Abstract
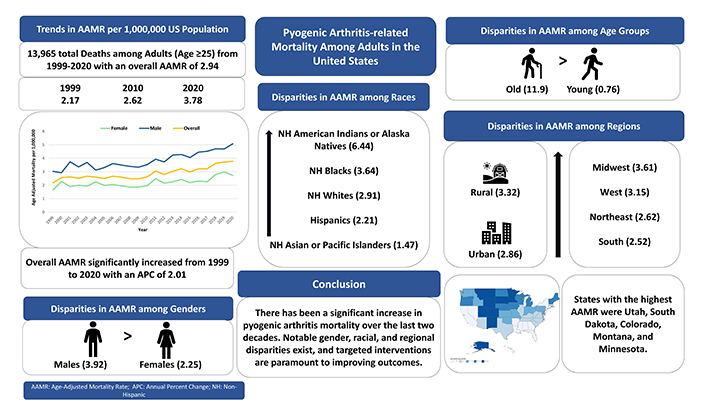
Pyogenic arthritis (PA) related mortality trends have not been studied well across various demographics in the United States (US). This cross-sectional study aimed to evaluate these trends among the US population aged ≥ 25 years from 1999–2020 using data from the CDC WONDER database. We identified all the deaths where PA was listed as the underlying or contributing cause of death, using the ICD-10 code M00. Age-adjusted mortality rates (AAMRs) were calculated per 1 million US population and the Joinpoint regression model was used to assess the annual mortality trends by calculating the annual percent change (APC) in AAMRs. Between 1999 and 2020, 13,965 total deaths occurred among US adults aged ≥ 25 years with an AAMR of 2.94. The overall AAMR of PA increased significantly from 1999 to 2020 with an APC of 2.01 (p < 0.01). Males and older adults had consistently higher AAMRs than their respective counterparts. Non-Hispanic (NH) American Indians/Alaska Natives and NH Blacks/African Americans had higher mortality rates compared with other racial groups. The Midwest had the highest overall AAMR, followed by the West, Northeast, and South regions. In conclusion, PA mortality has been on the rise and targeted interventions are warranted to reduce disproportionate mortality rates among vulnerable populations.
Keywords
Pyogenic arthritis, mortality, trends, disparitiesPyogenic arthritis (PA), also known as septic arthritis, is a severe joint infection caused by the invasion of pyogenic bacteria, leading to inflammation, joint pain, swelling, and potential joint destruction if not promptly treated [2]. Despite advances in medical care, the burden of this condition remains a critical public health concern. The literature reports a mortality rate for PA ranging from 4% to 42%, with values as high as 50% in cases of polyarticular condition [3]. However, there exists a gap in the literature regarding PA-related mortality burden and temporal mortality trends among various demographic and regional groups. In this study, we aim to bridge this gap by using data from a large national database of mortality figures in the United States (US) and provide valuable insights for policymakers to improve patient outcomes and inform future research.
In this cross-sectional study, we analyzed the annual mortality trends related to PA in adults aged ≥ 25 years in the US from 1999 to 2020 using data from the Centers for Disease Control and Prevention’s Wide‐Ranging Online Data for Epidemiologic Research (CDC WONDER) database [4]. This database captures data for all fatalities in the US. We identified all the cases where PA was listed as an underlying or contributing cause of death using the International Classification of Diseases, Tenth Revision (ICD-10) code M00. Age‐adjusted mortality rates (AAMR) were calculated per 1 million US population by standardizing crude mortality rates to the 2000 US census population. The Joinpoint regression program version 4.9.0.0 (National Cancer Institute) was used to evaluate any increase or decrease in AAMR from 1999–2020 by calculating annual percent change (APC) in the AAMR and corresponding 95% confidence interval (CI). The Joinpoint software applies permutation testing to identify whether observed changes in AAMR are statistically significant, taking into account the sample size and variability in the data. A change in AAMR over a time segment was considered statistically significant with a p-value < 0.05. Since the data is completely de-identified and publicly available, approval from the institutional review board was not required.
Between 1999 and 2020, a total of 13,965 PA-related deaths occurred among US adults aged ≥ 25 years, with an overall AAMR of 2.94/1 million population (Table 1). The overall AAMR of PA increased significantly from 2.17 in 1999 to 3.78 in 2020 with an APC of 2.01 (95% CI: 1.26 to 2.77; p < 0.01). Around 55% of the deaths occurred in males, and their AAMRs remained higher than that of females throughout the study duration (cumulative AAMR: 3.92 vs 2.25, respectively). Both the males (APC: 2.07; 95% CI: 1.23–2.92; p < 0.01) and females (APC: 1.65; 95% CI: 0.28–3.04; p < 0.02) showed a significantly increasing mortality trend over the study duration (Graphical abstract).
Age-adjusted mortality rates (AAMR) for pyogenic arthritis among adults aged ≥ 25 years in the United States from 1999 to 2020
| Year | Deaths | Population | AAMR | 95% CI |
|---|---|---|---|---|
| 1999 | 385 | 180,408,769 | 2.17 | 1.96–2.39 |
| 2000 | 458 | 181,984,640 | 2.56 | 2.33–2.80 |
| 2001 | 478 | 184,305,128 | 2.62 | 2.39–2.86 |
| 2002 | 464 | 186,208,028 | 2.52 | 2.29–2.75 |
| 2003 | 500 | 188,090,429 | 2.67 | 2.44–2.91 |
| 2004 | 494 | 190,205,384 | 2.60 | 2.37–2.83 |
| 2005 | 492 | 192,551,384 | 2.50 | 2.28–2.72 |
| 2006 | 531 | 195,019,359 | 2.67 | 2.44–2.90 |
| 2007 | 526 | 197,403,777 | 2.60 | 2.37–2.82 |
| 2008 | 516 | 199,795,090 | 2.48 | 2.26–2.90 |
| 2009 | 522 | 202,107,016 | 2.48 | 2.27–2.70 |
| 2010 | 563 | 203,891,983 | 2.62 | 2.40–2.84 |
| 2011 | 681 | 206,592,936 | 3.05 | 2.82–3.28 |
| 2012 | 631 | 208,826,037 | 2.80 | 2.58–3.02 |
| 2013 | 714 | 211,085,314 | 3.04 | 2.81–3.26 |
| 2014 | 759 | 213,809,280 | 3.22 | 2.99–3.45 |
| 2015 | 722 | 216,553,817 | 2.99 | 2.77–3.21 |
| 2016 | 787 | 218,641,417 | 3.22 | 2.99–3.44 |
| 2017 | 813 | 221,447,331 | 3.22 | 2.99–3.44 |
| 2018 | 940 | 223,311,190 | 3.62 | 3.39–3.86 |
| 2019 | 982 | 224,981,167 | 3.72 | 3.48–3.95 |
| 2020 | 1,007 | 226,635,013 | 3.78 | 3.54–4.01 |
| Total | 13,965 | 4,473,854,489 | 2.94 | 2.89–2.99 |
Stratified analysis based on race/ethnicity revealed that non‐Hispanic (NH) American Indians or Alaska Natives had the highest cumulative AAMR (6.44) followed by NH Blacks or African Americans (3.64), NH Whites (2.91), Hispanics or Latinos (2.21), and NH Asians or Pacific Islanders (1.47). Analysis based on age groups revealed that older adults (65 years and above) contributed to 78% of deaths and had much higher cumulative AAMR than younger adults aged 25–64 years (11.93 vs 0.76, respectively). Rural areas had higher cumulative AAMR than urban areas (3.32 vs 2.86). AAMR also varied substantially across different states, ranging from 6.21 in Utah to 1.68 in Florida. The states with the highest AAMR were Utah, South Dakota, Colorado, Montana, and Minnesota. When stratified by the census region, the Midwest region showed the highest cumulative AAMR (3.61) followed by the West (3.15), Northeast (2.62), and South (2.52) regions.
Our study, using data from a large, reputable database, highlights the following important findings: (1) PA-related mortality has significantly increased among US adults aged ≥ 25 years over the last 22 years. (2) Males had higher mortality rates than females and older adults had higher mortality rates than younger adults. (3) NH American Indians or Alaska natives had higher mortality rates, followed by NH Blacks or African Americans, NH Whites, Hispanics or Latinos, and NH Asians or Pacific Islanders.
There could be many potential reasons behind the concerning increase in PA-related mortality in the US over the last 2 decades. Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most common causes of adult-onset PA [5]. Studies have shown a significant rise in MRSA resistance to antibiotics such as tetracycline (from 3.6% in 2010 to 12.8% in 2019), trimethoprim-sulfamethoxazole (from 2.6% in 2010 to 9.2% in 2019), and clindamycin (from 16% in 2005 to 17% in 2014) [5, 6]. This increasing resistance may result in more severe, difficult-to-treat infections, potentially contributing to higher mortality rates. Moreover, the proportion of individuals over 50 years old in the US has risen from 27.1% in 1999 to 35.7% in 2020 [7]. Furthermore, there has been a marked increase in comorbidities such as diabetes (from 15.9% in 1999 to 29.2% in 2020) and obesity (from 30.5% in 1999 to 42.8% in 2018) within this aging population [8–11]. Older individuals often have a diminished immune response compared to younger individuals, and the presence of comorbidities such as diabetes and obesity further impairs the body’s ability to combat infections, leading to more severe complications like sepsis. Additionally, the combination of advanced age, obesity, and diabetes increases the risk of cardiovascular disease and chronic kidney disease, complicating the management of conditions such as pyogenic arthritis. These factors can also lead to mobility challenges and social isolation, which may create barriers to accessing healthcare, resulting in delays in treatment and eventually increased mortality.
Disparities in healthcare access and socioeconomic factors among different racial and regional groups likely contribute to the elevated risk of mortality from PA in certain populations [12, 13]. In our study, the highest mortality rates were observed among NH American Indians/Alaska Natives, followed by NH Blacks/African Americans. Racial inequality may explain these findings, as studies have shown that hospitals serving predominantly African American and American Indian communities receive less funding compared to others, which can impact the quality of care provided to these populations [14, 15]. Additionally, lower financial stability and limited access to health insurance among American Indians likely exacerbate healthcare disparities and negatively affect outcomes [16, 17]. Given the significant increase in the American Indian population (from 12.2% in 1999 to 18.7% in 2020), racial disparities in healthcare access and quality may also account for the overall rise in AAMR observed in our study [7].
Addressing the rising PA mortality trend requires a multifaceted approach, including improving early diagnosis and treatment, improving antibiotic stewardship to combat resistance, promoting patient education on infection prevention, and investing in research for novel therapies. To reduce disparities in PA mortality highlighted in our study, strategies should focus on improving access to healthcare in underserved communities and racial groups, increasing awareness of PA risks among high-risk populations, enhancing cultural competency in healthcare delivery, and ensuring equitable distribution of resources. Further research should explore the exact underlying causes of these disparities and the effectiveness of specific interventions to reduce PA mortality.
The results of this study should be approached with caution, given several inherent limitations. Firstly, the cross-sectional design and the unavailability of more detailed data limited our ability to conduct a thorough multivariable-adjusted analysis to fully explain the disparities identified. The database lacks critical individual-level information, such as socioeconomic status, comorbidity profiles, disease duration, and specific medical treatments, all of which are important confounding factors that influence mortality outcomes. Second, reliance on death certificate data introduces potential inaccuracies in cause-of-death assessments due to possible reporting errors. Moreover, our analysis was exploratory and no adjustments for multiplicity were made across the comparisons in our Joinpoint regression model. Future studies may consider multiplicity adjustments to provide a more rigorous estimate of significance. Finally, we did not set a predetermined AAMR increase as clinically meaningful, as there is currently no established consensus on what AAMR increase constitutes a clinically significant increase in PA-related mortality. Further research is needed to determine the clinical significance of the observed increase in PA-related mortality over the last two decades. Consequently, while our findings offer valuable insights, they should primarily be viewed as hypothesis-generating rather than conclusive.
In conclusion, our study demonstrates significantly increasing PA mortality among adults in the US, with males, NH American Indians/Alaska Natives, older adults, and residents of rural areas being the high-risk subgroups. Effective public health strategies are needed to mitigate this increasing mortality burden.
Abbreviations
| AAMRs: | age-adjusted mortality rate |
| APC: | annual percent change |
| CI: | confidence interval |
| MRSA: | methicillin-resistant Staphylococcus aureus |
| NH: | non-Hispanic |
| PA: | pyogenic arthritis |
| US: | United States |
Declarations
Author contributions
UQ: Conceptualization, Methodology, Investigation, Formal analysis, Writing—original draft, Writing—review & editing, Supervision. MA: Conceptualization, Methodology, Investigation, Formal analysis, Writing—original draft. FN and EM: Investigation, Formal analysis, Writing—original draft.
Conflicts of interest
The authors declare they have no conflicts of interest.
Ethical approval
Due to the de-identified nature of the dataset, the need for ethical approval is waived by the Institutional Review Board.
Consent to participate
Due to the de-identified nature of the dataset, the need for informed consent is waived by the Institutional Review Board.
Consent to publication
Not applicable.
Availability of data and materials
The data used for this study are publicly available at no cost. The data not shown, which support the findings of this study, are available from the corresponding author upon reasonable request.
Funding
Not applicable.
Copyright
© The Author(s) 2025.
Publisher’s note
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.