Affiliation:
1Department of Periodontology, SIBAR Institute of Dental Sciences, Guntur 522509, Andhra Pradesh, India
Affiliation:
1Department of Periodontology, SIBAR Institute of Dental Sciences, Guntur 522509, Andhra Pradesh, India
Email: anumala.deepas@gmail.com
ORCID: https://orcid.org/0000-0003-4334-8173
Affiliation:
1Department of Periodontology, SIBAR Institute of Dental Sciences, Guntur 522509, Andhra Pradesh, India
ORCID: https://orcid.org/0000-0003-4103-455X
Affiliation:
1Department of Periodontology, SIBAR Institute of Dental Sciences, Guntur 522509, Andhra Pradesh, India
ORCID: https://orcid.org/0000-0003-2002-4352
Affiliation:
1Department of Periodontology, SIBAR Institute of Dental Sciences, Guntur 522509, Andhra Pradesh, India
ORCID: https://orcid.org/0000-0002-9196-0183
Affiliation:
2Department of Periodontology, Faculty of Dentistry, MAHSA University, Jenjarom 42610, Malaysia
ORCID: https://orcid.org/0000-0002-0904-577X
Explor Med. 2024;5:833–842 DOI: https://doi.org/10.37349/emed.2024.00258
Received: July 01, 2024 Accepted: October 18, 2024 Published: November 14, 2024
Academic Editor: Giuseppe Minervini, University of Campania “Luigi Vanvitelli”, Italy
The article belongs to the special issue Oral Health Interconnections and Multidisciplinary Approaches
Aim: Periodontal diseases are prevalent and can be exacerbated by conditions such as obesity. Understanding the impact of obesity on periodontal health is crucial for developing effective management strategies. This study aimed to evaluate the effect of nonsurgical periodontal therapy on salivary visfatin levels and serum lipid levels in chronic periodontitis patients with or without obesity.
Methods: A total of 40 patients aged between 20 to 50 years were enrolled in the study. Group 1 (obese group) included 20 chronic periodontitis patients with obesity while Group 2 (non-obese group) included 20 chronic periodontitis patients without obesity. Gingival index (GI), probing depth (PD), clinical attachment level (CAL), salivary visfatin, and serum lipid levels were measured before and six weeks after nonsurgical periodontal therapy (NSPT). Statistical tests were done to analyze the data in the study.
Results: Mean GI scores, mean PD scores, and mean CAL scores were significantly reduced before and 6 weeks after NSPT in both groups (p < 0.05). The mean salivary visfatin levels also demonstrated a statistically significant reduction between the obese and non-obese groups (p < 0.05). Similarly, the mean serum lipid levels significantly differed before and 6 weeks after NSPT in the obese group (p < 0.05).
Conclusions: The current study suggests a significant correlation between GI, PD, CAL, salivary visfatin, and serum lipid levels in the obese group following NSPT.
Periodontitis is a chronic multifactorial disease that affects the tissues that surround the teeth and is characterized by the overproduction of tissue-destructive molecules and inflammatory mediators against periodontal pathogens [1]. Individuals with periodontitis often connect to systemic conditions such as diabetes, coronary heart disease (CHD), preterm birth, and obesity [2].
This correlation seems rooted in a shared low-grade inflammatory burden, indicating a common underlying pathophysiological mechanism linking periodontal disease to systemic conditions [3].
Obesity is a systemic condition characterized by an excessive accumulation of adipose tissue, which has significant health implications [4]. Adipose tissue is not merely a fat storage reservoir but also a dynamic endocrine organ that releases various biologically active substances [5]. These include hormones and pro-inflammatory cytokines, collectively known as adipokines, such as resistin, visfatin, leptin, and adiponectin [6]. These adipokines play crucial roles in inflammatory processes and metabolic regulation. Adipose tissue dysfunction triggers inflammatory pathways and induces oxidative stress, establishing a parallel pathophysiological connection between obesity and periodontitis [7]. Additionally, dyslipidemia, characterized by abnormal serum lipid levels, is commonly observed in obese individuals and is known to be influenced by inflammatory processes [8].
The review article by Kandhan TS and Rajasekar A [9] sheds light on the prevalence of periodontal disease associated with obesity. Understanding the intricate relationship between obesity and periodontal disease is essential for advancing awareness and enhancing primary care strategies. The review highlights the need for novel diagnostic approaches to identify these conditions at early stages and to monitor their progression effectively [9].
Saliva is a crucial biological fluid that contains a range of biomarkers, both locally and systemically derived, which are essential for detecting periodontitis [10]. Elevated visfatin levels in saliva have been associated with inflammation, suggesting that visfatin could serve as a biomarker for assessing the link between chronic periodontitis and obesity [11]. The identification of inflammatory biomarkers like visfatin in saliva can help in recognizing the presence of periodontitis by evaluating the risk and understanding its association with obesity.
The success of periodontal treatment primarily hinges on the thorough removal of supra- and subgingival biofilm from the teeth, as well as effective patient self-care, to prevent biofilm formation. According to guidelines from the European Federation of Periodontology (EFP), nonsurgical periodontal therapy (NSPT), including traditional quadrant-wise subgingival instrumentation (Q-SI) performed over multiple appointments scheduled 1 to 4 weeks apart, is a key approach for managing periodontitis [12].
The potential impact of NSPT on systemic inflammatory markers, such as salivary visfatin and serum lipid profiles, in obese patients with chronic periodontitis remains largely unexplored. Since both periodontitis and obesity independently elevate visfatin levels, understanding how NSPT affects this adipokine is crucial for revealing potential roles in reducing the systemic inflammatory burden and improving metabolic health in this population [13]. To better evaluate the influence of obesity on the responses to NSPT and to enhance the study’s validity, a control group of patients with chronic periodontitis without obesity was included for comparison. Thus, the current study aimed to evaluate the effect of NSPT on salivary visfatin levels and serum lipid profiles in chronic periodontitis patients with or without obesity.
Forty patients diagnosed with chronic periodontitis were selected from the Outpatient Department of Periodontics at SIBAR Institute of Dental Sciences, Guntur. The study was conducted between 2021 and 2022. The study protocol was explained to the patients, and written informed consent was obtained after approval from the institutional ethics committee (Pr.36/IEC/SIBAR/2021).
Based on clinical and radiographic examinations, the diagnosis of chronic periodontitis was established according to the 1999 classification of periodontal diseases by Armitage GC [1]. The study population was randomly assigned into two groups using a computer-generated randomization sequence. Each group contained 20 participants. Group 1 included 20 chronic periodontitis patients with obesity, Group 2 included 20 chronic periodontitis patients without obesity. Randomization was stratified by obesity to ensure an equal distribution of patients with or without obesity between the groups. Figure 1 shows the CONSORT flow diagram of the study.
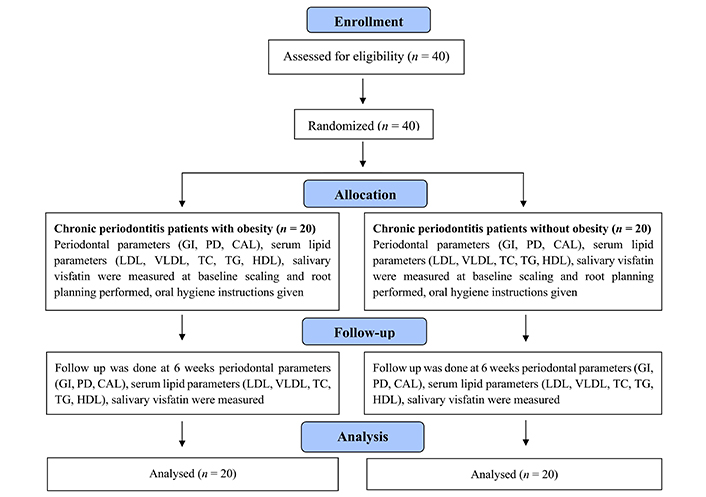
CONSORT flow diagram. CAL: clinical attachment level; GI: gingival index; PD: probing depth
The sample size for this study was determined using G*Power 3.1.9.2 software. G*Power is a widely used tool for statistical power analysis, developed by a team of researchers at the Universität Düsseldorf (Heinrich-Heine-Universität Düsseldorf), Germany, including Franz Faul, Edgar Erdfelder, Axel Buchner, and Albrecht-Georg Lang. With an effect size of 1.7, α of 0.05, and 80% power, it was indicated that 40 participants were sufficient to ensure reliable and valid results.
Patients diagnosed with chronic periodontitis, having at least 20 natural teeth, and aged between 20 to 50 years, were included in both groups. Participants exhibited clinical measurements of probing depth (PD) ≥ 4 mm, clinical attachment level (CAL) ≥ 5 mm, and radiographic evidence of bone loss consistent with chronic periodontitis. Those in the obesity group exhibited a BMI of ≥ 30 kg/m2 and waist circumference exceeding 80 cm for women or 90 cm for men [14]. Patients with other periodontal diseases, systemic conditions, smoking, alcohol or tobacco use, pregnancy, breastfeeding, recent periodontal therapy (within the last 6 months), or medications affecting periodontal health and cholesterol were excluded.
Participants were asked to fast for at least 2 hours before saliva collection. Unstimulated saliva was obtained by spitting. Saliva was collected in sterile tubes and promptly frozen at –70°C until further use. Upon thawing, the quantity of visfatin was measured using an ELISA kit. Elabscience Human VF (visfatin) ELISA kit from the USA was employed to determine salivary visfatin concentrations.
Blood samples were obtained from an antecubital vein following a 12-hour fasting period to measure serum lipid parameters such as LDL, VLDL, HDL, TC, and TG. These assessments were conducted at the Clinical Biochemistry Laboratory (Zed Labs, Guntur City) using standard enzymatic methods.
The clinical oral examination and sample collection were performed by single-calibrated periodontists to ensure consistency and homogeneity. All patients underwent a thorough clinical examination, during which periodontal parameters including gingival index (GI) [15], PD [16], and CAL [16] were measured using a University of North Carolina-15 probe (UNC-15 probe). Blood and saliva samples were collected, and later scaling was performed with the initiation of oral hygiene instructions. Within 2 weeks root planning procedure was also completed. The standardized plaque scoring method was employed to evaluate oral hygiene levels among participants in both the obese and non-obese groups to control for variations in oral hygiene [15]. Oral hygiene quality was evaluated throughout the study by collecting self-reported data from patients regarding their adherence to oral hygiene routines, including brushing and flossing frequency, and technique. Patients were recalled at 6-week follow-up, periodontal parameters were recorded, and blood and saliva samples were collected and analyzed for serum lipid profiles and salivary visfatin levels.
The data was analyzed by SPSS version 20 software (IBM Corp., Armonk, NY, USA). Statistical analyses were performed using standard methods to ensure clarity and accuracy. Descriptive statistics, including mean and standard deviation, were used to summarize baseline characteristics and outcomes. Differences between groups were assessed using independent t-tests for continuous variables and chi-square tests for categorical variables. Changes in periodontal parameters and serum lipid profiles before and 6 weeks after NSPT were analyzed using paired t-tests. All statistical tests were two-tailed, and p < 0.05 was considered statistically significant.
Table 1 compares the demographic characteristics and anthropometric measurements between the obese and non-obese groups. The mean age of participants, as determined by the independent samples t-test, was similar between the two groups (37 years), with no statistically significant difference. Gender distribution was assessed using the chi-square test and showed no significant differences between the groups. In terms of anthropometric measurements, significant disparities were observed. The independent samples t-test revealed that the mean BMI was significantly higher in the obese group (31.93 ± 1.40 kg/m2) compared to the non-obese group (21.61 ± 2.06 kg/m2), with a t-value of 18.45 and a p-value < 0.05. Similarly, the waist circumference was significantly greater in the obese group (90.50 ± 7.87 cm) than in the non-obese group (78.65 ± 6.08 cm), with a t-value of 5.32 and a p-value < 0.05.
Comparison of demographics, body mass index, and waist circumference between obese and non-obese groups
| Parameter | Group | N | Mean | SD | SEM | t-value | p-value | Male (%) | Female (%) | Chi-square value | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Obese | 20 | 37.75 | 6.40 | 1.43 | 0.37 | 0.70 | 9 (45.00) | 11 (55.00) | 0.10 | 0.75 |
| Non-obese | 20 | 37.05 | 5.32 | 1.19 | 10 (50.00) | 10 (50.00) | |||||
| Body mass index (kg/m2) | Obese | 20 | 31.93 | 1.40 | 0.31 | 18.45 | < 0.05* | ||||
| Non-obese | 20 | 21.61 | 2.06 | 0.46 | |||||||
| Waist circumference (cm) | Obese | 20 | 90.50 | 7.87 | 1.76 | 5.32 | < 0.05* | ||||
| Non-obese | 20 | 78.65 | 6.08 | 1.36 |
p < 0.05 is considered statistically significant for both the independent samples t-test (mean age, body mass index, waist circumference) and the chi-square test (gender); *: denotes significance
Table 2 represents the intragroup comparison of mean GI scores, mean PD scores, and mean CAL scores before and after NSPT. At baseline, the mean GI scores were 1.86 ± 0.55 and 1.80 ± 0.44 in the obese group and non-obese group, respectively. At 6 weeks, the mean GI scores were 1.03 ± 0.23 and 0.83 ± 0.30 in the obese group and non-obese group, respectively. There was a significant reduction in the mean GI scores before and 6 weeks after NSPT in both study groups (p < 0.05). At baseline, the mean PD scores were 5.48 ± 0.47 and 5.33 ± 0.89 in the obese group and non-obese group, respectively. At 6 weeks, the mean PD scores were 4.32 ± 0.25 and 4.25 ± 0.77 in the obese group and non-obese group, respectively. There was a significant reduction in the mean PD scores before and 6 weeks after NSPT in both study groups (p < 0.05). At baseline, the mean CAL scores were 6.17 ± 0.89 and 6.09 ± 1.19 in the obese group and non-obese group, respectively. At 6 weeks, the mean CAL scores were 5.10 ± 0.94 and 5.11 ± 0.88 in the obese group and non-obese group, respectively. There was a significant reduction in the mean CAL scores before and 6 weeks after NSPT in both study groups (p < 0.05).
Intragroup comparison of mean gingival index (GI) scores, mean probing depth (PD) scores, and mean clinical attachment level (CAL) scores from baseline to 6 weeks
| Indices | Group | Time | N | Mean | SD | t-value | p-value |
|---|---|---|---|---|---|---|---|
| GI | Obese | Baseline | 20 | 1.86 | 0.55 | 8.34 | < 0.05* |
| 6 weeks | 20 | 1.03 | 0.23 | ||||
| Non-obese | Baseline | 20 | 1.80 | 0.44 | 10.28 | < 0.05* | |
| 6 weeks | 20 | 0.83 | 0.30 | ||||
| PD | Obese | Baseline | 20 | 5.48 | 0.47 | 12.56 | < 0.05* |
| 6 weeks | 20 | 4.32 | 0.25 | ||||
| Non-obese | Baseline | 20 | 5.33 | 0.89 | 5.87 | < 0.05* | |
| 6 weeks | 20 | 4.25 | 0.77 | ||||
| CAL | Obese | Baseline | 20 | 6.17 | 0.89 | 7.94 | < 0.05* |
| 6 weeks | 20 | 5.10 | 0.94 | ||||
| Non-obese | Baseline | 20 | 6.09 | 1.19 | 5.85 | < 0.05* | |
| 6 weeks | 20 | 5.11 | 0.88 |
Paired samples t-test; p < 0.05 considered statistically significant; *: denotes significance
Table 3 represents the intergroup comparison of mean GI scores, mean PD scores, and mean CAL scores in the obese and non-obese groups. No significant difference was observed in mean GI scores, mean PD scores, and mean CAL scores between the groups.
Comparison of mean gingival index (GI) scores, mean probing depth (PD) scores, and mean clinical attachment level (CAL) scores between the obese and non-obese groups at baseline and 6 weeks
| Parameter | Time | Group | N | Mean | SD | SEM | t-value | p-value |
|---|---|---|---|---|---|---|---|---|
| GI | Baseline | Obese | 20 | 1.86 | 0.55 | 0.12 | 0.34 | 0.73 |
| Non-obese | 20 | 1.80 | 0.44 | 0.09 | ||||
| 6 weeks | Obese | 20 | 1.03 | 0.23 | 0.05 | 2.01 | 0.06 | |
| Non-obese | 20 | 0.83 | 0.30 | 0.06 | ||||
| PD | Baseline | Obese | 20 | 5.48 | 0.47 | 0.10 | 0.62 | 0.53 |
| Non-obese | 20 | 5.33 | 0.89 | 0.20 | ||||
| 6 weeks | Obese | 20 | 4.32 | 0.25 | 0.05 | 0.39 | 0.69 | |
| Non-obese | 20 | 4.25 | 0.77 | 0.17 | ||||
| CAL | Baseline | Obese | 20 | 6.17 | 0.89 | 0.20 | 0.24 | 0.80 |
| Non-obese | 20 | 6.09 | 1.19 | 0.26 | ||||
| 6 weeks | Obese | 20 | 5.10 | 0.94 | 0.21 | –0.03 | 0.97 | |
| Non-obese | 20 | 5.11 | 0.88 | 0.19 |
Independent samples t-test; p < 0.05 considered statistically significant
Table 4 shows the mean salivary visfatin levels in the obese and non-obese groups. At baseline, the salivary visfatin levels were 17.73 ± 0.90 ng/mL in the obese group and 13.06 ± 1.02 ng/mL in the non-obese group, with a statistically significant difference observed between the groups (p < 0.05). At 6 weeks after NSPT, the mean salivary visfatin levels were 16.76 ± 0.84 ng/mL in the obese group and 12.01 ± 0.98 ng/mL in the non-obese group, with a statistically significant difference observed between the obese and non-obese groups (p < 0.05).
Comparison of mean visfatin levels (ng/mL) between the obese and non-obese groups
| Time | Group | N | Mean | SD | SEM | t-value | p-value |
|---|---|---|---|---|---|---|---|
| Baseline | Obese | 20 | 17.73 | 0.90 | 0.20 | 15.30 | < 0.05* |
| Non-obese | 20 | 13.06 | 1.02 | 0.22 | |||
| 6 weeks | Obese | 20 | 16.76 | 0.84 | 0.18 | 16.40 | < 0.05* |
| Non-obese | 20 | 12.01 | 0.98 | 0.21 |
Independent samples t-test; p < 0.05 considered statistically significant; *: denotes significance
Table 5 shows the intragroup comparison of mean LDL, VLDL, TC, TG, and HDL levels in the obese group from baseline to 6 weeks after NSPT. At baseline, higher LDL, VLDL, TC, and TG levels and lower HDL levels were found. At 6 weeks, lower LDL, VLDL, TC, and TG levels and higher HDL levels were found. A statistically significant difference was observed before and 6 weeks after NSPT in the obese group (p < 0.05).
Comparison of mean LDL, VLDL, TC, TG, and HDL levels between baseline and 6 weeks in the obese group
| Parameter | Group | N | Mean | SD | SEM | t-value | p-value |
|---|---|---|---|---|---|---|---|
| LDL | Baseline | 20 | 114.05 | 8.36 | 1.87 | 5.06 | < 0.05* |
| 6 weeks | 20 | 97.05 | 12.50 | 2.80 | |||
| VLDL | Baseline | 20 | 39.50 | 4.38 | 0.98 | 5.63 | < 0.05* |
| 6 weeks | 20 | 33.40 | 2.06 | 0.46 | |||
| TC | Baseline | 20 | 182.45 | 9.77 | 2.18 | 4.45 | < 0.05* |
| 6 weeks | 20 | 168.65 | 9.84 | 2.20 | |||
| TG | Baseline | 20 | 198.55 | 21.65 | 4.84 | 5.53 | < 0.05* |
| 6 weeks | 20 | 168.60 | 10.90 | 2.43 | |||
| HDL | Baseline | 20 | 40.15 | 1.07 | 0.23 | 4.45 | < 0.05* |
| 6 weeks | 20 | 41.65 | 1.13 | 0.25 |
Paired t-test; p < 0.05 considered statistically significant; *: denotes significance
Periodontal medicine has emerged as mounting evidence that periodontitis is linked to systemic disorders, including diabetes, CHD, preterm birth, and obesity. Obesity is identified as either an independent risk factor or an aggravating risk factor that is widely considered as one of the important major health risks in the modern world. Recent research has shown that obesity and periodontal disease share a common link in the inflammatory process and pathogenesis [17].
Visfatin exhibits potent destructive and proinflammatory properties, playing a significant role in sustaining inflammation by inhibiting apoptosis and activating neutrophils [18]. Visfatin exhibits insulin-mimetic properties by stimulating the phosphorylation of insulin receptor substrates 1 and 2 in human osteoblasts. This enhances glucose uptake, promotes cell proliferation, increases type I collagen production, and induces angiogenesis [19]. In response to IL-1β, visfatin levels increase in chondrocytes, where it acts locally in an autocrine and paracrine manner, contributing to the synthesis of prostaglandin E2 (PGE-2) [20]. These functions highlight visfatin’s dual role as an inflammatory mediator and a modulator of metabolic processes, underscoring its potential significance in various pathological conditions involving inflammation and tissue remodeling [21].
Effective periodontal therapy can decrease markers of oxidative stress, which are typically elevated in periodontitis. This reduction is associated with a decrease in the inflammatory burden, thus potentially lowering the risk of further oxidative damage to periodontal tissues and systemic health. Early and effective periodontal intervention is crucial not only for controlling local inflammation but also for preventing systemic implications and enhancing overall patient well-being. Therefore, the purpose of the current study was to evaluate the link between obesity and periodontitis by utilizing BMI, waist circumference, and periodontal parameters (GI, PD, CAL) as indices and salivary visfatin levels, and serum lipid levels respectively.
The current study showed high levels of salivary visfatin and serum lipid levels with high LDL, VLDL, TC, TG, and low HDL levels at baseline. Six weeks after NSPT a significant decrease in salivary visfatin and serum lipid levels with decreased LDL, VLDL, TC, TG, and increased HDL levels was observed in chronic periodontitis patients with obesity and a substantial connection between obesity and periodontitis. Throughout the study, the patients remained obese until the study completion indicating that the decrease in salivary visfatin and serum lipid parameters is probably associated with periodontal therapy.
Duan JY et al. (2009) [22], Fentoğlu O et al. (2010) [23], and Zuza EP et al. (2016) [24] investigated the impact of scaling and root planing on serum lipid levels in periodontitis and hyperlipidemia patients. Their observations revealed that periodontal initial therapy led to a reduction in serum lipid levels among patients with both conditions at 3-month follow-up visits. The present study’s results were in accordance with the above-mentioned research studies [22–24].
Tabari ZA et al. (2014) [25] conducted a study to evaluate the salivary concentrations of visfatin in patients with periodontitis. They found that visfatin was observed in all samples of saliva collected from individuals with chronic periodontitis. These findings suggest that there is an association of salivary visfatin in periodontitis patients. In the present study, salivary visfatin was higher in periodontitis patients and the results were in accordance with Tabari ZA et al. [25].
Abolfazli N et al. (2015) [26] conducted research to evaluate the impact of scaling and root planing on visfatin levels in both serum and saliva among patients with generalized moderate-to-severe periodontitis. The results showed a direct correlation between periodontal inflammation, disease progression, and visfatin levels in both saliva and serum. Current study results were similar to Abolfazli N et al. [26].
Fu YW et al. (2016) [27] conducted research to assess the impact of periodontal therapy on plasma lipids and proinflammatory biomarker levels in periodontitis and hyperlipidemia patients. Their findings indicated thorough periodontal therapy in hyperlipidemia and periodontitis patients led to betterment in serum lipid levels and reduction in circulating proinflammatory biomarker levels. The research concluded that serum lipid levels demonstrated improvement following NSPT at two weeks and six weeks compared to baseline levels. The current study results were similar to Fu YW et al. [27].
Kumar V et al. (2019) [28] conducted research to assess the salivary levels of visfatin in three groups. Group 1 consists of non-obese healthy people, Group 2 consists of obese patients with periodontitis, and Group 3 consists of obese patients without periodontitis. They found that the highest visfatin levels in saliva were observed in obese patients with periodontitis, while the lowest levels were detected in non-obese healthy people. Significant differences in salivary visfatin concentrations were also noted among the three groups. Current study results were similar to those of Kumar V et al. [28].
Recent studies have investigated the relationship between salivary visfatin levels and periodontal disease in the context of obesity. Coutinho A et al. (2021) [29] found that salivary visfatin levels were higher in patients with periodontal disease compared to healthy individuals, suggesting that visfatin could serve as a potential inflammatory biomarker for periodontitis. Ceylan Şen S et al. (2022) [11] found that visfatin levels were higher in obese patients with periodontitis compared to non-obese patients, suggesting a role in increased periodontal damage. Similarly, Rajasekar A (2023) [30] observed a positive association between BMI, salivary visfatin, and periodontal parameters. These findings align with our study, supporting visfatin as a potential biomarker for inflammation in periodontitis, especially among obese patients [11].
Thus, this present study showed higher visfatin levels in the saliva of Group 1 compared to Group 2. Additionally, periodontal therapy effectively decreased salivary visfatin and serum lipid levels in chronic periodontitis patients with obesity contributing to improved oral and systemic health.
Salivary visfatin can be considered as a potential biomarker to identify periodontal disease progression in obese people as well as a possible therapeutic target for evaluating the effectiveness of periodontal therapy. Early and effective periodontal intervention is crucial not only for managing local inflammation but also for preventing systemic complications and improving overall patient health. Future studies could benefit from incorporating objective measures of dietary intake and lifestyle changes to reduce the influence of self-reporting and provide a more accurate assessment of the effects of periodontal therapy on lipid profiles with larger sample sizes and longer follow-up periods.
CAL: clinical attachment level
CHD: coronary heart disease
GI: gingival index
NSPT: nonsurgical periodontal therapy
PD: probing depth
AP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing—original draft, Resources. AD: Conceptualization, Project administration, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing. RD: Conceptualization, Project administration, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing. KKK: Conceptualization, Supervision, Validation, Visualization. RB: Writing—original draft, Validation, Visualization, Writing—review & editing. TP: Conceptualization, Project administration, Supervision, Validation, Visualization.
The authors declare that they have no conflicts of interest.
This study was approved by the SIBAR Institutional Ethical Committee (approval reference number: Pr.36/IEC/SIBAR/2021) and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. All participants provided informed consent prior to their involvement, ensuring they were fully informed about the purpose, procedures, and potential risks of the study.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
The data that support the findings of this study are not publicly available due to privacy concerns and the confidential nature of participant information. In order to protect the privacy of the individuals involved, the data will remain confidential and will not be shared publicly.
Not applicable.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2132
Download: 27
Times Cited: 0
Martina Costanzo ... Ilenia Campione
Zeina Darwich ... Chadi Azmeh
Francesca Gorassini ... Gabriele Cervino
Olha Denefil ... Natalia Tverdokhlib
Gerardo Pellegrino ... Giuseppe Lizio
Alberto Enrique Varela ... José E. Rodríguez
Aya Dawoud Agha ... Moudar Bakkour
Alessia Pardo ... Massimo Albanese
