Affiliation:
1Department of Biomedical and Neuromotor Sciences (DIBINEM), School of Dentistry, University of Bologna, 40126 Bologna, Italy
ORCID: https://orcid.org/0000-0001-8782-8991
Affiliation:
3Surgical, Medical and Dental Department of Morphological Sciences related to Transplant, Oncology and Regenerative Medicine, University of Modena and Reggio Emilia, 41124 Modena, Italy
ORCID: https://orcid.org/0000-0002-3053-5562
Affiliation:
4Private Practice, Private Dental Office, 98123 Messina, Italy
Email: giuseppelizio@libero.it
ORCID: https://orcid.org/0000-0002-7552-7523
Explor Med. 2024;5:887–895 DOI: https://doi.org/10.37349/emed.2024.00263
Received: March 23, 2024 Accepted: September 16, 2024 Published: November 21, 2024
Academic Editor: Giuseppe Minervini, University of Campania “Luigi Vanvitelli”, Italy
The article belongs to the special issue Oral Health Interconnections and Multidisciplinary Approaches
Immediate implant-supported rehabilitation of atrophic maxillae with a fixed screw-retained prosthesis has to deal with the fixtures’ disparallelism and a high risk of fracture of the fixture-abutment connecting screw. After the flapless placement of six implants, with the distal ones inclined at more than 30° to bypass the sinus cavities and reduce the cantilever effects, the provisional prosthesis was immediately connected. The low-profile OT Equator attachment system enabled a trustworthy anchorage of the superstructure without the connection-screws allocation on the rear fixtures. Three months later, all implants were definitively loaded. The patient was monitored for two years follow-up. No problem arose during the whole treatment. The prosthesis maintained its stability and anchorage with complete functional and aesthetic results. No signs of periimplantitis or radiographically evident bone loss were noted. The OT Bridge system successfully simplified the immediate loading of all implants regardless of the inclination of the rear fixtures, avoiding a provisional mobile denture.
The “tilted implants” approach for the fixed full-arch rehabilitation of atrophic maxillae entails the distal inclination of the rear implants anterior to the sinus in association with four [1] or two [2] straight fixtures in the frontal area. The longer the implants, the more stability, thanks to the major bone contact surface and the engagement of denser basal bone of the nasal fossa pavement or the anterior/posterior walls of the sinus cavities [3–7]. A recent review with a follow-up of 5–17 years, reported a 96.93% survival rate out of 1,951 tilted implants in different clinical situations [4]. This datum, comparable to the 96.66% of the axial implants [4], confirmed the results of studies with shorter follow-ups [8–10].
As an alternative, the posterior fixtures, angled anteriorly, are placed in the tuber maxillae and pterygoid lamina [11]. The consequent sagittal disparallelism is often associated with the implant palate-vestibular inclination to compensate for the centripetal resorption [2].
Nevertheless, the inter-implant axial divergence complicates matching with the prosthetic superstructure, mainly when using internal connections. External connections better tolerate minimal implant disparallelism but have drawbacks such as micromovements and bacterial infiltration at the fixture-abutment interface. For these reasons, the internal connection is preferred with parallel implants, allowing the bone level positioning of the fixture neck and the platform-switching practice using smaller diameter abutments [12].
The adoption of short, intermediate elements screwed to the fixture’s shoulder, i.e., the angled Multi-Unit Abutment (MUA) system, copes with the implants’ divergence to obtain a passive fit of the prosthesis [13]. This device strictly depends on a small connecting screw subjected to fracture and unscrewing for the limited allocation space [14–16]. Conical frictional joints, without a connection screw, poorly tolerate implant disparallelism [17–20]. A further alternative can be the use of co-axial implants with an angled connection system in the neck, obtaining a direct fixture-prosthesis matching with a larger connecting screw [21]. Additional intermediate components augment the interfaces favoring bacterial infiltration attacks and periimplantitis [22]. OT Equator joint, matched with a retentive cap, was developed for the implant-retained removable overdentures in cases of relevant implant divergence. The cap, housing a particular nylon component, realizes a tilting mechanism, allowing a passive prosthesis loading even in conditions of up to 50° implant divergence [23]. This connection system is used even in cases of implant-supported removable dentures with the implants splinted together by a metallic bar [24].
The OT Bridge screw-retained system for fixed-screwed protheses adopts the same low-profile joint, the OT Equator, with a newly conceived abutment system called Extragrade, to be embedded in the prosthetic framework [11, 15, 25, 26].
The Extragrade is a standard cylindric and straight abutment housing in its inner coronal surface an interchangeable plastic ring, the Seeger, which confers a substantial sub-equatorial snap-like joint with the fixture up to 50–80° of its inclination (Figures 1, 2). The upright shape of this turret allows the housing of a connection screw bigger than MUA to ensure the implant-abutment coupling. The OT Bridge system demonstrated the same anchoring power as MUA in vitro [13, 25, 27], with, in addition, the “snap” joint component in case of connection screw damage, and obtained only a 1.3% one-year implant failure on fourteen maxillary full-arch immediate rehabilitation [28].
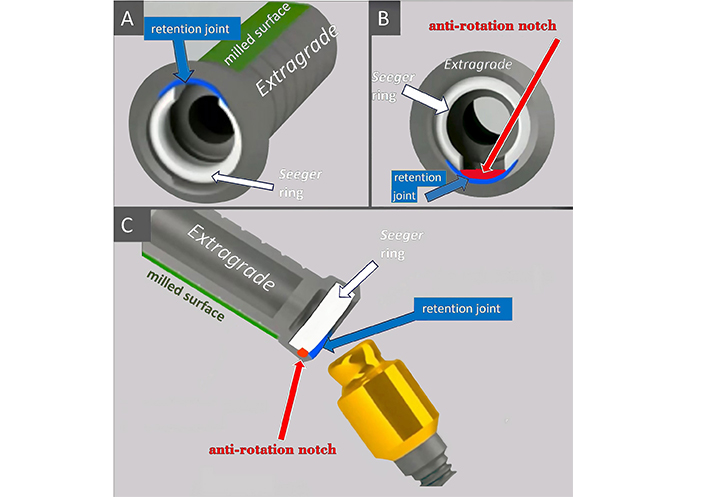
The prosthetic components in three-quarter (A), transversal (B), and longitudinal (C) perspectives. The “Seeger” ring (white) engages the distal undercuts of the inclined abutment in correspondence of its lacking portion, defining with the inner surface of the Extragrade (grey) a snap-retention joint (blue). An anti-rotation notch (orange) in the same zone guarantees the axial steadiness. The external milled surface of the turrets (green) guides their correct positioning
The present paper reports a successful case of immediately loaded implants supporting a full-arch maxillary rehabilitation with “tilted implants”.
A 58-years-old totally edentulous male patient, in generally good condition and a non-smoker, underwent our attention wearing a complete removable restoration in both jaws; the dentures had been delivered approximately two years earlier at our private dental clinic, ZEA Dental Clinic, Imola (BO), Italy, following the extraction of the hopeless anterior residual teeth due to severe periodontitis. The patient struggled with the mobile devises, complaining of a continuous perception of “foreign body” in his mouth. The new request was for a complete fixed prosthetic rehabilitation, to be accomplished as fast as possible, with minimal suffering.
After taking a panoramic X-ray, the occlusion of the dentures was balanced to obtain a correct vertical dimension. “Double scan” method was adopted to plan the treatment. Dentures provided with radio-opaque tracing points had been scanned by a cone-beam CT first, and a second scan of the patient’s mouth while wearing the mobile devises was taken subsequently. The data of the two scans were then aligned thanks to the radiopaque points by dedicated software, rightly superimposing the clearer denture images of the first scan to those from the second one, representing the bone structures better.
Six implants were planned to be placed in the upper jaw, tilting the rear ones to avoid sinus lifts and to reach the first molar zone with the prosthesis, and five implants were planned to support a fixed structure in the mandible. After that, the prostheses were scanned with an intra-oral digital scanner, and the standard tessellation (STL) data about the superficial texture of the restorations were imported and matched with the DICOM data from the CT to realize the surgical guides for flap-less implant insertion in both the jaws.
The OT Bridge (Rhein83, Bologna, Italia) solution, particularly indicated to overcome the dis-alignment problem of the implants in the maxilla, was chosen to connect the implants to the superstructure, correcting more than 35° of the axial discrepancy between the frontal and the rear fixtures with respect to the occlusal plane. In maxilla, the anterior implants were flapless placed in canines/first premolars and lateral incisors position, and the rear tilted ones in second premolars/first molars position. In mandible, the implants were inserted in the first molars/second premolars, canines, and right first incisor position, The dimensions (4 mm × 12 mm) and the type of fixtures [Konic external hexagon, BTK®, Povolaro di Dueville (VI), Italia] were all the same. OT Equator abutments were connected to the fixtures with a 22–25 N·cm torque and the Extragrade abutments were joined. The low-profile semispherical attaches realize a subequatorial joint with the straight abutments carrying the Seeger ring in their internal correspondent surface. An abutment-implant connecting screw assured this “snap” coupling except for the rear fixtures, whose inclination would have hindered the screwing and unscrewing finger movements, particularly without a dedicated angled screwdriver. Once the Extragrades were embedded in the prefabricated provisional polymethyl-methacrylate (PMMA) restoration in the patient’s mouth without interferences (passivation), the superstructure was unscrewed from the four anterior implants and detached from the snap joint. Afterward, the prosthesis was reinforced with a metallic bar, relined, refined, and re-connected with the same modality. The rear implants remained unscrewed to the provisional device until the final restoration delivery was carried out three months later. Regarding the mandible, the five implants were intra-orally welded to each other and immediately loaded in the same surgical setting. The provisional restorations were delivered within 24 hours. Ibuprofen (800 mg, three times a day for the following three days, and then, as needed) was prescribed along with a soft diet and chlorhexidine mouthwashes. The patient reported minimal hematoma in the sub-mandibular area which completely resolved in seven post-surgical days, with few ecchymoses in the labial regions. The control checks were performed weekly in the first month after the immediate loading and every 15 days until the definitive prosthesis connection sitting, without any surgical or prosthetic criticism observation. After three months, a digital impression with an intraoral scanner was taken and a screw-retained zirconia restoration was delivered. Before screwing, the Seeger rings were placed between the subequatorial area of the OT Equators and the Extragrade framework connections. The prosthesis was screwed to all abutments at 20 N·cm torque and the occlusion was checked. The monitoring visits, monthly in the first year and three-monthly in the second one, for an overall period of two years from the surgical sitting, did not reveal any complication without radiological bone peri-implant resorption at periapical X-rays control. The case is shown in Figure 3.
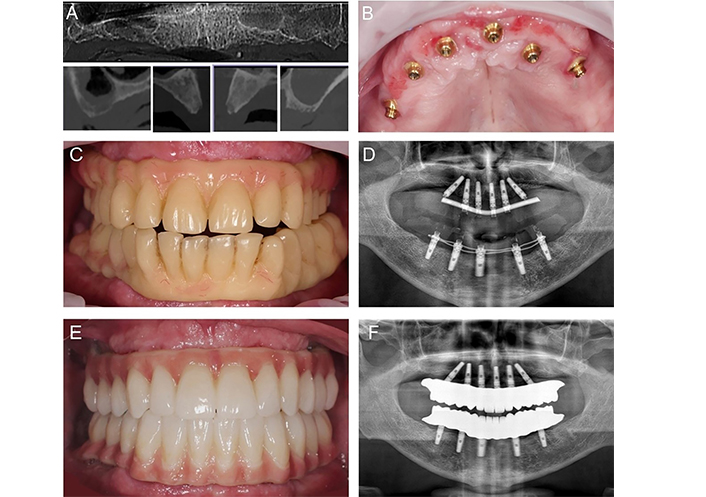
Clinical and radiological images of the reported case. Cone beam CT panorex and cross-sectional cuts show the expansion of the sinuses with signs of sinusitis and the bone availability in the pre-maxillary zone (A). Intra-operative scenario after the implant placement and their connection with the OT Bridge abutments (B). The provisional prostheses connected to the implants (C). Panoramic X-ray after the delivery of the provisional prostheses (D). Clinical situation at the two-year check (E). Radiographical situation at the two-year check (F)
The tilted ≥ 13 mm long implant option was proposed in 1999 to avoid reconstructive surgery [3]. The angled distal fixtures split the vertical and horizontal occlusal forces and allow a cantilever length reduction. The most-reported anteroposterior inclination is 30°/45°, with an overall range from 15° to 50° [4]. In the literature, it was ratified that a limit of 45° between vestibular inclined implants and the prosthesis plane did not compromise the normal upper lip function [2]. Such an approach is particularly advantageous in immediate loading, where a 30/35 N·cm minimum torque is required [13]. Static and dynamic digital surgical guidance allowed a more precise and flapless approach. Focusing on the edentulous maxilla with traditional loading, Fortin & Sullivan reported 44 successful cases with 10- to 19-year follow-up [5]. A cumulative 1-year survival rate of 97.9% was recorded in a systematic review with 48 hours of prosthetic connection after surgery [13].
A fixed screw-retained bridge, a fixed denture tooth with false gingiva, and a removable overdenture coupling with an implant-connected machined framework are the prosthetic options considering the aesthetic and hygienic demands and the need for soft tissue support [5]. A full-arch acrylic prosthesis with a metal framework was mainly used as a temporary implant-screw-retained device for immediate loading. No difference in marginal bone resorption between tilted and straight fixtures was reported in the literature when loaded immediately [7] or after 48 [6] and 72 hours [9]. The most common complications described in the literature are the fracture of the provisional prosthesis and connection-screw loss [4, 13].
The connection system between intra- and extra-osseous components is fundamental to the long-term success of tilted implants. The conical frictional joint appears superior to others in terms of loading support, does not need a connection screw, and the minimal micro-gaps at the implant/abutment connection decreases bacterial leakage. Nevertheless, a conical connection, depending on the contact between the two coupling surfaces, can tolerate only minimal grades of implant misalignment [14, 17]. The angled MUA system, transforming an internal connection to a low-profile external one, can compensate for up to 35° of axial implant divergence with the occlusal plane [16]. However, the limited coupling contact with the abutment and the reduced dimension of the retaining screws cause rotational tension under the no-axial loadings, with loss of the preload screwing force and subsequent fracture risk [15, 21]. Hence, the MUA must have a bulky shoulder and an average diameter of 4.8 mm, which reduces the occlusal space for the peri-implant soft tissues and the framework.
A new implant design with an inclined neck portion was developed to overcome angulation issues and the challenges of using intermediate abutments. The angled connection allows a correct prosthetic direction from the surgery phase. The restorative procedure appears simplified because the prosthesis can be connected directly to the implants with a better fitting and less fastening screw fractures or loosenings. Nevertheless, an increased rate of bone resorption, porcelain fractures, and mucositis were reported in cases of direct implant-prosthetic connection [21].
The OT Bridge system consents to exploit the advantages of the ball-retention attaches for implant-anchored overdentures in the fixed screw-retained prosthetic solutions. The OT Equator, with undercuts all around its axis, permits a coupling even with up to 80° tilted implant-abutment unit. The spheric shape of this attach allows the occlusal load to be distributed to the plastic ring of the female cap embedded in the overdenture, reducing the force concentration to the perimplant bone and soft tissues [28]. This low-profile abutment is adaptable to any fixtures’ platform. It allows the platform to be standardized even in the case where different types of implants have been inserted [29].
The straight profile of this joint is compatible with a 0.3 mm thicker screw in comparison with the MUA system, with 70% more stress resistance [11, 14, 26]. The particular design of the Seeger acetal ring housed in the Extragrade turret engages the undercuts of the OT Equator without limit of spatial orientation and assures a snap passive joint to the fixtures. This kind of engagement gives the prosthesis a first reliable anchorage, without hindering the subsequent allocation of the connecting screw. Furthermore, the Seeger works as a load absorber and reduces the stress around the fixture-abutment complex.
The use of straight abutments as the Extragrade component lowers the economic costs, and the OT Bridge system’s compatibility with all CAD/CAM systems makes it versatile for various philosophies of implant-supported rehabilitation.
The adopted joint simplified the reported treatment. Obtaining the first good stability of the provisional prosthesis, even without connecting the screws to the angled distal fixtures, allowed more rapid reline and adapt the temporary device in the patient’s mouth after the surgery. The definitive prosthesis was easily screwed to all the fixtures. The connection system used in the present case can favor a reduction from six to four of the implant number, as in the all-on-four protocol, which is still a debatable approach for upper jaw fixed rehabilitation.
Nevertheless, the OT Equator could be more prone to fracture in the undercuts after a long-term follow-up in fixed rehabilitation, particularly in case of implant misalignment, and the Seeger ring can lose its retention power for prolonged stress. A finite element method (FEM) study recorded no substantial variations in stress distribution without allocating one of the two anterior screws in a simulated all-on-four rehabilitation [25]. Pozzan et al. [26] did not observe in vitro any variations in the stress distribution or locking preload loss by removing up to two connecting screws in an all-on-four mandibular simulated rehabilitation. No in vitro studies focused on the mechanical properties of this joint in case of fixed rehabilitation, independently of the presence or not of the fastening screw.
Only a few clinical cases of fixed screw-retained prostheses were treated with the OT Bridge system with up to two years of loading, different anatomical situations, and angulation of the implants [11, 23, 24]. The presented case report aims to encourage the fulfillment of in vitro and in vivo predictable studies ratifying the use of snap-joint connections for fixed rehabilitation with and without the screw.
A totally edentulous atrophic maxilla was treated with the placement of six implants, with the rear ones tilted to reach the first molar zone with the superstructure. A particular sub-equatorial snap-joint system was adopted to cope with the axial discrepancy, more than 35°, between the frontal and the distal fixtures with respect to the occlusal plane. The provisional prosthesis was immediately connected. After three months, all implants were screwed to the final prosthesis. The patient was successfully monitored during a two year follow-up.
MUA: Multi-Unit Abutment
GP: Conceptualization, Data curation, Visualization. ZZ: Conceptualization, Resources, Supervision, Visualization. VC: Supervision, Visualization. GL: Writing—original draft, Writing—review & editing, Visualization.
The authors declare that there are no conflicts of interest.
The study was conducted in accordance with the Declaration of Helsinki. According to the local policy, ethical review is not applicable as preliminary cases report with a validated technique.
The informed consent to participate in the study was obtained from the participant.
Written informed consent has been obtained from the patient to participate and to anonymously report personal information showing radiographic and clinical images.
The data that support the findings of this study are not available yet in a public folder. Data are however available from Zoran Zaccheroni (zoranzac@libero.it) or Gerardo Pellegrino (gerardo.pellegrino2@unibo.it) upon request.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
© The Author(s) 2024.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1712
Download: 18
Times Cited: 0
Martina Costanzo ... Ilenia Campione
Zeina Darwich ... Chadi Azmeh
Francesca Gorassini ... Gabriele Cervino
Olha Denefil ... Natalia Tverdokhlib
Alberto Enrique Varela ... José E. Rodríguez
Aiswarya Polumatla ... Tejaswin Polepalle
Aya Dawoud Agha ... Moudar Bakkour
Alessia Pardo ... Massimo Albanese
