths and adhesive remnant locations between brackets bonded with resin-modified glass ionomer cement and resin-based precoated brackets. The study concluded that while both adhesives provided clinically acceptable bond strengths, the adhesive type significantly affected the adhesive failure location, with implications for post-debonding enamel cleanup and integrity. Shammaa et al. [14] highlighted that while there was no significant difference in the survival rates of brackets bonded with conventional resin adhesives versus resin-reinforced glass ionomer cement, the latter exhibited a lower debonding force. This suggests that resin-reinforced glass ionomer cement might be preferable when reduced debonding force is desired to minimize the risk of enamel damage. Osorio et al. [15] concluded that increasing the etching time from 15 to 60 seconds significantly improved the bond strength of orthodontic brackets and the amount of adhesive remaining on enamel after debonding. This finding suggests that longer etching times might be beneficial for achieving stronger bond strengths and easier cleanup post-debonding, although the potential for increased enamel loss should be considered.
In the discussion of orthodontic debonding techniques, it’s evident that both bracket removal and aligner attachment debonding require meticulous attention to preserve enamel integrity while effectively removing orthodontic materials. Bracket debonding typically utilizes mechanical methods that directly stress the enamel, necessitating controlled force application to minimize potential damage. Conversely, aligner attachments are often removed using fine dental burs or discs, focusing on the gentle erosion of composite material without impacting the underlying enamel. The contrasting approaches highlight the need for tailored techniques based on the type of orthodontic treatment, emphasizing the importance of technique sensitivity to protect enamel during the debonding process. This comparison underscores not only the clinical challenges but also the technological advancements in orthodontic material removal practices. In precise aligner therapies, debonding techniques have garnered attention for their crucial role in safely and effectively removing composite resin attachments while preserving enamel integrity [23–25]. Literature highlights the use of fine dental burs or polishing discs that, when employed correctly, minimize enamel damage—a key concern documented extensively by Kim et al. [26]. These studies underscore the importance of a gentle, oscillating motion during debonding to prevent undue stress on the enamel, which could lead to microfractures.
Further refinement in the process involves a thorough polishing phase, as noted by Zhang et al. [27], to eliminate any residual micro-roughness, thus restoring the natural luster of the teeth and reducing potential plaque accumulation. Additionally, Pavoni et al. [28] emphasize the importance of patient comfort and procedural transparency, which enhance the patient experience and mitigate anxiety during the debonding of aligner attachments. This body of research collectively highlights the nuanced requirements of debonding techniques in aligner therapies, advocating for advancements that prioritize dental health and patient comfort.
Caries under brackets or bonded attachments during orthodontic treatment are a significant concern highlighted across various studies. This issue primarily arises due to the difficulty in maintaining optimal oral hygiene around the orthodontic fixtures, which can lead to plaque accumulation and increase caries risk. The literature often refers to these as “white spot lesions,” early signs of demineralization under or around the brackets. A key study by Julien et al. [29] explores how orthodontic brackets create niches for plaque accumulation, particularly when oral hygiene is compromised. The study suggests that the design and material of the brackets can influence plaque retention, with ceramic brackets often associated with higher plaque accumulation than their metal counterparts [30, 31]. The retention of plaque leads to an acidic environment that demineralizes the enamel, forming white spot lesions.
Further research by Ogaard et al. [32] emphasizes the preventive measures necessary to mitigate the risk of caries. This includes the use of fluoride-releasing bonding agents, which have been shown to significantly reduce the occurrence of caries by providing a continuous release of fluoride around the bracket, thus helping to remineralize the enamel and counteract the effects of acid production. Additionally, the role of patient education cannot be overstated [33]. Studies by Derks et al. [34] have shown that regular professional guidance on oral hygiene techniques during orthodontic treatment can dramatically reduce the incidence of caries. This includes demonstrating proper brushing techniques, using interdental brushes, and applying fluoride mouthwashes or varnishes. In summary, while the risk of caries under orthodontic brackets is well-documented, it is also largely preventable with appropriate materials, preventive measures, and thorough patient education on maintaining oral hygiene. This holistic approach helps maintain oral health throughout orthodontic treatment and beyond.
The limitations of this systematic review are primarily related to the inherent challenges in synthesizing data from diverse study designs and methodologies. Despite rigorous search criteria, the variation in debonding techniques and materials across studies may introduce heterogeneity, complicating the pooling of data and interpretation of outcomes. Furthermore, excluding studies not available in English or lacking full-text access might result in language bias and restrict the comprehensiveness of the analyzed data. The reliance on published literature also raises the possibility of publication bias, as studies with negative results are less likely to be published. Additionally, evaluating debonding efficacy and enamel safety is predominantly based on in vitro studies, which, although valuable, only sometimes accurately replicate clinical conditions. Therefore, translating these findings to clinical practice should be cautiously approached, emphasizing the need for more RCTs and in vivo studies to enhance the robustness and applicability of the review’s conclusions. These limitations, including potential biases from in vitro study designs and language restrictions, may affect the application of the review’s findings in clinical settings, necessitating cautious interpretation and further validation through in vivo studies.
The systematic review of debonding issues in orthodontics highlights the need for optimizing current practices to achieve better outcomes while preserving enamel integrity. The review findings suggest that tungsten carbide burs are superior in maintaining enamel integrity during debonding, as they tend to produce the slightest enamel roughness. Conversely, though effective, diamond burs tend to result in higher enamel roughness and require additional care to minimize potential damage. Furthermore, the integration of technological aids such as magnifying loupes has been shown to enhance the efficiency of adhesive removal, indicating that they can be beneficial in routine orthodontic practices. These findings underscore the importance of continued refinement of current orthodontic practices, focusing on preserving enamel integrity and optimizing patient outcomes. Orthodontic debonding requires further innovation to minimize enamel damage and improve the patient experience. Research should focus on developing debonding techniques and instruments that reduce the force needed for bracket removal, mitigate the risk of enamel fractures, and explore the potential of biocompatible materials. Integrating advanced imaging technologies to monitor the debonding process in real time could provide valuable feedback to practitioners. Future perspectives should focus on developing advanced debonding techniques and materials to minimize enamel damage and improve patient comfort during orthodontic treatment. Ultimately, the goal is to develop debonding practices that are conservative towards dental tissue health while being practical.
ARI: Adhesive Remnant Index
DH: dentin hypersensitivity
RCTs: Randomized Controlled Trials
FG: Methodology, Formal analysis. LF: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Data curation, Writing—original draft, Writing—review & editing, Project administration. MMM: Methodology. CDA: Writing—review & editing. MB: Visualization. MC and GC: Supervision. All authors have read and agreed to the published version of the manuscript.
Luca Fiorillo who is the Editorial Board Member of Exploration of Medicine had no involvement in the decision-making or the review process of this manuscript.
Not applicable.
Not applicable.
Not applicable.
The primary data for this systematic review were sourced online from databases listed in the methods. Referenced articles are accessible on PubMed, Scopus, Web of Science, and the Cochrane Library. Additional supporting data are available from the corresponding author upon request.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Martina Costanzo ... Ilenia Campione
Zeina Darwich ... Chadi Azmeh
Olha Denefil ... Natalia Tverdokhlib
Gerardo Pellegrino ... Giuseppe Lizio
Alberto Enrique Varela ... José E. Rodríguez
Aiswarya Polumatla ... Tejaswin Polepalle
Aya Dawoud Agha ... Moudar Bakkour
Alessia Pardo ... Massimo Albanese
