Affiliation:
1Department of Rheumatology, National Hospital Postgraduate Training & Medical Centre, Lahore 54000, Pakistan
Email: sumaira_farman@hotmail.com
ORCID: https://orcid.org/0009-0006-2345-3442
Affiliation:
2Arthritis Care Foundation, Lahore 54000, Pakistan
ORCID: https://orcid.org/0009-0008-2154-3799
Affiliation:
3Department of Paediatric Medicine, National University Hospital, NUHS Tower Block, Singapore 119228, Singapore
ORCID: https://orcid.org/0009-0000-2690-8779
Affiliation:
4Department of Paediatrics, Selayang Hospital, Ministry of Health, Selangor 68100, Malaysia
ORCID: https://orcid.org/0000-0003-1844-573X
Affiliation:
5Pediatric Rheumatology Group, Department of Paediatrics, Tehran University of Medical Sciences, Tehran 009821, Iran
ORCID: https://orcid.org/0000-0002-9711-7189
Affiliation:
6Department of Rheumatology, Shalamar Hospital, Shalamar Medical & Dental College, Lahore 54840, Pakistan
ORCID: https://orcid.org/0000-0003-3223-4787
Explor Musculoskeletal Dis. 2024;2:133–144 DOI: https://doi.org/10.37349/emd.2024.00042
Received: September 24, 2023 Accepted: November 28, 2023 Published: April 17, 2024
Academic Editor: Rebecca Grainger, University of Otago, New Zealand
The article belongs to the special issue Digital health technologies in rheumatology: emerging evidence and innovation
Aim: To evaluate the reach and potential effectiveness of teleteaching of health providers in paediatric rheumatology by observing the pattern of sessions, attendance, and attendees’ feedback in paediatric rheumatology teleteaching sessions across the Asia Pacific region. These were conducted by the Asia Pacific League of Associations for Rheumatology (APLAR) Paediatric Rheumatology Special Interest Group (Paeds Rheum SIG) as an APLAR academy activity.
Methods: A retrospective, descriptive analysis of electronic records of synchronous telehealth sessions held between July 2021 to July 2023. These followed three formats: case-based webinars, single topic modular online course, and a hybrid one-day short course. The topics of sessions, attendees’ registration details, specifically primary area of practice/specialty, geographic location, and their satisfaction as per feedback forms were noted.
Results: Case-based webinars had an average attendance of 200 per webinar: majority adult rheumatologists, paediatric rheumatologists (PRs), or paediatricians. The modular course consisted of nine sessions with an average of 63 participants per session. Specialties comprised PRs, adult rheumatologists with immunologists, and general paediatricians. The one-day hybrid course had over 600 attendees. Attendees were adult rheumatologists, general physicians, paediatricians, and PRs. Although the majority (79.3%) of attendees from these sessions were from APLAR member nation organisations (MNOs), a significant percentage (20.7%) were from non-APLAR MNOs and even non-Asia Pacific regions. The attendees’ feedback for all three formats showed a high level of satisfaction with case-based webinars being most favoured.
Conclusions: Teleteaching in paediatric rheumatology has the potential to fulfill the dire need for improved expertise of health professionals managing children with rheumatic diseases. Case-based, interactive sessions of shorter duration and a blended hybrid format may garner the most attendance and best learning outcomes.
Paediatric rheumatology providers care for a unique set of patients, whose diseases are usually complex in both diagnosis and management that require chronic care. Rheumatic disease burden exceeds access to treatment everywhere, regardless of wealth and geography [1]. Paediatric rheumatology care is critical as the general understanding of the global burden of rheumatic disease in the paediatric population is poor. There is a lack of guidelines for the diagnosis and management of rheumatic disease in resource-limited settings, despite the burden being felt even more keenly in middle-resource-income countries (MRIC) and low-resource-income countries (LRIC), where studies have demonstrated rheumatology care needs often remain unmet [1].
Increasing access to treatment is critically important, as paediatric rheumatic conditions increasingly contribute to the years of healthy life lost, or disability-adjusted life years (DALYs) globally for children [1]. The cost of undiagnosed and untreated paediatric rheumatic disease is several fold: the individual child’s pain and suffering, the impact on the caregivers and family, the cost to the healthcare system, and the lost earnings and economic contribution [1].
Based on recent data from the World Bank, the total world population of children aged 0–14 currently stands at 2 billion [2]. Recent prevalence numbers of 2,500–3,000 cases/million children give us approximately 5–6 million children affected with rheumatic diseases, whereby 78% live in Asia and Africa [3]. Juvenile idiopathic arthritis (JIA) is the most prevalent paediatric rheumatic disease and a leading cause of acquired non-traumatic musculoskeletal disability [4]. The frequency of mimicking conditions, the lack of a specific diagnostic test, and confusion with adult diagnostic patterns and criteria complicate the diagnosis of JIA and delay access to care, even in the most well-resourced health care systems [4]. World-wide population-based estimates indicate that there are 2–4 million children suffering with JIA [5].
The average minimum acceptable density of paediatric rheumatologists (PRs) in the developed world is 1:500,000 [3]. The current available international PR workforce is only 12% of this standard, with 40% based in the USA leaving only one PR for every 26 million children in Asia [3].
Asia Pacific League of Associations for Rheumatology (APLAR) has 33 official member nation organisations (MNOs), spanning half the globe, from the middle east (e.g., Jordan and Syria) all the way to Australia, and-north to south-from Kazakhstan and Mongolia to New Zealand. Asia Pacific is a vast, diverse region, with a sizable burden of rheumatic diseases, which affects the quality of life of patients and consumes healthcare resources. The prevalence of rheumatic diseases in Asia Pacific compared with North America and Europe is relatively lower, but given the large populations, this translates to a huge burden in the region [6].
These MNOs have a wide spectrum of economies ranging from low to high income. Data shows that least developed countries have the highest projected birth rate translating to the highest young population (Figure 1) [7]. Additionally, countries with low human development indices (HDIs) and low gross domestic product (GDP) have the highest percentage of young population, and lowest public health spending [8–10], and as per a 2021 Special Interest Group (SIG) survey the most critical shortages of PRs! Barriers to developing and providing paediatric rheumatology specialised multidisciplinary services across Asia Pacific are many and include absent or inadequate specialists and allied health professionals. However, paediatric rheumatology training is fraught with many challenges including the lack of a critical mass of specialist PRs in the first place [11]. The dilemma of what comes first, a chicken or an egg, is classically demonstrated here!
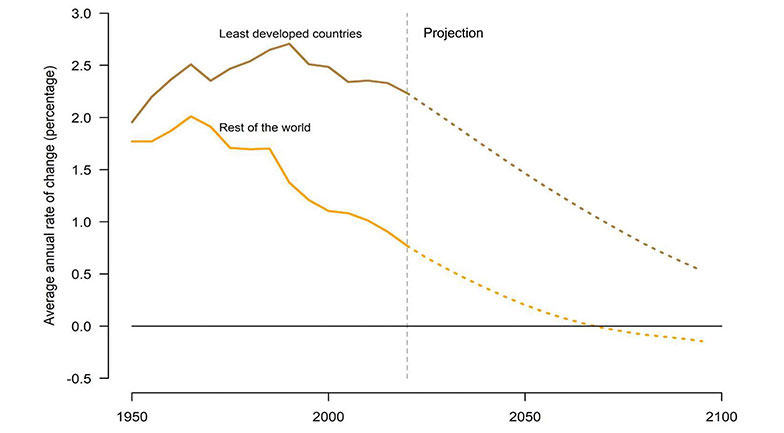
The total population of the least developed countries is growing at a rate that is 2.5 times faster than the growth rate of the total population of the rest of the world
Note. Adapted from “World population prospects 2019: highlights [Internet],” by United Nations, Department of Economic and Social Affairs, Population Division. United Nations; c2019 [cited 2023 Sep 18]. Available from: https://population.un.org/wpp2019/Publications/Files/WPP2019_Highlights.pdf. CC BY 3.0 IGO.
As a result, adult rheumatologists, paediatricians, general physicians, etc. are compelled to treat these children without adequate access to educational/training materials [11–13]. The need for a collaborative regional effort to overcome the severe shortage of paediatric rheumatology services was recognized, and the APLAR Paediatric Rheumatology SIG (Paeds Rheum SIG) was approved during the annual APLAR congress held in Brisbane, Australia in 2019.
The first mandate given to the SIG was an education of patients, and physicians and continued professional development of rheumatologists in the region. However, the 2021 SIG survey with 18/33 MNO responses revealed the availability of only 20 training programs clustered in 13 countries. The practical barriers of travel, cost, and adequate availability of formal training opportunities preclude “conventional structured training” for all involved in the health care of children with rheumatic diseases.
Teleteaching educational sessions may thus be an effective alternative to conventional training in improving expertise in paediatric rheumatic diseases. A recent study conducted in Pakistan to evaluate the pros and cons of online distance learning for medical students had very positive feedback favouring online learning modalities [14]. Another 2019 meta-analysis indicated that webinars were positively associated with gains in knowledge and skills thus making this an attractive option for effective online education [15].
The experience of synchronous teleteaching sessions in three formats, viz., case-based webinars, modular single-topic course, and a short one-day hybrid review course, conducted by the APLAR Paeds Rheum SIG, is presented here.
This is a retrospective, descriptive study that was done through the analysis of electronic records of synchronous teleteaching sessions held between July 2021 to July 2023. These followed three formats: case-based webinars, single topic modular online course, and a hybrid one-day short course. The topics of sessions, attendees’ registration details, specifically primary area of practice/specialty, geographic location, and their satisfaction as per feedback forms were noted.
From July 2021 to July 2023, the webinar committee of the APLAR Paeds Rheum SIG organized seven webinars, scheduled every 3–4 months. Data from five webinars spanning 2022–2023 was analyzed. Due to logistical constraints during the coronavirus disease 2019 (COVID-19) lockdown period, the first two webinars were hosted by an independent platform which did not have a feedback mechanism in place.
Each webinar consisted of two case presentations from two different countries within APLAR, each case lasting 45 min, including time for discussion and questions. Topics included JIA, vasculitides, macrophage activation syndrome (MAS), multi-system inflammatory syndrome in children (MIS-C), juvenile dermatomyositis, uveitis, chronic non-bacterial osteitis, autoimmune cytopenias, recurrent pericarditis, and autoinflammatory conditions.
This course comprised nine modules or sessions, each one to two hours, held from December 2021 to April 2022. The topics covered in the nine sessions were the following: a clinical approach to systemic autoinflammatory disorders; approach to patients with periodic fever, aphthous stomatitis, pharyngitis, adenitis (PFAPA); network developments for autoinflammatory disorders and patient education; NOD-like receptor proteins 3 (NLRP3)-from autoinflammation to metaflammation; the role of type 1 interferons as trigger of cytokine storm in MAS; interferonopathies with a special aspect on rare proteasomopathies viz., chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE)/proteasome-associated autoinflammatory syndromes (PRAAS); overlapping features of systemic JIA and autoinflammatory disorders.
Attendees had to correctly answer at least 80% of the questions posed post webinar to be eligible for the certificates endorsed by the APLAR academy.
This was held in conjunction with the annual conference of an APLAR MNO, the Pakistan Society for Rheumatology (PSR). It was hybrid, with online faculty from across the Asia Pacific region viz., Australia, India, Malaysia, Singapore, and on-site from Pakistan and the USA. The course focused on various childhood onset rheumatic diseases with interactive case-based sessions, paediatric Gait, Arms, Legs, and Spine (pGALS), and an extended rheumatological examination.
The topics were (1) when to think of a rheumatological disease in kids; (2) childhood onset lupus (cLupus): a unique population; (3) cLupus emergencies; (4) managing cLupus: latest guidelines; (5) JIA presentation, differentials & latest treatment guidelines; (6) skin manifestations of primary vasculitis in children.
There were over 500 registrants for each webinar in 2022, decreasing to 350–450 in 2023. The actual number of attendees, however, remained fairly constant at around 180–220 per webinar for all seven of the webinars.
Majority of the attendees came from APLAR MNOs, whilst approximately 15% came from non-MNO nations viz., Afghanistan, Bhutan, Brazil, Cambodia, Egypt, France, Georgia, Ireland, Italy, Kenya, Nigeria, Portugal, Romania, Trinidad, Tobago, Turkey, the United Kingdom, USA, West Sahara, and Yemen.
The attendees comprised a wide range of healthcare providers: the majority (38.7%) identifying as adult internists or paediatricians, followed by PRs (26.0%, trained or in training) and adult rheumatologists (26.0%). Other registrants came from fields of nursing, allied health (occupational or physical therapy), general practice, and other subspecialties (Figure 2). This is consistent with existing data that suggests that in most parts of the region, paediatric rheumatology patients are being cared for by doctors who have not undergone specific training for this subspecialty [9–11]. Therefore, the first part of each case presentation highlighted a comprehensive approach to the clinical problem at hand, rather than focusing on management alone. In addition, speakers also spent time highlighting the differences between children and adults with respect to the disease in question.
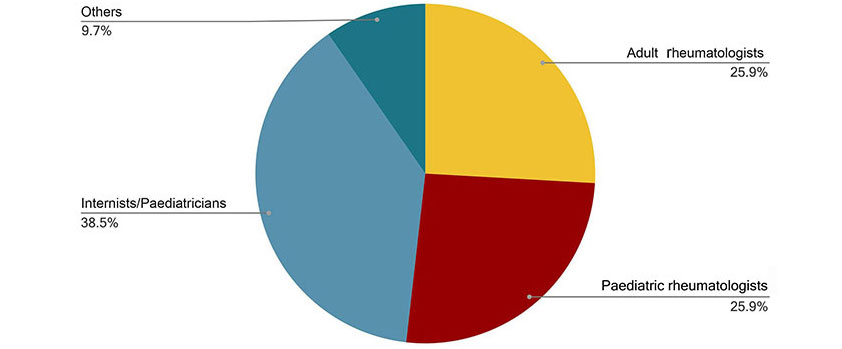
Average attendee speciality distribution for 5 out of the 7 Paeds Rheum SIG webinars. Number of participants: 200
Information about the events was disseminated via email, with notices on the APLAR and, where available, MNOs’ social media platforms (e.g., Facebook and YouTube).
Post-webinar feedback demonstrated extremely high levels of satisfaction with an average of 93.5% of respondents indicating scores of 4–5 on a 5-point Likert scale (0 was “very unsatisfied” and 5 was “very satisfied”). In addition, an average of 88.7% found the webinars highly relevant and helpful for their day-to-day practice.
In 2023, a post-webinar questionnaire was included, in response to participants’ feedback and requests for certificates of attendance, which seems to reflect the importance and value of the webinars to the receiving audience. Attendees who scored 75% and above were emailed certificates of attendance and achievement.
A less measurable but no less valuable result of these webinars was the coming together of paediatric rheumatology providers in the region, fostering familiarity and friendship. A positive effect of this is beginning to be seen in upcoming proposed collaborations for education and research.
The mean number of participants in each of the nine sessions was 63; the majority (36.4%) identified as PRs, followed by adult rheumatologists (20.3%), immunologists (10.1%), and general paediatricians (8.9%). A small number also came from the fields of internal medicine, general physician, haematology/oncology (approximately 4% each), and other subspecialties (1% or less) (Figure 3).
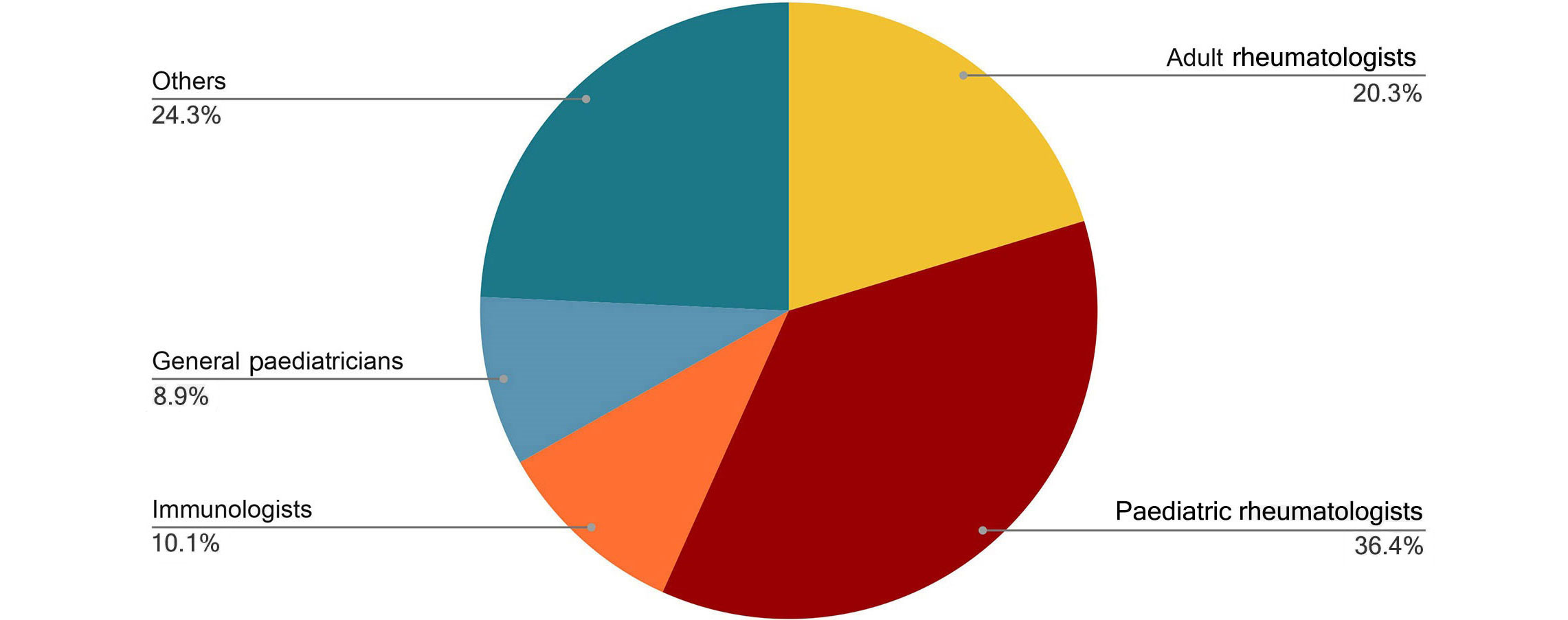
Attendee specialty distribution for the single topic course on autoinflammatory diseases. Number of participants: 63
Ninety-five percent of the attendees came from the APLAR MNOs with 70% of the total coming from the host country, Iran. Less than 5% were from non-MNO countries viz., the USA, United Kingdom, France, Canada, Nigeria, Brazil, Burundi, and Mongolia.
The feedback was impressively positive regarding the speakers’ knowledge, presentation skills, up-to-date material, interactive question answer sessions with the audience, and time management. The audience conveyed a preference for case-based discussions rather than non-case-based sessions.
A total of 616 participants attended the course. Two hundred and three (32.95 %) of these participants provided their country of residence, with 161 (79.3%) from APLAR MNO countries while 42 (20.7%) were from non-MNO countries. Out of the 161 attendees from MNO countries, 41 (25.5%) were from Pakistan, the host country (Figure 4), suggesting a substantial number to fall into online participants.
Only 150 participants gave their specialty (Figure 5). This is less than 25% of the participants and cannot be considered true representation. However, it does suggest that other than PRs a significant number of adult rheumatologists participated. The number and wide geographical location of attendees also reflects the need, scope, and potential of such an activity. Nearly all of the attendees (93.2%) found the course very useful and agreed that the activity improved understanding of the subject matter.
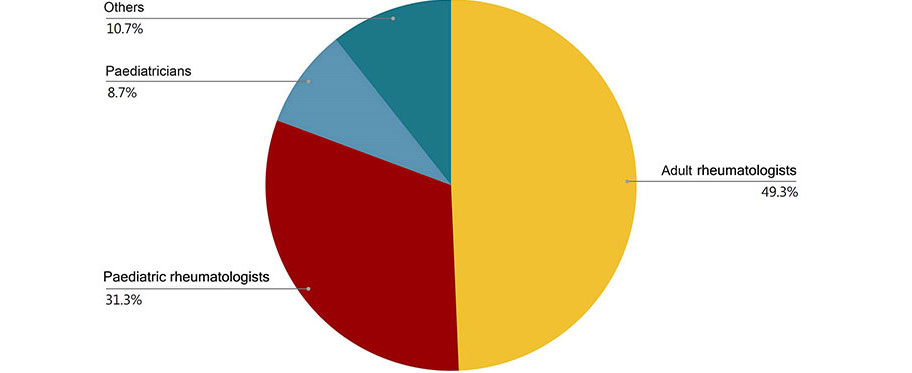
Attendee specialty distribution for a short one-day hybrid course. Number of participants: 150
We present data from synchronous teleteaching sessions in paediatric rheumatology conducted in three different formats: case-based webinars; modular course; and hybrid course.
Virtual online courses in paediatric rheumatology are scarce and apart from the European League Against Rheumatism (EULAR) course, they remain relatively unknown. The EULAR course is modular and comprehensive suitable for paediatricians and adult rheumatologists. However, its content may not be completely applicable to the diverse population and economic settings within the Asia Pacific region. Additionally, it is a paid course which may restrict accessibility for health professionals from LRIC.
Another example of a virtual learning resource is paediatric musculoskeletal matters (PMM). It has been developed for better recognition of rheumatic diseases by general practitioners and allied health workers [16, 17]. It is free access and provides information through training materials such as modules, images, and videos. Both the EULAR course and PMM use asynchronous methods of online learning.
A comparison of asynchronous and synchronous methods of an online course in medical laboratory technology showed significant preference by the majority of students in favour of a synchronous method for greater clarity of understanding of concepts and confidence in the ability to solve examination questions [18].
In this regard, the APLAR Paeds Rheum SIG initiated synchronous teleteaching sessions in three formats: a series of case-based webinars, a single topic modular course, and a short one-day hybrid course.
The webinars were conducted 2–3 times per year. The aims of these webinars were: education through the sharing of clinical cases, with special consideration for the unique socio-cultural, geographical, and resource variations in the Asia Pacific region and the creation of a shared space where relevant healthcare providers for paediatric rheumatology patients in the Asia Pacific viz., adult rheumatologists, paediatricians, general physicians, etc. could network, share clinical experience, and learn from each other.
The nine-session course on autoinflammatory diseases was held in collaboration with the Paediatric Rheumatology Society of Iran and the short one-day hybrid review course was held in collaboration with the annual conference of the PSR.
The current shortage of PRs and trainers in paediatric rheumatology in the Asia Pacific cannot be overemphasised and thus, human resource development and training in paediatric rheumatology for health professionals managing children with rheumatic diseases is of utmost importance. According to the “average minimum acceptable requirement” of PRs in the West, for the 33 APLAR member nations, we need more than 3,000, while the actual number as estimated by the SIG survey is estimated around 300 only (Figure 6).
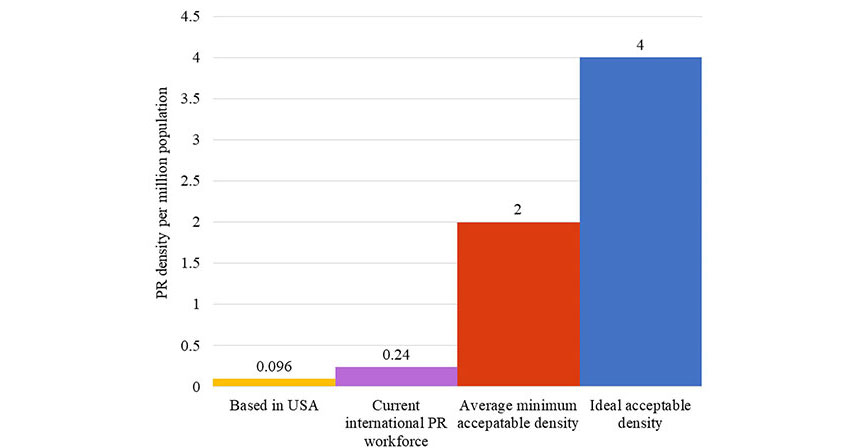
PR density per million population: current vs. minimum requirement vs. ideal requirement
In most cases, rheumatology providers are localised in major centers, which creates disparities even in countries whereby there are trained rheumatologists. Training opportunities for paediatrics or paediatric subspecialties are also quite limited in many LRIC, especially in Africa, whereby only one country has PR training available [4]. In places with large paediatric populations and general workforce shortages, sub-specialists cover general paediatrics (Figure 7).
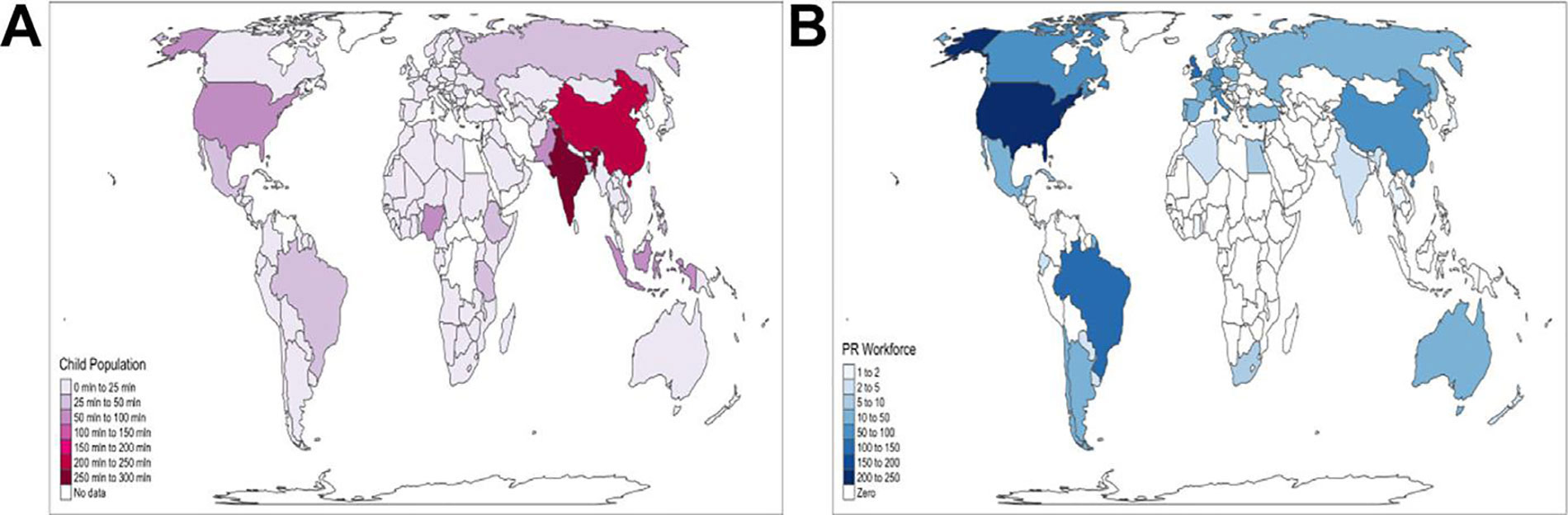
Mapping the world paediatric rheumatology workforce and the world paediatric population. A. The number of children ages 0–14 in each country. The map demonstrates that much of the world’s paediatric population resides in LRIC, particularly sub-Saharan Africa, South Asia, and Southeast Asia; B. the global distribution of the paediatric rheumatology workforce is concentrated in North America and Europe, largely in HRIC [4]
Note. Reprinted with promission from “Pediatric rheumatic disease in lower to middle-income countries: impact of global disparities, ancestral diversity, and the path forward,” by Scott C, Sawhney S, Lewandowski LB. Rheum Dis Clin North Am. 2022;48:199–215 (https://www.rheumatic.theclinics.com/article/S0889-857X(21)01126-1/abstract). © 2024 Elsevier Inc., its licensors, and contributors.
This abysmal state of paediatric rheumatology is reflected by the survey on the paediatric rheumatology workforce in Australia and New Zealand conducted in 2016 by the Australian Paediatric Rheumatology Group (APRG) which found that there was a shortfall in the paediatric rheumatology workforce of 68% based on minimum requirements and a shortfall of 225% based on an ideal scenario [16]. Furthermore, more than 40% of children did not have easy access to multidisciplinary team care which is essential in the care of these patients [19].
It has also been shown that Australia has significant delay from symptom onset to diagnosis of JIA, presumably due to a lack of education of non-rheumatology health professionals about paediatric rheumatology diseases. The most effective intervention would be the education of general medical staff to improve recognition of rheumatic disease and reduce delays in diagnosis [19].
The findings of this survey are even more significant as amongst the APLAR MNOs both Australia and New Zealand have high HDIs and GDP [8–10] with three training centers in Australia of the 20 identified among the APLAR MNOs in the 2021 SIG survey. We can assume the situation to be much worse in other Asia Pacific regions, especially the LRIC. Even in a country like the USA with the greatest density of PRs globally [3], internist rheumatologists are still more geographically diffuse than PRs and act as substitutes for them in regions that lack such providers [20]. This current gap is likely to worsen, with the projected demand to increase to almost twice the supply by 2030 [21].
Strengthening the education of paediatricians and general practitioners to recognize paediatric rheumatic diseases and refer for further care is an essential step especially in countries with few providers [22]. Targeted innovative interventions are needed for training a health care force for early recognition and appropriate management of these conditions.
We have seen that shorter in-person training can be supplemented with an online, asynchronous curriculum [23]. The one-year online graduate certificate of paediatric rheumatology University of Western Australia (UWA) earned an award in teaching innovation [24]. The COVID-19 global pandemic accelerated the development of virtual medical education and training; LRIC without access to PRs with no possibility of a local training program can, and should, leverage this new approach [25–28].
Research has demonstrated that asynchronous and synchronous support different purposes and complement each other [29]. Data analysis suggests that neither approach alone is sufficient; instead, a blended approach is required, with the possibility of blended learning to include blending of asynchronous and synchronous online modes [30]. This leads us to recommend the development of an online blended paediatric rheumatology training program with a hybrid short duration on-site training component.
In summary, the available data shows a huge gap between supply and demand for paediatric rheumatology providers. Additionally, there is a severe shortage of trainers and training sites to fill the gap. Teleteaching in paediatric rheumatology has the potential to fulfill the dire need for improved expertise of health professionals managing children with rheumatic diseases. It may be an effective alternative to conventional structured paediatric rheumatology training till such time when formal training is made more available and accessible. This article highlights this potential reflected by the numbers of attendees, the varied mix of their specialty and geographic location, and the positive feedback. Case-based, interactive sessions of shorter duration and a blended hybrid format may garner the most attendance and best learning outcomes. We strongly believe that any initiative taken would not only impact APLAR MNOs, but the whole region as well. The APLAR Paeds Rheum SIG hopes to take the lead in this endeavour.
APLAR: Asia Pacific League of Associations for Rheumatology
cLupus: childhood onset lupus
EULAR: European League Against Rheumatism
JIA: juvenile idiopathic arthritis
LRIC: low-resource-income countries
MNOs: member nation organisations
Paeds Rheum SIG: Paediatric Rheumatology Special Interest Group
PRs: paediatric rheumatologists
SIG: Special Interest Group
SF: Conceptualization, Data curation, Methodology, Supervision, Writing—review & editing, Writing—original draft. MKHR and EYA: Data curation, Formal analysis, Writing—original draft, Writing—review & editing. SPT: Writing—review & editing. KAA: Data curation, Writing—review. SEAK: Data curation.
The authors declare that they have no conflicts of interest.
Not applicable.
Informed consent to participate in the study was obtained from all participants.
Not applicable.
All datasets generated for this study are included in the manuscript.
Not applicable.
© The Author(s) 2024.
Open Exploration maintains a neutral stance regarding jurisdictional claims in published maps and institutional affiliations.
Copyright: © The Author(s) 2024. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Hannah Labinsky ... Johannes Knitza
Prakashini Mruthyunjaya ... Debashish Danda
Michael Schirmer ... Johannes D. Pallua
Diego Benavent ... Antonio Gómez-Centeno
Carlos A. Guillén-Astete ... Mónica Vázquez-Díaz
Judy L. Seraphine, Alvin F. Wells
